Abstract
Summary
The aim of the current study was to use a Bayesian network meta-analysis to evaluate the relative benefits and risks of balloon kyphoplasty (BK), percutaneous vertebroplasty (PVP), and non-surgical treatment (NST) for patients with osteoporotic vertebral compression fractures (OVCFs). The results demonstrate that for pain and functional status, PVP was significantly better than NST, while the three treatments did not significantly differ in other outcomes.
Introduction
BK, PVP, and NST are widely used to treat OVCFs, but preferable treatment is unknown. The aim of the current study was to use a Bayesian network meta-analysis to evaluate the relative benefits and risks of BK, PVP, and NST for patients with OVCFs.
Methods
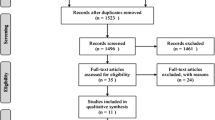
PubMed, EMBASE, and the Cochrane Library were screened. Based on the preplanned eligibility criteria, we screened and included randomized controlled trials that compared BK, PVP, and NST in treating patients with OVCFs. The risk of bias for individual studies was appraised. The data were pooled using a Bayesian network meta-analysis and a traditional direct comparison meta-analysis.
Results
Of the 1057 relevant studies, 15 were eligible and included. Compared with NST, PVP significantly reduced pain, Oswestry Disability Index (ODI), and Roland–Morris Disability Questionnaire (RMDQ). The comparative efficacy of BK and PVP was similar for pain (mean difference (MD) 0.51, 95% credible interval (CrI) − 0.35 to 1.4), ODI (MD 0.11, 95% CrI − 13 to 13), and RMDQ (MD 1.2, 95% CrI − 2.7 to 5.4). The European Quality of Life–5 Dimensions (EQ–5D) and Physical Component Summary subscales of the Medical Outcomes Study 36-Item Short-Form General Health Survey (SF-36 PCS) did not differ significantly. There were also no substantial differences in the risks of subsequent vertebral fractures, adjacent vertebral fractures, and re-fractures at the treated level across all comparators. The results of pairwise meta-analyses were almost consistent with those of network meta-analyses. The treatment ranking indicated that PVP had the highest probability of being the most effective for pain, ODI, RMDQ, and EQ-5D. BK had the highest probability of improving SF-36 PCS and of reducing the risk of subsequent vertebral fractures and re-fractures at the treated level. NST was ranked first in preventing adjacent vertebral fractures.
Conclusion
PVP was the most effective method for improving pain, functional status, and quality of life (based on EQ-5D). BK emerged as the best intervention for decreasing the risk of subsequent vertebral fractures and re-fractures at the treated level. NST could be ranked first in reducing adjacent vertebral fractures. The future directions of OVCFs treatment will depend on the outcomes of additional and larger randomized trials in comparing BK with PVP.




Similar content being viewed by others
References
Glaser DL, Kaplan FS (1997) Osteoporosis: definition and clinical presentation. Spine (Phila Pa 1976) 22:12s–16s
Strom O, Borgstrom F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jonsson B (2011) Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 6:59–155
Borgstrom F, Zethraeus N, Johnell O et al (2006) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 17:637–650
Silverman SL, Minshall ME, Shen W, Harper KD, Xie S (2001) The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the Multiple Outcomes of Raloxifene Evaluation Study. Arthritis Rheum 44:2611–2619
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the international Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Lau E, Ong K, Kurtz S, Schmier J, Edidin A (2008) Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am 90:1479–1486
Malmivaara A, Hakkinen U, Aro T et al (1995) The treatment of acute low back pain—bed rest, exercises, or ordinary activity? N Engl J Med 332:351–355
Reginster J, Minne HW, Sorensen OH et al (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 11:83–91
Kanis JA, Johnell O (1999) The burden of osteoporosis. J Endocrinol Investig 22:583–588
Diamond TH, Bryant C, Browne L, Clark WA (2006) Clinical outcomes after acute osteoporotic vertebral fractures: a 2-year non-randomised trial comparing percutaneous vertebroplasty with conservative therapy. Med J Aust 184:113–117
Garfin SR, Yuan HA, Reiley MA (2001) New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 26:1511–1515
Lieberman IH, Dudeney S, Reinhardt MK, Bell G (2001) Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 26:1631–1638
Chen LX, Li YL, Ning GZ, Li Y, Wu QL, Guo JX, Shi HY, Wang XB, Zhou Y, Feng SQ (2015) Comparative efficacy and tolerability of three treatments in old people with osteoporotic vertebral compression fracture: a network meta-analysis and systematic review. PLoS One 10:e0123153
Zhao S, Xu CY, Zhu AR, Ye L, Lv LL, Chen L, Huang Q, Niu F (2017) Comparison of the efficacy and safety of 3 treatments for patients with osteoporotic vertebral compression fractures: a network meta-analysis. Medicine 96:e7328
Zhang Y, Shi L, Tang P, Zhang L (2017) Comparison of the efficacy between two micro-operative therapies of old patients with osteoporotic vertebral compression fracture: a network meta-analysis. J Cell Biochem 118:3205–3212
Kan SL, Yuan ZF, Chen LX, Sun JC, Ning GZ, Feng SQ (2017) Which is best for osteoporotic vertebral compression fractures: balloon kyphoplasty, percutaneous vertebroplasty or non-surgical treatment? A study protocol for a Bayesian network meta-analysis. BMJ Open 7:e012937
Higgins JPT, Green S (editors) (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated march 2011]. The Cochrane collaboration. Available at: www.cochrane-handbook.org. Accessed 1 June 2018
Toft N, Innocent GT, Gettinby G, Reid SW (2007) Assessing the convergence of Markov Chain Monte Carlo methods: an example from evaluation of diagnostic tests in absence of a gold standard. Prev Vet Med 79:244–256
Dias S, Sutton AJ, Ades AE, Welton NJ (2013) Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making 33:607–617
Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE (2013) Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making 33:641–656
Mills EJ, Thorlund K, Ioannidis JP (2013) Demystifying trial networks and network meta-analysis. BMJ 346:f2914
Spiegelhalter DJ, Best NG, Carlin BP, Van Der Linde A (2002) Bayesian measures of model complexity and fit. J R Stat Soc Ser B (Stat Methodol) 64:583–639
Dias S, Welton NJ, Caldwell DM, Ades AE (2010) Checking consistency in mixed treatment comparison meta-analysis. Stat Med 29:932–944
Ge L, Tian JH, Li L, Wang Q, Yang KH (2015) Mesh fixation methods in open inguinal hernia repair: a protocol for network meta-analysis and trial sequential analysis of randomised controlled trials. BMJ Open 5:e009369
Dias S, Sutton AJ, Welton NJ, Ades AE (2013) Evidence synthesis for decision making 3: heterogeneity—subgroups, meta-regression, bias, and bias-adjustment. Med Decis Making 33:618–640
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS One 8:e76654
Chen G, Zhang ST, Liu YC, Sun RZ, Zhao X, Luo D (2010) Percutaneous vertebroplasty compared to conservative treatment in patients with osteoporotic vertebral compression fractures. The Journal of Cervicodynia and Lumbodynia 31:323–326
Chen JP, Qi XW, Li SJ, Kuang LP, Yuan XH, Wang GS, Tan WY (2015) Bone cement injection as vertebral augmentation therapy for osteoporotic vertebral compression fractures. Chinese Journal of Tissue Engineering Research 19:3292–3296
Dohm M, Black CM, Dacre A, Tillman JB, Fueredi G, KAVIAR investigators (2014) A randomized trial comparing balloon kyphoplasty and vertebroplasty for vertebral compression fractures due to osteoporosis. Am J Neuroradiol 35:2227–2236
Wang CH, Ma JZ, Zhang CC, Nie L (2015) Comparison of high-viscosity cement vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Pain physician E187–194
Yi X, Lu H, Tian F, Wang Y, Li C, Liu H, Liu X, Li H (2014) Recompression in new levels after percutaneous vertebroplasty and kyphoplasty compared with conservative treatment. Arch Orthop Trauma Surg 134:21–30
Boonen S, Van Meirhaeghe J, Bastian L, Cummings SR, Ranstam J, Tillman JB, Eastell R, Talmadge K, Wardlaw D (2011) Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res 26:1627–1637
Evans AJ, Kip KE, Brinjikji W, Layton KF, Jensen ML, Gaughen JR, Kallmes DF (2016) Randomized controlled trial of vertebroplasty versus kyphoplasty in the treatment of vertebral compression fractures. J Neurointerv Surg 8:756–763
Klazen CAH, Lohle PNM, De Vries J et al (2010) Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 376:1085–1092
Liu JT, Li C, Chang CS, Liao WJ (2015) Long-term follow-up study of osteoporotic vertebral compression fracture treated using balloon kyphoplasty and vertebroplasty. J Neurosurg Spine 23:94–98
Rousing R, Hansen KL, Andersen MO, Jespersen SM, Thomsen K, Lauritsen JM (2010) Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: a clinical randomized study. Spine (Phila Pa 1976) 35:478–482
Yang EZ, Xu JG, Huang GZ, Xiao WZ, Liu XK, Zeng BF, Lian XF (2016) Percutaneous vertebroplasty vs conservative treatment in aged patients with acute osteoporotic vertebral compression fractures: a prospective randomized controlled clinical study. Spine 41:654–660
Voormolen MHJ, Mali WPTM, Lohle PNM, Fransen H, Lampmann LEH, Van Der Graaf Y, Juttmann JR, Jansssens X, Verhaar HJJ (2007) Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. Am J Neuroradiol 28:555–560
Blasco J, Martinez-Ferrer A, Macho J, San Roman L, Pomes J, Carrasco J, Monegal A, Guanabens N, Peris P (2012) Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up, controlled trial. J Bone Miner Res 27:1159–1166
Chen D, An ZQ, Song S, Tang JF, Qin H (2014) Percutaneous vertebroplasty compared with conservative treatment in patients with chronic painful osteoporotic spinal fractures. J Clin Neurosci 21:473–477
Farrokhi MR, Alibai E, Maghami Z (2011) Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures: clinical article. J Neurosurg Spine 14:561–569
Belkoff SM, Mathis JM, Jasper LE, Deramond H (2001) The biomechanics of vertebroplasty. The effect of cement volume on mechanical behavior. Spine (Phila Pa 1976) 26:1537–1541
Belkoff SM, Mathis JM, Jasper LE, Deramond H (2001) An ex vivo biomechanical evaluation of a hydroxyapatite cement for use with vertebroplasty. Spine (Phila Pa 1976) 26:1542–1546
Heini PF, Walchli B, Berlemann U (2000) Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J 9:445–450
Stevenson M, Gomersall T, Lloyd Jones M, Rawdin A, Hernandez M, Dias S, Wilson D, Rees A (2014) Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for the treatment of osteoporotic vertebral fractures: a systematic review and cost-effectiveness analysis. Health Technol Assess (Winch Eng) 18:1–290
Papanastassiou ID, Phillips FM, Van Meirhaeghe J, Berenson JR, Andersson GB, Chung G, Small BJ, Aghayev K, Vrionis FD (2012) Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J 21:1826–1843
Zhao G, Liu X, Li F (2016) Balloon kyphoplasty versus percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures (OVCFs). Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA
Mahmootjan M, Zhu SB, Li JF, Jin L, Su RH, Wang X (2014) Two surgical methods for osteoporotic vertebral compression fractures: a meta-analysis on safety and efficacy. Chin J Tissue Eng Res 18:3551–3559
Chang X, Lv YF, Chen B, Li HY, Han XB, Yang K, Zhang W, Zhou Y, Li CQ (2015) Vertebroplasty versus kyphoplasty in osteoporotic vertebral compression fracture: a meta-analysis of prospective comparative studies. Int Orthop 39:491–500
Buchbinder R, Golmohammadi K, Johnston RV, Owen RJ, Homik J, Jones A, Dhillon SS, Kallmes DF, Lambert RG (2015) Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev 4:CD006349
Haywood KL, Garratt AM, Fitzpatrick R (2005) Quality of life in older people: a structured review of generic self-assessed health instruments. Qual Life Res 14:1651–1668
Yang HL, Zhao L, Liu J, Sanford CG Jr, Chen L, Tang T, Ebraheim NA (2007) Changes of pulmonary function for patients with osteoporotic vertebral compression fractures after kyphoplasty. J Spinal Disord Tech 20:221–225
Alvarez L, Alcaraz M, Perez-Higueras A, Granizo JJ, de Miguel I, Rossi RE, Quinones D (2006) Percutaneous vertebroplasty: functional improvement in patients with osteoporotic compression fractures. Spine (Phila Pa 1976) 31:1113–1118
Chosa K, Naito A, Awai K (2011) Newly developed compression fractures after percutaneous vertebroplasty: comparison with conservative treatment. Jpn J Radiol 29:335–341
Tang H, Zhao J, Hao C (2011) Osteoporotic vertebral compression fractures: surgery versus non-operative management. J Int Med Res 39:1438–1447
Fribourg D, Tang C, Sra P, Delamarter R, Bae H (2004) Incidence of subsequent vertebral fracture after kyphoplasty. Spine (Phila Pa 1976) 29:2270–2276 discussion 2277
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Li L, Ren J, Liu J, Wang H, Wang X, Liu Z, Sun T (2015) Results of vertebral augmentation treatment for patients of painful osteoporotic vertebral compression fractures: a meta-analysis of eight randomized controlled trials. PLoS One 10
Berlemann U, Ferguson SJ, Nolte LP, Heini PF (2002) Adjacent vertebral failure after vertebroplasty: a biomechanical investigation. J Bone Joint Surg Br 84:748–752
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361:569–579
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361:557–568
Funding
This work was supported by Tianjin Municipal Science and Technology Commission (16KG158), and Foundation of Tianjin Union Medical Center (2016YJZD003, 2017YJ024, 2018YJ010). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhu, RS., Kan, SL., Ning, GZ. et al. Which is the best treatment of osteoporotic vertebral compression fractures: balloon kyphoplasty, percutaneous vertebroplasty, or non-surgical treatment? A Bayesian network meta-analysis. Osteoporos Int 30, 287–298 (2019). https://doi.org/10.1007/s00198-018-4804-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4804-2