Abstract
Summary
Lumbar spine trabecular bone score (TBS) can be used to modify the output from the fracture risk assessment tool, FRAX, to enhance fracture prediction. An alternative approach for using TBS in clinical practice, based upon an adjustment to the bone mineral density (BMD) T-score, may be helpful in regions where intervention guidelines and/or reimbursement are primarily based on BMD T-score.
Introduction
The aim of this study is to develop an approach for using TBS in clinical practice based upon a “risk-equivalent” adjustment to the BMD T-score.
Methods
We identified 45,185 women age 40 years and older with baseline spine and hip DXA, TBS, and FRAX probabilities including femoral neck BMD. Incident major osteoporotic fractures (MOF, n = 3925) were identified from population-based health services data (mean follow-up 7.4 years comprising 335,910 person-years). Cox proportional hazards models adjusted for age and BMI were first used to estimate the risk for MOF from BMD T-score alone, then after including TBS and a multiplicative age interaction term. From the parameter estimates, we developed a TBS offset to the BMD T-score based upon change in TBS that would give the same risk as a unit change in BMD T-score for the femoral neck, total hip, and lumbar spine.
Results
All BMD measurements, TBS, and the age interaction term independently predicted MOF (p < 0.001). Measures of risk stratification and model fit were improved for the TBS-adjusted BMD T-score versus the unadjusted BMD T-score (p < 0.001). There was a high level of agreement between MOF probability estimated from TBS-adjusted MOF FRAX probability and FRAX probability using the “risk-equivalent” femoral BMD T-score: MOF probability r2 = 0.98, slope = 1.02, intercept = − 0.3; hip probability r2 = 0.95, slope = 1.07, intercept = 0.0.
Conclusions
The BMD-independent effect of lumbar spine TBS on fracture risk can be estimated as a simple offset to the BMD T-score.


Similar content being viewed by others
References
Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94(6):646–50. https://doi.org/10.1016/0002-9343(93)90218-E
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group Osteoporos Int 4(6):368–381. https://doi.org/10.1007/BF01622200
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9(8):1137–1141. https://doi.org/10.1002/jbmr.5650090802
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42(3):467–475. https://doi.org/10.1016/j.bone.2007.11.001
Marshall D, Hailey D, Jonsson E (1996) Health policy on bone density measurement technology in Sweden and Australia. Health Policy 35(3):217–228. https://doi.org/10.1016/0168-8510(95)00785-7
Cranney A, Jamal SA, Tsang JF, Josse RG, Leslie WD (2007) Low bone mineral density and fracture burden in postmenopausal women. CMAJ 177(6):575–580. https://doi.org/10.1503/cmaj.070234
Stone KL, Seeley DG, Lui LY, Cauley JA, Ensrud K, Browner WS, Nevitt MC, Cummings SR, Osteoporotic Fractures Research Group (2003) BMD at multiple sites and risk of fracture of multiple types: long-term results from the study of osteoporotic fractures. J Bone Miner Res 18(11):1947–1954. https://doi.org/10.1359/jbmr.2003.18.11.1947
Kanis JA (2008) Assessment of osteoporosis at the primary health-care level, technical report. Collaborating Centre, University of Sheffield, UK. https://www.sheffield.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV et al (2016) A systematic review of intervention thresholds based on FRAX : a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25. https://doi.org/10.1007/s11657-016-0278-z
Harvey NC, Gluer CC, Binkley N, McCloskey EV, Brandi ML, Cooper C et al (2015) Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone 78:216–224. https://doi.org/10.1016/j.bone.2015.05.016
Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions part 2: trabecular bone score. J Clin Densitom 18(3):309–330. https://doi.org/10.1016/j.jocd.2015.06.008
McCloskey EV, Oden A, Harvey NC, Leslie WD, Hans D, Johansson H et al (2016) A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res 31(5):940–948. https://doi.org/10.1002/jbmr.2734
McCloskey EV, Oden A, Harvey NC, Leslie WD, Hans D, Johansson H et al (2015) Adjusting fracture probability by trabecular bone score. Calcif Tissue Int 96(6):500–509. https://doi.org/10.1007/s00223-015-9980-x
Martineau P, Leslie WD, Johansson H, Oden A, McCloskey EV, Hans D, Kanis JA (2017) Clinical utility of using lumbar spine trabecular bone score to adjust fracture probability: the Manitoba BMD cohort. J Bone Miner Res 32(7):1568–1574. https://doi.org/10.1002/jbmr.3124
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis Foundation (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Kanis JA, McCloskey EV, Harvey NC, Johansson H, Leslie WD (2015) Intervention thresholds and the diagnosis of osteoporosis. J Bone Miner Res 30(10):1747–1753. https://doi.org/10.1002/jbmr.2531
Roos NP, Shapiro E (1999) Revisiting the Manitoba Centre for Health Policy and Evaluation and its population-based health information system. Med Care 37(6 Suppl):JS10–JJS4
Leslie WD, Metge C (2003) Establishing a regional bone density program: lessons from the Manitoba experience. J Clin Densitom 6(3):275–282. https://doi.org/10.1385/JCD:6:3:275
Leslie WD, Caetano PA, Macwilliam LR, Finlayson GS (2005) Construction and validation of a population-based bone densitometry database. J Clin Densitom 8(1):25–30. https://doi.org/10.1385/JCD:8:1:025
Looker AC, Orwoll ES, Johnston CC Jr, Lindsay RL, Wahner HW, Dunn WL et al (1997) Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res 12(11):1761–1768. https://doi.org/10.1359/jbmr.1997.12.11.1761
Pothuaud L, Barthe N, Krieg MA, Mehsen N, Carceller P, Hans D (2009) Evaluation of the potential use of trabecular bone score to complement bone mineral density in the diagnosis of osteoporosis: a preliminary spine BMD-matched, case-control study. J Clin Densitom 12(2):170–176. https://doi.org/10.1016/j.jocd.2008.11.006
Hans D, Goertzen AL, Krieg MA, Leslie WD (2011) Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the Manitoba study. J Bone Miner Res 26(11):2762–2769. https://doi.org/10.1002/jbmr.499
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA, Manitoba Bone Density Program (2010) Independent clinical validation of a Canadian FRAX tool: fracture prediction and model calibration. J Bone Miner Res 25(11):2350–2358. https://doi.org/10.1002/jbmr.123
Fraser LA, Langsetmo L, Berger C, Ioannidis G, Goltzman D, Adachi JD et al (2011) Fracture prediction and calibration of a Canadian FRAX(R) tool: a population-based report from CaMos. Osteoporos Int 22(3):829–837. https://doi.org/10.1007/s00198-010-1465-1
Kozyrskyj AL, Mustard CA (1998) Validation of an electronic, population-based prescription database. Ann Pharmacother 32(11):1152–1157. https://doi.org/10.1345/aph.18117
Lix LM, Azimaee M, Osman BA, Caetano P, Morin S, Metge C, Goltzman D, Kreiger N, Prior J, Leslie WD (2012) Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health 12(1):301. https://doi.org/10.1186/1471-2458-12-301
Acknowledgments
The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Population Health Research Data Repository (HIPC 2012/2013-18). The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, Healthy Living, and Seniors, or other data providers is intended or should be inferred. This article has been reviewed and approved by the members of the Manitoba Bone Density Program Committee.
Author information
Authors and Affiliations
Contributions
Conception, design, and analysis (WDL); interpretation of data (all authors); drafting the article (ES); critically revising the article for important intellectual content (all authors); final approval of the version to be published (all authors); and agreement to be accountable for all aspects of the work (all authors). WDL had full access to all the data in the study and takes the responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflicts of interest
Eugene McCloskey: Nothing to declare for FRAX and the context of this paper, but numerous ad hoc consultancies/speaking honoraria and/or research funding from Amgen, Bayer, General Electric, GSK, Hologic, Lilly, Merck Research Labs, Novartis, Novo Nordisk, Nycomed, Ono, Pfizer, ProStrakan, Roche, Sanofi-Aventis, Servier, Tethys, UBS, and Warner-Chilcott.
Didier Hans: Co-ownership in the TBS patent. Stock options or royalties: Med-Imaps. Research grants: Amgen, Radius Pharma, Agnovos, GE Healthcare.
Nicholas Harvey: Nothing to declare for FRAX and the context of this paper but has received consultancy, lecture fees, and honoraria from Alliance for Better Bone Health, AMGEN, MSD, Eli Lilly, Servier, Shire, UCB, Radius, Consilient Healthcare, and Internis Pharma.
John A. Kanis: Grants from Amgen, grants from Lilly, non-financial support from Medimaps, grants from Unigene, nonfinancial support from Asahi, grants from Radius Health, outside the submitted work; and Dr. Kanis is the architect of FRAX but has no financial interest. Governmental and NGOs: National Institute for health and clinical Excellence (NICE), UK; International Osteoporosis Foundation; INSERM, France; Ministry of Public Health, China; Ministry of Health, Australia; Ministry of Health, Abu Dhabi; National Osteoporosis Guideline Group, UK; WHO.
Appendix
Appendix
Mean-centered age (AgeC) is calculated as age − 63.5; mean-centered age-normalized TBS (TBSCAN) is calculated as TBSCAN = (TBS − 1.32) + AgeC × 0.00413, where 1.32 is the mean TBS of the study population, 63.5 is the mean age, and 0.00413 is the β-coefficient of age in the linear regression with TBS.
Relative gradients were calculated as the ratios of the Cox model parameter estimates of BMD T-score alone versus the parameter estimate of TBSCAN, or versus the parameter estimate of AgeC × TBSCAN interaction term. From Table 2, the relative gradients for TBSCAN for the femoral neck (FN), total hip (TH), and lumbar spine (LS) regions were 0.28, 0.29, and 0.13, respectively, and for the AgeN × TBSCAN interaction term were − 7.63, − 6.89, and − 3.26, respectively. The calculation of TBS-adjusted BMD T-scores for the three regions is as follows:
-
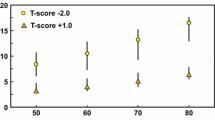
TBS-adjusted FN BMD T-score = FN BMD T-score + TBSCAN/0.28 − AgeC × TBSCAN/7.63
-
TBS-adjusted hip BMD T-score = hip BMD T-score + TBSCAN/0.29 − AgeC × TBSCAN/6.89
-
TBS-adjusted LS BMD T-score = LS BMD T-score + TBSCAN/0.13 − AgeC × TBSCAN/3.26
Rights and permissions
About this article
Cite this article
Leslie, W.D., Shevroja, E., Johansson, H. et al. Risk-equivalent T-score adjustment for using lumbar spine trabecular bone score (TBS): the Manitoba BMD registry. Osteoporos Int 29, 751–758 (2018). https://doi.org/10.1007/s00198-018-4405-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4405-0