Abstract
Summary
Hypovitaminosis D is a problem among hip fracture patients. In a 1-year cohort study comprising 245 hip fracture patients (mean age of females 81 years and males 78 years) from south-eastern Finland, the mean 25-hydroxyvitamin D [S-25(OH)D] concentration was 73(SD 31) nmol/L. Vitamin D supplementation has been integrated into our current practice.
Introduction
The objectives of this study are to verify vitamin D levels among hip fracture patients and to compare the results with a similar study conducted in the same two hospitals covering the same geographic area 12 years ago.
Methods
A prospective cohort comprising 245 Caucasian hip fracture patients was enrolled in the study in two acute hospitals in south-eastern Finland (61° N) over a 12-month period in 2015–2016. The S-25(OH)D was measured using 25-hydroxyvitamin D electrochemiluminescence binding assay. The S-25(OH)D concentrations were compared with the corresponding concentrations of a similar cohort analyzed in the same two hospitals 12 years ago.
Results
Of the 245 patients, 70% were women with a mean age of 81 (SD 10) years, while the men had a mean age of 78 (SD 12) years (p < 0.01). The total mean S-25(OH)D concentration was 73 (SD 31.3) nmol/L. Regional differences were found: 15% in hospital A and 36% in hospital B had a S-25(OH(D level < 50 nmol/L, and the mean S-25(OH)D level was 79.2 (SD 31.7) nmol/L in hospital A and 62.4 (SD 27.5) nmol/L in hospital B (p < 0.001). No differences were found in S-25(OH)D concentrations by either the place of residence or the time of year. Overall, the percentage of patients with a sufficient vitamin D level (> 50 nmol/L) was remarkably higher in 2015–2016 (77%) than in 2003–2004 (22%).
Conclusion
Our results indicate that vitamin D supplementation has been widely integrated into our current practice. However, regional differences were found in the S-25(OH)D concentrations for which the reasons are unknown.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D deficiency is a common global problem [1]. It causes secondary hyperparathyroidism, high bone turnover, bone loss, mineralization defects, as well as hip and other fractures [2].
The risk factors for vitamin D deficiency are related to race, latitude, exposure to sunlight, decreased functional capacity of the skin, and the use of vitamin D supplementation. Older adults are at a high risk of developing vitamin D deficiency due to decreased cutaneous synthesis and dietary intake of vitamin D and to the efficacy of vitamin D supplementation.
According to the most recent recommendation from The European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO), 50 nmol/L (i.e., 20 ng/mL) should be the minimal serum 25-hydroxyvitamin D [S-25(OH)D] concentration at the population level and in patients with osteoporosis to ensure optimal bone health [3]. Below this threshold, vitamin D supplementation is recommended at 800 to 1000 IU/day [3]. In fragile elderly subjects who are at a heightened risk of falls and fractures, the ESCEO recommends a minimum S-25(OH)D level of 75 nmol/L (i.e., 30 ng/mL), in order to achieve the greatest impact on fracture prevention [3]. The upper limit of adequacy, i.e., the level above which adverse effects are possible, is defined as 125 nmol/L (i.e., 50 ng/mL) [4]. Vitamin D status appears to be inversely related to fractures in middle-aged adults. In older adults, the dose response relationship between baseline vitamin D status and fracture risk appears to be J-shaped [5]. According to a recent meta-analysis, a low vitamin D level (≤ 50 nmol/L) is associated with an increased risk of all types of fractures and hip fractures [6].
Falls are a major risk factor for fractures. Calcium and vitamin D supplementation leads to a modest reduction in fracture risk, although population level intervention has not been shown to be an effective public health strategy [7]. According to the literature, calcium alone did not lead to a clinically significant fracture reduction [8].
The most serious type of fracture in the elderly is hip fracture, because nearly all patients are treated operatively and their first-year morbidity and mortality after the fracture are high. In 2003 and 2004, we studied the S-25(OH)D status in 223 Caucasian patients with an acute hip fracture in two hospitals in south-eastern Finland (61° N). The hospitals are responsible for an area comprising a total of 300,000 inhabitants [9]. In this study conducted 12 years ago, only every fifth patient with an acute hip fracture had a sufficient vitamin D level (≥ 50 nmol/L) [9].
In the present study, our aim was to verify vitamin D levels among hip fracture patients in the same two hospitals covering the same geographic area with prospective data collected over 1 year and to compare the present vitamin D concentrations to those found in the previous study 12 years ago [9].
Material and methods
We registered prospective, consecutive patients with a fresh hip fracture at the Päijät-Häme Central Hospital (A) in the city of Lahti and at the North Kymi Hospital (B) in the city of Kouvola, in south-eastern Finland (61° N). A number of patients in Kouvola were transferred to the Central Hospital of Kymenlaakso, in the city of Kotka, and these patients were included in the hip fracture data of the North Kymi Hospital. The fractures were coded in accordance with ICD-10 classification, as had been conducted in 2003–2004 for femoral neck fractures (S72.0), trochanteric fractures (S72.1), and subtrochanteric fractures (S72.2). Pathological fractures and high-energy fractures were excluded.
The study period in both hospitals was from October 15, 2015 to October 14, 2016 (12 months). Hospital A is responsible for an area of 210,000 inhabitants and hospital B, correspondingly, for 86,000 inhabitants. The study was approved by the Ethics Committee of Surgery at the Hospital District of Helsinki and Uusimaa in Finland. Written informed consent was obtained from all patients.
Data gathering
Most of the basic data gathering was performed by dedicated nurses trained for this work. They compiled, prospectively, the questionnaire with data regarding the patients’ background: age, gender, height, weight, place of residence, date and time of injury, date of admission, use of medication, and previous fractures.
The patients’ place of residence was defined: (i) patient’s actual/private home, further defined as “private home”; (ii) residential care home for the elderly or any unit of residence provided by the social care services, further defined as “residential home”; (iii) service home with 24-h staff assistance, further defined as “service home with 24-h assistance”; and (iv) hospital or other institution. Previous fractures were classified: fracture of the proximal humerus, elbow, wrist, rib, vertebra, pelvis, hip, femur, knee, tibia and ankle, or multiple fractures suffered at the age of 50 years or older.
Each patient or his/her representative (relative or carer) was asked whether he/she used calcium and/or vitamin D supplementation and/or anti-osteoporotic drugs on a daily basis before the injury.
The types of fractures were recorded by an orthopedic surgeon in all the hospitals (RT., P.L., A.T.). The ASA score (American Society of Anaesthesiologists score) [10] was also recorded.
Laboratory measures
Serum samples were collected after arrival at hospital. Serum samples were centrifuged at 2000g for 10 min and frozen as soon as possible. The frozen samples were transferred from hospital B to hospital A, where all the samples were stored at − 70 °C until analyzed in batches. Serum assays were performed in cobas 8000 modular analyzer series (Roche Diagnostic GmbH, Mannheim, Germany).
S-25(OH)D was measured using 25-hydroxyvitamin D electrochemiluminescence binding assay (Roche Diagnostic GmbH, Mannheim, Germany). The assay employs a vitamin D binding protein to bind vitamin D3 (25-OH) and vitamin D2 (25-OH). The measurement range is 7.5–175 nmol/L, and reference range is > 50 nmol/L. The method has been standardized against liquid chromatography-tandem mass spectrometry [11] which, in turn, has been standardized to the NIST standard [12]. At the normal range (mean 70.8 nmol/L), repeatability and intermediate precision of the test are 3.9 and 6.5%, respectively.
Cross-reactivity for 25-hydroxyvitamin D3 is 100% both in the current assay (Roche Diagnostics) and in the radioimmunoassay (IDS) used in the previous study [9] and for 25-hydroxyvitamin D2, 92 and 75%, respectively. According to information provided by the manufacturers, there is no significant difference in cross-reactivity for 24,25-dihydroxyvitamin D3, cholecalciferol D3, and ergocalciferol D2 between the assays.
In order to compare the S-25(OH)D concentrations of the present study with the corresponding results of the previous study [9], the S-25(OH)D concentrations of the previous study [9] were re-analyzed in accordance with the prevailing S-25(OH)D classification.
Statistical analyses
Differences between two groups were tested using the chi-squared test and Wilcoxon rank test, and, in cases of more than two groups, with the Kruskal-Wallis test. Fisher’s exact test was used when appropriate. For differences in the mean values between more than two groups, the two-way analysis of variance (ANOVA) was applied. The p values < 0.05 were considered statistically significant.
Results
The baseline characteristics of the patients, distribution of fracture types and ASA classes, and the pre-fracture use of calcium and vitamin D supplements according to hospitals are shown in Table 1. The most relevant basic variables of the previous study on 223 hip fracture patients [9] are shown in Table 2.
During the study period, a total of 245 Caucasian patients (70% female) with an acute hip fracture were enrolled in the study: 156/245 (64%) patients in hospital A and 89/245 (36%) patients in hospital B. Two hip fracture patients (2/89) in North Kymi Hospital (hospital B) were operated on at the Kymenlaakso Central Hospital, Kotka. No differences were found in the mean age of males and females between the hospitals (Table 1). In the total data, the mean age of females was 81 (SD 9.5) years and males 78 (SD 12) years (F-test: 5.36, d.f. = 1; 240, p < 0.01).
Thirty-seven percent of patients (91/245) had sustained 119 previous fractures, mainly hip (29%), wrist (24%), or vertebra (11%) fractures (Fig. 1). Nine percent of patients (23/245) had previously sustained multiple fractures (range: 2–4 fractures) (Table 1), mostly wrist, hip, or proximal humerus fractures (Fig. 1). Sixty percent had sustained no previous fractures, and information on previous fractures was missing in seven patients. A total of 4% of the patients had used anti-osteoporotic medication before the index hip fracture (Table 1).
Vitamin D status
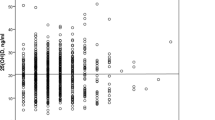
The mean S-25(OH)D concentration was 73.1 (SD 31.3) nmol/L, and there was a slight difference in mean vitamin D levels between males and females; 67.0 (SD 31.0) nmol/L vs. 75.8 (SD 31.1) nmol/L, respectively (F-test 4.49, d.f. = 1; 239, p < 0.05).
The distribution of S-25(OH)D concentrations according to hospital is shown in Table 3. 25-hydroxyvitamin D assay was missing in one patient in hospital B. In the total data, four patients had a S-25(OH)D concentration below 10 nmol/L and as many patients had a level above 150 nmol/L. The mean S-25(OH)D level was 79.2 (SD 31.7) nmol/L in hospital A and 62.4 (SD 27.5) nmol/L in hospital B (F-test: 17.39, d.f. = 1; 239, p < 0.001). The S-25(OH)D concentration was insufficient (< 50 nmol/L) in 36.3% of the patients in hospital B, whereas the corresponding figure in hospital A was 14.8% (Table 3).
In the previous study [9], there were no differences in S-25(OH)D concentrations between the hospitals. Overall, the S-25(OH)D concentrations were lower in the previous study than in the present study. In the previous study, the S-25(OH)D concentration was < 50 nmol/L in 77.6% of the patients, and 3.1% reached the optimal level of 75–120 nmol/L (Table 3).
Previous fractures and vitamin D
Whether the patient had sustained none, one, or more than one previous fracture, or the figure remained unknown (7 cases), there were no differences in the mean vitamin D levels between these groups (F-test: 0.68, d.f. = 1; 237, n.s.). Regarding the respective hospitals, there were differences between the groups: hospital A patients had a higher mean vitamin D level in all groups (F-test: 17.14; d.f. = 1; 237, p < 0.001).
ASA class and vitamin D
Most of the patients who belonged to ASA class 3 (n = 146) had a vitamin D level of ≥ 50 nmol/L (113/146, 77%). Those who belonged to ASA class 4 (n = 65, one assay missing) also had a vitamin D level of ≥ 50 nmol/L (51/65, 78%). An optimal level (> 75 nmol/L) was achieved in 50% of ASA class 3 and in 43% of ASA class 4.
BMI and vitamin D
Body mass index (BMI, kg/m2) was calculated in 216 patients. No difference was found in BMI distribution (< 25 kg/m2; 25–49 kg/m2; 50–74 kg/m2; 75–120 kg/m2; > 120 kg/m2) between the sexes (χ2 = 4.18, d.f. = 3, n.s.). The average BMI was 24 kg/m2, and there were no differences in the mean BMI between the sexes or the hospitals. There was no association between the distributions of BMI classes and vitamin D levels (χ2 = 1.16, d.f. = 3, n.s.).
Place of residence, time of year, and vitamin D
In the total data of the present study, there were no differences in the vitamin D levels between places of residence (Table 4). A more detailed study of vitamin D levels at the patients’ place of residence according to hospital revealed that there were more patients with vitamin D concentration < 50 nmol/L in hospital B among those patients who came from private homes (20/56, 35.7%) than among corresponding patients in hospital A (21/120, 18%) (Fisher’s exact = 0.006). In addition, a non-significant trend towards hypovitaminosis D was noted among hospital B patients coming from service homes with 24-h assistance (1/16, 6.2%) compared to the corresponding patients in hospital A (7/21, 33%) (Fisher’s exact = 0.054). In the previous study conducted 12 years ago [9], no differences were found in the vitamin D levels between the places of residence (Table 4).
No differences were found in the present study in patients’ S-25(OH)D concentrations between the late summer and early fall months (August, September, October) and the late winter months (January, February, March) (Wilcoxon = − 0.26, n.s.), whereas in the previous study [9], patients’ S-25(OH)D concentrations were significantly lower in the winter months than in the late summer months (p < 0.01) (Table 5).
Discussion
The main result of this study was that vitamin D levels among hip fracture patients have improved remarkably over a 12-year period. Our present results showed a significant increase in S-25(OH)D levels among hip fracture patients in comparison with the results of our previous study from 2003 to 2004 among the same target group and in the same hospitals [9]. From 2003 to 2004, the proportion of hip fracture patients with a sufficient S-25(OH)D level (> 50 nmol/L) was 22.4% [9], whereas in the present study, the corresponding figure was 77.5%. Thus, a significant reduction of patients with vitamin D levels < 50 nmol/L was observed. Furthermore, 12 years ago, only 3% of patients reached the optimal S-25(OH)D level of 75 to 120 nmol/L [9], whereas the corresponding figure in the present study was 40%.
However, regional differences were found in our present results: more than one third of patients in the hospital B region had an insufficient vitamin D level (< 50 nmol/L) compared to the figure of 15% in hospital A. Also, the average S-25(OH)D level was lower in hospital B than in hospital A. We do not know the reason for this. The distance between the two hospitals is approximately 70 km. The information on the importance of vitamin D for an individual’s health should have been similar everywhere in the country.
Sufficient vitamin D intake is important for general health, and low vitamin D status may increase the risk of contracting many common chronic diseases. In northern latitudes, exposure to UVB light is limited, and the formation of vitamin D in the skin occurs during March and October only [13]. Interestingly, in the present study, vitamin D levels were evenly distributed regardless of the time of year. The situation was quite the opposite in 2003–2004; during the winter months, the corresponding levels were significantly lower than those in the fall months [9]. The present findings indicate a regular enhancement of vitamin D in its various forms among the elderly population throughout the year.
Moreover, in our present study, as in the previous study [9], the place of residence was not important regarding vitamin D status. A study from Switzerland showed a severe vitamin D deficiency in Swiss hip fracture patients (n = 222) [14]. Vitamin D deficiency below 30 nmol/L was present in 60% of patients, 80% were below 50 nmol/L, and only 4% reached a level of 75 nmol/L. The levels varied according to place of residence: the mean S-25(OH)D level was 34.6 nmol/L among hip fracture patients admitted from home, 27.7 nmol/L among those coming from assisted living, and 24 nmol/L among nursing home residents [14].
In a more recent study from Germany [15], vitamin D deficiency was present in 87% of 209 patients with an acute femoral neck fracture. The mean S-25(OH)D concentration was 8.4 ng/mL (21 nmol/L). The 1-year mortality of patients with severe (< 10 ng/mL, i.e., < 25 nmol/L) and mild (10–20 ng/mL, i.e., 25–50 nmol/L) vitamin D deficiency was 29% and 13%, respectively, compared to 9% in patients with ≥ 20 ng/mL (≥ 50 nmol/L). Furthermore, pre-fracture vitamin D deficiency was independently associated with post-operative medical complications [15].
In our previous study [16], with a follow-up time of 11 years, hip fracture patients with a pre-fracture S-25(OH)D concentration of ≥ 50 nmol/L had the highest survival at the end of the follow-up. Survival rate was lowest during the entire follow-up among those patients with a vitamin D level of ≤ 25 nmol/L. Those who had a vitamin D level of 25–49 nmol/L survived slightly better up to 7 years than those with a level of ≥ 50 nmol/L [16].
Vitamin D deficiency has been the subject of discussion in Finland over the last decade. Liquid dairy products and fat spreads (not butter) were fortified with vitamin D in 2003 and 2010. According to recommendations, older people over 75 years of age, as well as younger people who spend little time outdoors, should get up to 20 μg/day of vitamin D to achieve 50 nmol/L serum concentration level [17]. In the 2–74 years age group, the recommendation for vitamin D supplementation is 10 μg/day, and 20 μg/day in the age group from 75 years and above, if daily use of dairy products, fat spreads, and/or fish is insufficient [18]. In the most recent Finnish National FINDIET 2012 Survey, vitamin D supplements were used by 33% of working age men and 55% of working age women, as well as 37% of older men and 60% of older women up to 74 years of age [19]. Unfortunately, the Finnish National FINDIET 2012 Survey did not include the use of these supplements among people aged 75 years and older.
According to Finnish Osteoporosis guidelines [20], the S-25(OH)D level above 50 nmol/L has been stated as being sufficient. Furthermore, patients with a S-25(OH)D level below 50 nmol/L suffer from hypovitaminosis D, and the target level of vitamin D should be 75 to 120 nmol/L (optimal level) [20]. However, high S-25(OH)D concentrations may increase the odds of elderly people falling. This was suggested in a recent study [21] in which the increase in falls was found in the group with S-25(OH)D concentrations of 44.7 to 98.9 ng/mL (i.e., 111 to 246 nmol/L) compared with the group with S-25(OH)D levels of 21.3 to 30.3 ng/mL (i.e., 53 to 75 nmol/L). In the present data, there were 17 patients (7%) with a S-25(OH)D level of ≥ 120 nmol/L.
The present study indicates that vitamin D deficiency among the elderly is not as common as it was in Finland 12 years ago. This important finding is supported by a very recent prospective study using nationally representative data on Finnish adults aged ≥ 30 years with an 11-year follow-up [22]. The mean S-25 (OH)D level among the ≥ 75-year-olds increased from 43 nmol/L in 2000 to 65.1 nmol/L in 2011, and the prevalence of vitamin D deficiency decreased, correspondingly, from 65.5% to 9.7% [22].
In a recent meta-analysis by Feng et al. [6] comprising 16 prospective cohort studies, the risk of total and hip fractures was analyzed. The results showed that the low S-25(OH)D level was significantly associated with the risk of total and hip fractures. The low S-25(OH)D level varied between 15 and 21 ng/mL (37.5–52.3 nmol/L). The risk of hip fractures increased by 40% for each SD decrease in S-25(OH)D level. However, the per SD decrease in S-25(OH)D was not associated with the increased risk of total fracture [6]. Moreover, a prospective study among Japanese community-dwelling women with a 15-year follow-up showed that low S-25(OH)D levels, especially < 20 ng/mL (< 50 nmol/L), were associated with elevated fracture risk [23].
According to a previous review [24], all-cause death rate, cancer and cardiovascular diseases, multiple carcinomas, osteoporosis, bone fractures in elderly women, and other aging-related diseases show a U-shaped dependency on S-25(OH)D concentration. The optimal S-25(OH)D concentration appeared to be 40–80 nmol/L on the population level. Because vitamin D is a hormone, like any other hormone, it is harmful in both too low and too high concentrations [24].
Finally, vitamin D deficiency has been relatively well defined in the literature. However, thus far, an upper “safe” threshold for S-25(OH)D level has not been defined for which a consensus has been reached.
The present study has both strengths and limitations. One of the main strengths is the prospective design of the study. Moreover, all S-25(OH)D concentrations were analyzed in one and the same laboratory using the same method. Previous fractures were identified in 37% of patients. According to our previous study, hip fracture patients were good at recalling the number of fractures, if any, they had previously sustained [9]. We subsequently confirmed the accuracy of the number of previous fractures in another study by checking the patients’ medical records manually [25]. The figures were similar: 34% [9] and 35% [25]. We assume that the information on previous fractures is also as accurate in the present study.
One limitation is the missing data. The study was planned to include all consecutive patients with an acute hip fracture. However, the drop-out figure was 44% in hospital A and 35.5% in hospital B. We know that only a small number of patients did not wish to participate in the study. However, we were actually surprised at how difficult it was to stimulate the staff in the ERs of both hospitals to cooperate in the study. It would appear that the busy timetable and occasional backlogs in the ERs were the main reasons for drop outs.
However, the male to female ratio (30:70) and the mean age of the patients (80 years) in the present data were similar to the corresponding figures in the Finnish National hip fracture register (32:68 and 79 years, respectively) [26] Also, the distribution rate of fracture types (femoral neck, trochanteric, and subtrochanteric fractures) was similar to national rates [26]. Based on these figures, there does not seem to be any systematic bias in our data. Nonetheless, the potential influence of the missing data on the results remains unclear.
In conclusion, the improved situation in vitamin D levels among hip fracture patients is most probably due to the vitamin D fortification of liquid dairy products and spreads in Finland in 2003 and 2010. Furthermore, a great deal of information has been published on the benefits of vitamin D supplementation and on the measurement of vitamin D levels. The Finnish Osteoporosis Association has been active in this matter. The population of the present study area covers around 5.5% of the total Finnish population of 5.5 million. Our results indicate that vitamin D supplementation has been widely integrated into our current practice. The improved serum 25-hydroxyvitamin levels may partially explain the declining trend in the incidence of hip fracture in Finland during the first decade of the new millennium [27].
Change history
05 March 2018
The presentation of Table 4 was unclear in the original publication. The article has now been corrected in this respect.
References
Lips P (2010) Worldwide status of vitamin D nutrition. J Steroid Biochem Mol Biol 121:297–300
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22:477–501
Rizzoli R, Boonen S, Brandi ML, Bruyère O, Cooper C, Kanis JA, Kaufman JM, Ringe JD, Weryha G, Reginster JY (2013) Vitamin D supplementation in elderly or postmenopausal women: a 2013 update of the 2008 recommendations from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Curr Med Res Opin 29:305–313. https://doi.org/10.1185/03007995
Aloia JF (2011) Clinical Review: the 2011 report on dietary reference intake for vitamin D: where do we go from here? J Clin Endocrinol Metab 96:2987–2996
Julian C, Lentjes MA, Huybrechts I, Luben R, Wareham N, Moreno LA, Khaw KT (2016) Fracture risk in relation to serum 25-hydroxyvitamin D and physical activity: results from the epic-norfolk cohort study. PLoS One 17:11. https://doi.org/10.1371/journal.pone.0164160 eCollection 2016
Feng Y, Cheng G, Wang H, Chen B (2017) The associations between serum 25-hydroxyvitamin D level and the risk of total fracture and hip fracture. Osteoporos Int 28:1641–1652
Harvey NC, Biver E, Kaufman JM, Bauer J, Branco J, Brandi ML, Bruyère O, Coxam V, Cruz-Jentoft A, Czerwinski E, Dimai H, Fardellone P, Landi F, Reginster JY, Dawson-Hughes B, Kanis JA, Rizzoli R, Cooper C (2017) The role of calcium supplementation in healthy musculoskeletal ageing: an expert consensus meeting of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Foundation for Osteoporosis (IOF). Osteoporos Int 28:447–462
Tai V, Leung W, Grey A, Reid IR, Bolland MJ (2015) Calcium intake and bone mineral density: systematic review and meta-analysis BMJ 351: h4183. doi: https://doi.org/10.1136/bmj.h4183
Nurmi I, Kaukonen JP, Lüthje P, Naboulsi H, Tanninen S, Kataja M, Kallio ML, Leppilampi M (2005) Half of the patients with an acute hip fracture suffer from hypovitaminosis D: a prospective study in southeastern Finland. Osteoporos Int 16:2018–2024
Haynes SR, Lawler PG (1995) An assessment of the consistency of ASA physical status classification allocation. Anaesthesia 50:195–199
Vogeser M, Kyriarsoulis A, Huber E, Kobold U (2004) Candidate reference method for the quantification of circulating 25-hydroxyvitamin D3 by liquid chromatography-tandem mass spectrometry. Clin Chem 50:1415–1417
Phinney KW (2008) Development of a standard reference material for vitamin D in serum. Am J Clin Nutr 88(suppl):511–512
Lamberg-Allardt C, Brustad M, Meyer HE (2013) Vitamin D—a systematic review for the 5th edition of the Nordic Nutrition Recommendations. Food Nutr Res 57, https://doi.org/10.3402/fnr.v57i0.22671; eCollection 2013. Modified 27.12.2016
Bischoff-Ferrari HA, Can U, Staehelin HB, Platz A, Henschkowski J, Michel BA, Dawson-Hughes B, Theiler R (2008) Severe vitamin D deficiency in Swiss hip fracture patients. Bone 42:597–602
Fakler JKM, Grafe A, Dinger J, Josten C, Aust G (2016) Perioperative risk factors in patients with a femoral neck fracture—influence of 25-hydroxyvitamin D and C-reactive protein on postoperative medical complications and 1-year mortality. BMC Musculoskelet Disord 17:51. https://doi.org/10.1186/s12891-016-0906-1
Nurmi-Lüthje I, Lüthje P, Kaukonen JP, Kataja M (2015) Positive effects of a sufficient pre-fracture serum vitamin D level on the long-term survival of hip fracture patients in Finland: a minimum 11-year follow-up. Drugs Aging 32:477–486
https://www.evira.fi/en/foodstuff/healthy-diet/ (2016). Accessed 24 July 2017
Nordic Council of Ministers. Nordic Nutrition recommendations (2012) https://doi.org/10.6027/Nord2014-002 (access via Norden iLibrary)
Helldán A, Raulio S, Kosola M, Tapanainen H, Ovaskainen M-L, Virtanen S (2012) The national FINDIET 2012 survey. Reports of Institution of Health and Welfare, 16/2013. Helsinki, Finland https://www.julkari.fi/bitstream/handle/10024/110839/THL_RAP2013_016_%26sliitteet.pdf?sequence=1, (accessed 14 July.2017)
Osteoporosis. Current Care Guideline (2014) http://www.kaypahoito.fi/web/english/guidelineabstracts/guideline?id=ccs00102 (Published 24.04.2014 in Finnish)
Bischoff-Ferrari H, Dawson-Hughes B, Orav JE, Staehelin HB, Meyer OW, Theiler R, Dick E, Willet WC, Egli A (2016) Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern Med 176:175–183
Jääskeläinen T, Itkonen ST, Lundqvist A, Erkkola M, Koskela T, Lakkala K, Dowling KG, Hull GLJ, Kröger H, Karppinen J, Kyllönen E, Härkänen T, Cashman KD, Männistö S, Lamberg-Allardt C (2017) The positive impact of general vitamin D fortification policy on vitamin D status in a representative adults Finnish population: evidence from an 11-year follow-up based on standardized 25-hydroxyvitamin D data. Am J Clin Nutr 105:1512–1520
Tamaki J, Iki M, Sato Y, Kajita F, Nishino H, Akiba T, Matsumoto T, Kagamimori S (2017) Total 25-hydroxyvitamin D levels predict fracture risk: results from the 15-year follow-up of the Japanese Population-based Osteoporosis (JPOS) Cohort Study. Osteoporos Int 28:1903–1913
Tuohimaa P, Lou Y-R (2012) Optimal serum calcidiol concentration for cancer prevention. Anticancer Res 32:373–382
Lüthje P, Helkamaa T, Kaukonen JP, Nurmi-Lüthje I, Kataja M (2012) A long-term follow-up of 221 hip fracture patients in southeastern Finland: analysis of survival and prior or subsequent fractures. Arch Gerontol Geriatr 54:e294–e299. https://doi.org/10.1016/j.archger.2011.12.002
THL, National Institute for Health and Welfare (2017) PERFECT – PERFormance, Effectiveness and Cost of Treatment episodes. https://www.thl.fi/fi/tutkimus-ja-asiantuntijatyo/hankkeet-ja ohjelmat/perfect/osahankkeet/lonkkamurtuma/perusraportit Accessed 9 February 2017
Korhonen N, Niemi S, Parkkari J, Sievänen H, Palvanen M, Kannus P (2013) Continuous decline in incidence of hip fracture: nationwide statistics from Finland between 1970 and 2010. Osteoporos Int 24:1599–1603. https://doi.org/10.1007/s00198-012-2190-8
Acknowledgements
The authors would like to express their thanks to the staff of the ERs and laboratories in both hospitals for their help in conducting the study.
Funding
The study received support from the following sources: The Centenary Foundation of Kymi Corporation, the Research Foundations of Helsinki and Tampere University Hospitals, and the Kouvola Medical Association.
Author information
Authors and Affiliations
Ethics declarations
Conflicts of interest
None.
Additional information
A correction to this article is available online at https://doi.org/10.1007/s00198-018-4432-x.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nurmi-Lüthje, I., Tiihonen, R., Paattiniemi, EL. et al. Remarkable improvement in serum 25-hydroxyvitamin levels among hip fracture patients over a 12-year period: a prospective study in South-eastern Finland. Osteoporos Int 29, 837–845 (2018). https://doi.org/10.1007/s00198-017-4344-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4344-1