Abstract
Introduction and hypothesis
The aim of this study is to compare the effectiveness of transcutaneous tibial nerve stimulation (TTNS) on quality of life (QoL) and clinical parameters related to incontinence in pharmacological agents (PhAs) naive and refractory women with idiopathic overactive bladder (iOAB).
Methods
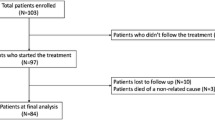
In this prospective nonrandomized clinical trial, women with resistance to PhAs were included in the first group (n=21), PhA-naive women were included in the second group (n=21). TTNS was performed 2 days a week, a total of 12 sessions for 6 weeks. Every session lasted 30 min. Women were evaluated for the severity of incontinence (Pad test), 3-day voiding diary (voiding frequency, nocturia, incontinence episodes, and number of pads), symptom severity (Overactive Bladder Questionnaire-V8), quality of life (Incontinence Impact Questionnaire-7), treatment satisfaction, positive response, and cure-improvement rates.
Results
A statistically significant improvement was found in all parameters for each group at the 6th week compared with the baseline values (p<0.05). It was found that the severity of incontinence, incontinence episodes, symptom severity, treatment satisfaction, and QoL parameters were significantly improved in PhA-naive group compared with the PhA-resistant group at the 6th week (p<0.05). There were no statistically significant differences in the frequency of voiding, nocturia, and number of pads between the two groups (p>0.05). Positive response rates, the primary outcome measure, were statistically significantly higher in the PhA-naive group than in the PhA-resistant group.
Conclusions
Although TTNS is more effective in PhA-naive women with iOAB, it appears to be an effective therapy that can also be used in the management of PhA-resistant women with iOAB.


Similar content being viewed by others
Abbreviations
- BT:
-
Bladder training
- iOAB:
-
İdiopathic overactive bladder
- PhA:
-
Pharmacological agents
- PTNS:
-
Percutaneous tibial nerve stimulation
- QoL:
-
Quality of life
- TTNS:
-
Transcutaneous tibial nerve stimulation
References
Bo K, Frawley HC, Haylen BT, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J. 2017;28(2):191–213. https://pubmed.ncbi.nlm.nih.gov/27921161/
Kasman A, Stave C, Elliott CS. Combination therapy in overactive bladder untapped research opportunities: a systematic review of the literature. Neurourol Urodyn. 2019;38(8):2083–92. https://pubmed.ncbi.nlm.nih.gov/31483070/
Wang S, Lv J, Feng X, Lv T. Efficacy of electrical pudendal nerve stimulation versus transvaginal electrical stimulation in treating female idiopathic urgency urinary incontinence. J Urol. 2017;197(6):1496–501. https://pubmed.ncbi.nlm.nih.gov/28153510/
La Rosa VL, Platania A, Ciebiera M, et al. A comparison of sacral neuromodulation vs. transvaginal electrical stimulation for the treatment of refractory overactive bladder: the impact on quality of life, body image, sexual function, and emotional wellbeing. Menopause Rev. 2019;18(2):89–93. https://pubmed.ncbi.nlm.nih.gov/31485205/
Gormley EA, Lightner DJ, Faraday M, Vasavada SP. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline Amendment. J Urol. 2015;193:1572–80. https://pubmed.ncbi.nlm.nih.gov/25623739/
Sonmez R, Yildiz N, Alkan H. Efficacy of percutaneous and transcutaneous tibial nerve stimulation in women with idiopathic overactive bladder: a prospective randomised controlled trial. Ann Phys Rehabil Med. 2022;65(1):101486. https://pubmed.ncbi.nlm.nih.gov/33429090/
Booth J, Hagen S, McClurg D, et al. A feasibility study of transcutaneous posterior tibial nerve stimulation for bladder and bowel dysfunction in elderly adults in residential care. J Am Med Dir Assoc. 2013;14(4):270–4. https://pubmed.ncbi.nlm.nih.gov/23206722/
Manríquez V, Guzmán R, Naser M, et al. Transcutaneous posterior tibial nerve stimulation versus extended release oxybutynin in overactive bladder patients. A prospective randomized trial. Eur J Obstet Gynecol Reprod Biol. 2016;196:6–10. https://pubmed.ncbi.nlm.nih.gov/26645117/
Schreiner L, Dos Santos TG, Knorst MR, Da Silva Filho IG. Randomized trial of transcutaneous tibial nerve stimulation to treat urge urinary incontinence in older women. Int Urogynecol J. 2010;21(9):1065–70. https://pubmed.ncbi.nlm.nih.gov/20458465/
Ramírez-García I, Blanco-Ratto L, Kauffmann S, Carralero-Martínez A, Sánchez E. Efficacy of transcutaneous stimulation of the posterior tibial nerve compared to percutaneous stimulation in idiopathic overactive bladder syndrome: randomized control trial. Neurourol Urodyn. 2019;38(1):261–8. https://pubmed.ncbi.nlm.nih.gov/30311692/
Harding CK, Lapitan MC, Arlandis S, et al. The European Association of Urology (EAU) Guidelines. In: EAU guidelines on management of non-neurogenic female lower urinary tract symptoms. EAU Guidelines (Internet); 2023. https://uroweb.org/guidelines/non-neurogenic-female-luts
Schreiner L, Nygaard CC, Dos Santos TG, Knorst MR, da Silva Filho IG. Transcutaneous tibial nerve stimulation to treat urgency urinary incontinence in older women: 12-month follow-up of a randomized controlled trial. Int Urogynecol J. 2021;32(3):687–93. https://pubmed.ncbi.nlm.nih.gov/33057739/
Ammi M, Chautard D, Brassart E, Culty T, Azzouzi AR, Bigot P. Transcutaneous posterior tibial nerve stimulation: evaluation of a therapeutic option in the management of anticholinergic refractory overactive bladder. Int Urogynecol J. 2014;25(8):1065–9. https://pubmed.ncbi.nlm.nih.gov/24599180/
Firinci S, Yildiz N, Alkan H, Aybek Z. Which combination is most effective in women with idiopathic overactive bladder, including bladder training, biofeedback, and electrical stimulation? A prospective randomized controlled trial. Neurourol Urodyn. 2020;39(8):2498–508. https://pubmed.ncbi.nlm.nih.gov/32960999/
Yildiz N, Alkan H, Sarsan A. Efficacy of intravaginal electrical stimulation added to bladder training in women with idiopathic overactive bladder: a prospective randomized controlled trial. Int Braz J Urol. 2021;47:1150–9. https://pubmed.ncbi.nlm.nih.gov/34469668/
Yildiz N, Alkan H, Findikoglu G. Efficacy of intravaginal electrical stimulation with different treatment frequency in women with refractory idiopathic overactive bladder. Int Braz J Urol. 2022;48(4):662–71. https://pubmed.ncbi.nlm.nih.gov/35363455/
Lee HE, Cho SY, Lee S, Kim M, Oh SJ. Short-term effects of a systematized bladder training program for idiopathic overactive bladder: a prospective study. Int Neurourol J. 2013;17(1):11–7. https://pubmed.ncbi.nlm.nih.gov/23610706/
Berghmans B, van Waalwijk van Doorn E, Nieman F, et al. Efficacy of physical therapeutic modalities in women with proven bladder overactivity. Eur Urol. 2002;41(6):581–587. https://pubmed.ncbi.nlm.nih.gov/12074773/
Yildiz N, Unal B. Comparison of the efficacy of intravaginal electrical stimulation in women with idiopathic overactive bladder naive and refractory to pharmacological agents. Int Urogynecol J. 2023;34(9):2099–105. https://pubmed.ncbi.nlm.nih.gov/36976326/
Abdelbary AM, El-Dessoukey AA, Massoud AM, et al. Combined vaginal pelvic floor electrical stimulation (PFS) and local vaginal estrogen for treatment of overactive bladder (OAB) in perimenopausal females. Randomized controlled trial (RCT) Urology. 2015;86(3):482–6. https://pubmed.ncbi.nlm.nih.gov/26135813/
Yamanishi T, Yasuda K, Sakakibara R, Hattori T, Suda S. Randomized, double-blind study of electrical stimulation for urinary incontinence due to detrusor overactivity. Urology. 2000;55:353–7. https://pubmed.ncbi.nlm.nih.gov/10699609/
O'Sullivan R, Karantanis E, Stevermuer TL, Allen W, Moore KH. Definition of mild, moderate and severe incontinence on the 24-hour pad test. BJOG. 2004;111(8):859–62. https://pubmed.ncbi.nlm.nih.gov/15270937/
Tarcan T, Mangır N, Özgür MÖ, Akbal C. OAB-V8 overactive bladder questionnaire validation study. Üroloji Bülteni. 2012;21:113–6. http://www.kontinansdernegi.org/userfiles/media/kontinans.galenos.com.tr/oab-v8-asiri-aktif-mesanesorgulama-formu.pdf
Acquadro C, Kopp Z, Coyne KS, et al. Translating overactive bladder questionnaires in 14 languages. Urology. 2006;67(3):536–40. https://pubmed.ncbi.nlm.nih.gov/16527574/
Cam C, Sakalli M, Ay P, Cam M, Karateke A. Validation of the short form of the incontinence impact questionnaire (IIQ-7) and the urogenital distress inventory (UDI-6) in a Turkish population. Neurourol Urodyn. 2007;26:129–133. https://pubmed.ncbi.nlm.nih.gov/17083117/
Padilla-Fernández B, Castro-Díaz DM. Combination therapy for overactive bladder: should we define refractoriness? Eur Urol. 2019;76(6):780–1. https://pubmed.ncbi.nlm.nih.gov/31540792/
Phé V, de Wachter S, Rouprêt M, Chartier-Kastler E. How to define a refractory idiopathic overactive bladder? Neurourol Urodyn. 2015;34(1):2–11. https://pubmed.ncbi.nlm.nih.gov/24155183/
Apostolidis A, Averbeck MA, Sahai A, et al. Can we create a valid treatment algorithm for patients with drug resistant overactive bladder (OAB) syndrome or detrusor overactivity (DO)? Results from a think tank (ICI-RS 2015). Neurourol Urodyn. 2017;36(4):882–93. https://pubmed.ncbi.nlm.nih.gov/28444708/
Funding statement
This study was not supported by any of the funding sources.
Data availability
Data are not open to the public but can be obtained from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Contributions
N. Yildiz: protocol/project development, data analysis, manuscript writing/editing; M.A. Celtek: protocol/project development, data collection.
Corresponding author
Ethics declarations
Ethics of approval statement
The study protocol was approved by the Institutional Review Board of Pamukkale University (approval number: E-60116787-020-277289).
Patient consent statement
All women were informed about the purpose and contents of the study and all women signed written consent to participate in the study.
Conflicts of interest
None.
Additional information
Handling Editor: G. Alessandro Digesu
Editor in Chief: Maria Bortolini
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yildiz, N., Celtek, M.A. Effects of Transcutaneous Tibial Nerve Stimulation in Women Refractory to and Never Used Pharmacological Agents for Idiopathic Overactive Bladder. Int Urogynecol J 35, 571–578 (2024). https://doi.org/10.1007/s00192-023-05704-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05704-0