Abstract
Introduction and hypothesis
Postpartum lumbopelvic pain (PLPP) is common among women. Abdominal, diaphragm, and pelvic floor muscles (PFMs) modulate intraabdominal pressure as a part of the force closure mechanism. These muscles are exposed to changes during pregnancy that compromise the force closure mechanism. It was hypothesized that abdominal and PFMs activity, the direction of bladder base displacement, diaphragm thickness, and excursion might differ between women with and without PLPP during respiratory and postural tasks.
Methods
Thirty women with and 30 women without PLPP participated in this case–control study. Ultrasound imaging was used to assess the abdominal, diaphragm, and PFMs during rest, active straight leg raising (ASLR) with and without a pelvic belt, and deep respiration.
Results
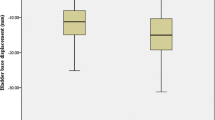
The bladder base descent was significantly greater in the PLPP group than in the controls during deep respiration and ASLR without a belt (p = 0.026; Chi-squared = 6.40). No significant differences were observed between the groups in the abdominal muscles activity and diaphragm muscle thickness. There was a significant interaction effect of the group and the task for diaphragm excursion (F (2, 116) = 6.08; p = 0.00) and PFM activity (F (2, 116) = 5.22; p = 0.00). In the PLPP group, wearing a belt compromised altered PFM activation and direction of bladder base displacement.
Conclusion
The PFM activity, direction of bladder base displacement, and diaphragm excursion differed between groups during postural and respiratory tasks. Therefore, it is recommended to involve retraining of the PFMs and diaphragm muscle in the rehabilitation of women with PLPP.


Similar content being viewed by others
References
Wu WH, Meijer OG, Uegaki K, et al. Pregnancy-related pelvic girdle pain (PPP), I: terminology, clinical presentation, and prevalence. Eur Spine J. 2004;13(7):575–89. https://doi.org/10.1007/s00586-003-0615-y.
Pool-Goudzwaard A, Vleeming A, Stoeckart R, Snijders C, Mens JM. Insufficient lumbopelvic stability: a clinical, anatomical and biomechanical approach to ‘a-specific’ low back pain. Man Ther. 1998;3(1):12–20.
O’Sullivan PB, Beales DJ, Beetham JA, et al. Altered motor control strategies in subjects with sacroiliac joint pain during the active straight-leg-raise test. Spine. 2002;27(1):E1–8.
LoMauro A, Aliverti A. Respiratory physiology of pregnancy: physiology masterclass. Breathe (Sheff). 2015;11(4):297–301. https://doi.org/10.1183/20734735.008615.
Vleeming A, Pool-Goudzwaard AL, Hammudoghlu D, Stoeckart R, Snijders CJ, Mens JM. The function of the long dorsal sacroiliac ligament: its implication for understanding low back pain. Spine. 1996;21(5):556–62. https://doi.org/10.1097/00007632-199603010-00005.
Mohan V, Paungmali A, Sitilerpisan P, Hashim UF, Mazlan MB, Nasuha TN. Respiratory characteristics of individuals with non-specific low back pain: a cross-sectional study. Nurs Health Sci. 2018;20(2):224–30. https://doi.org/10.1111/nhs.12406.
Rasouli O, Shanbehzadeh S, Arab AM, ShahAli S, Sarafraz H. The effect of respiratory phase on abdominal muscle activity during stable and unstable sitting positions in individuals with and without chronic low back pain. J Manip Physiol Ther. 2020;43(3):225–33. https://doi.org/10.1016/j.jmpt.2019.02.013.
Talasz H, Kofler M, Kalchschmid E, Pretterklieber M, Lechleitner M. Breathing with the pelvic floor? Correlation of pelvic floor muscle function and expiratory flows in healthy young nulliparous women. Int Urogynecol J. 2010;21(4):475–81. https://doi.org/10.1007/s00192-009-1060-1.
Martínez-Bustelo S, Ferri-Morales A, Corral-Gómez L, Castillo-García FJ, Castro-Varela V, Jácome MA. Transabdominal ultrasound to assess the displacement of the bladder base during abdominal and pelvic floor contractions in continent parous versus nulliparous women. Int Urogynecol J. 2022;33(8):2257–66. https://doi.org/10.1007/s00192-021-04756-4.
Arumugam A, Milosavljevic S, Woodley S, Sole G. Effects of external pelvic compression on form closure, force closure, and neuromotor control of the lumbopelvic spine—a systematic review. Man Ther. 2012;17(4):275–84. https://doi.org/10.1016/j.math.2012.01.010.
O'Sullivan PB. Lumbar segmental instability: clinical presentation and specific stabilizing exercise management. Man Ther. 2000;5(1):2–12.
Laslett M, Aprill CN, McDonald B, Young SB. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10(3):207–18. https://doi.org/10.1016/j.math.2005.01.003.
Teyhen DS, Williamson JN, Carlson NH, et al. Ultrasound characteristics of the deep abdominal muscles during the active straight leg raise test. Arch Phys Med Rehabil. 2009;90(5):761–7. https://doi.org/10.1016/j.apmr.2008.11.011.
Ehsani F, Sahebi N, Shanbehzadeh S, Arab AM, ShahAli S. Stabilization exercise affects function of transverse abdominis and pelvic floor muscles in women with postpartum lumbo-pelvic pain: a double-blinded randomized clinical trial study. Int Urogynecol J. 2020;31(1):197–204. https://doi.org/10.1007/s00192-019-03877-1.
Mens JM, Damen L, Snijders CJ, Stam HJ. The mechanical effect of a pelvic belt in patients with pregnancy-related pelvic pain. Clin Biomech (Bristol, Avon). 2006;21(2):122–7. https://doi.org/10.1016/j.clinbiomech.2005.08.016.
Scarlata S, Mancini D, Laudisio A, Benigni A, Antonelli Incalzi R. Reproducibility and clinical correlates of supine diaphragmatic motion measured by M-mode ultrasonography in healthy volunteers. Respiration. 2018;96(3):259–66. https://doi.org/10.1159/000489229.
Sarwal A, Walker FO, Cartwright MS. Neuromuscular ultrasound for evaluation of the diaphragm. Muscle Nerve. 2013;47(3):319–29. https://doi.org/10.1002/mus.23671.
Arab AM, Behbahani RB, Lorestani L, Azari A. Assessment of pelvic floor muscle function in women with and without low back pain using transabdominal ultrasound. Man Ther. 2010;15(3):235–9. https://doi.org/10.1016/j.math.2009.12.005.
Okamoto M, Murayama R, Haruna M, et al. Evaluation of pelvic floor function by transabdominal ultrasound in postpartum women. J Med Ultrason. 2010;37(4):187–93.
Whittaker JL. Ultrasound imaging for rehabilitation of the lumbopelvic region: a clinical approach. Amsterdam: Elsevier Health Sciences; 2007.
ShahAli S, Arab AM, Ebrahimi E, et al. Ultrasound measurement of abdominal muscles during clinical isometric endurance tests in women with and without low back pain. Physiother Theory Pract. 2019;35(2):130–8.
Ziaeifar M, Sarrafzadeh J, Noorizadeh Dehkordi S, Arab AM, Haghighatkhah H, Zendehdel Jadehkenari A. Diaphragm thickness, thickness change, and excursion in subjects with and without nonspecific low back pain using B-mode and M-mode ultrasonography. Physiother Theory Pract. 2022;38(13):2441–51. https://doi.org/10.1080/09593985.2021.1926022.
Kolář P, Šulc J, Kynčl M, et al. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352–62.
Arranz-Martín B, García-Gallego P, Romay-Barrero H, et al. Bladder base displacement during abdominal muscles contraction and functional activities in primiparous women assessed by transabdominal ultrasound: a descriptive study. J Clin Med. 2021;11(1):25.https://doi.org/10.3390/jcm11010025.
Beales DJ, O'Sullivan PB, Briffa NK. The effects of manual pelvic compression on trunk motor control during an active straight leg raise in chronic pelvic girdle pain subjects. Man Ther. 2010;15(2):190–9. https://doi.org/10.1016/j.math.2009.10.008.
Stuge B, Sætre K, Ingeborg Hoff B. The automatic pelvic floor muscle response to the active straight leg raise in cases with pelvic girdle pain and matched controls. Man Ther. 2013;18(4):327–32. https://doi.org/10.1016/j.math.2012.12.004.
Sjödahl J, Gutke A, Ghaffari G, Strömberg T, Öberg B. Response of the muscles in the pelvic floor and the lower lateral abdominal wall during the active straight leg raise in women with and without pelvic girdle pain: an experimental study. Clin Biomech (Bristol, Avon). 2016;35:49–55. https://doi.org/10.1016/j.clinbiomech.2016.04.007.
Weis CA, Nash J, Triano JJ, Barrett J. Ultrasound assessment of abdominal muscle thickness in women with and without low back pain during pregnancy. J Manip Physiol Ther. 2017;40(4):230–5. https://doi.org/10.1016/j.jmpt.2017.02.002.
Rostami M, Noormohammadpour P, Mansournia MA, et al. Comparison of the thickness of lateral abdominal muscles between pregnant women with and without low back pain. PM R. 2015;7(5):474–8. https://doi.org/10.1016/j.pmrj.2014.10.014.
Weis CA, Triano JJ, Barrett J, Campbell MD, Croy M, Roeder J. Ultrasound assessment of abdominal muscle thickness in postpartum vs nulliparous women. J Manip Physiol Ther. 2015;38(5):352–7. https://doi.org/10.1016/j.jmpt.2015.06.005.
Author information
Authors and Affiliations
Contributions
G. Kharaji: project development, data collection, manuscript writing/editing, final approval; S. ShahAli: project development, manuscript writing/editing, final approval; E. Takamjani: project development, manuscript editing, final approval; M. Kashanian: project development, final approval; J. Sarrafzadeh: data analysis, Manuscript writing/editing, final approval; S. Shanbehzadeh: data analysis, manuscript editing, final approval.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 474 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kharaji, G., ShahAli, S., Ebrahimi Takamjani, I. et al. Ultrasound assessment of the abdominal, diaphragm, and pelvic floor muscles during the respiratory and postural tasks in women with and without postpartum lumbopelvic pain: a case–control study. Int Urogynecol J 34, 2909–2917 (2023). https://doi.org/10.1007/s00192-023-05621-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05621-2