Abstract
Introduction and hypothesis
Factors that contribute to reoperation and surgical approaches for the management of recurrent uterovaginal prolapse after vaginal mesh hysteropexy (mesh hysteropexy) are unknown. We aimed to describe surgical management of pelvic organ prolapse recurrence after vaginal mesh hysteropexy, and patient characteristics in those who chose reoperation.
Methods
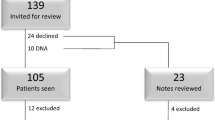
This is a descriptive analysis of women who experienced treatment failure within 5 years of mesh hysteropexy in a multi-site randomized trial. The composite definition of treatment failure included retreatment (pessary or reoperation), prolapse beyond the hymen, or bothersome prolapse symptoms. Characteristics of those pursuing and not pursuing repeat prolapse surgery, measures of prolapse, and symptom severity are described.
Results
Over 5-year follow up, 31/91 (34%) of the hysteropexy group met treatment failure criteria. All seven women who pursued reoperation reported bothersome prolapse symptoms; six were anatomic failures. Most seeking reoperation were early treatment failures; six (86%) by the 12-month visit and all by the 18-month visit. Compared to those electing expectant management, those pursuing reoperation had more apical prolapse, POP-Q point C median (IQR) −5.5 (−6.0, −4.0) cm versus +1.0 (−1.0, 3.0) cm respectively. Hysterectomy was performed in 6/7 reoperations (three vaginal, three endoscopic), with apical suspension in 5/6 hysterectomies. One participant with posterior compartment prolapse underwent transvaginal enterocele plication, uterosacral ligament suspension with posterior colpoperineorrhaphy. At a mean surgical follow-up of 34.3 (15.8) months, all women remained without anatomic or symptomatic failure.
Conclusions
When recurrent prolapse after mesh hysteropexy occurred, most women did not choose reoperation. Those who pursued surgery experienced more significant apical prolapse and were universally symptomatic.
Clinical trial identification number
NCT01802281
Similar content being viewed by others
References
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470 e1–6.
Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD. Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg. 2013;19(2):103–9.
Kapoor S, Sivanesan K, Robertson JA, Veerasingham M, Kapoor V. Sacrospinous hysteropexy: review and meta-analysis of outcomes. Int Urogynecol J. 2017;28(9):1285–94.
Bradley S, Gutman RE, Richter LA. Hysteropexy: an option for the repair of pelvic organ prolapse. Curr Urol Rep. 2018;19(2):15.
Nager CW, Zyczynski H, Rogers RG, Barber MD, Richter HE, Visco AG, et al. The design of a randomized trial of vaginal surgery for uterovaginal prolapse: vaginal hysterectomy with native tissue vault suspension versus mesh hysteropexy suspension (the Study of Uterine Prolapse Procedures Randomized Trial). Female Pelvic Med Reconstr Surg. 2016;22(4):182–9.
Nager CW, Visco AG, Richter HE, Rardin CR, Rogers RG, Harvie HS, et al. Effect of vaginal mesh hysteropexy vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: a randomized clinical trial. JAMA. 2019;322(11):1054–65.
Nager CW, Visco AG, Richter HE, Rardin CR, Komesu Y, Harvie HS, et al. Effect of sacrospinous hysteropexy with graft vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: 5-year results of a randomized clinical trial. Am J Obstet Gynecol. 2021;225(2):153 e1–e31.
Gutman RE, Rardin CR, Sokol ER, Matthews C, Park AJ, Iglesia CB, et al. Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 2017;216(1):38 e1–e11.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Yalcin I, Bump RC. Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol. 2003;189(1):98–101.
Schulten SFM, Detollenaere RJ, Stekelenburg J, IntHout J, Kluivers KB, van Eijndhoven HWF. Sacrospinous hysteropexy versus vaginal hysterectomy with uterosacral ligament suspension in women with uterine prolapse stage 2 or higher: observational follow-up of a multicentre randomised trial. BMJ. 2019;366:l5149.
FDA. FDA's activities: urogynecologic surgical mesh 2019 [updated 9/2/2021; cited 2021 11//18/2021]. Silver Spring MD: Food and Drug Administration; 2021. Available from: https://www.fda.gov/medical-devices/urogynecologic-surgical-mesh-implants/fdas-activities-urogynecologic-surgical-mesh. Accessed 11/28/21
Acknowledgements
The authors would like to acknowledge those in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Pelvic Floor Disorders Network who contributed to the SUPeR Study
Alpert Medical School of Brown University, Providence, RI
Charles R. Rardin, Deborah L. Myers, Cassandra Carberry, B. Star Hampton, Kyle Wohlrab, Nicole Korbly, Ann S. Meers, Samantha Douglas, Elizabeth-Ann Viscione
Cleveland Clinic, Cleveland OH
Matthew Barber, Eric Jelovsek, Cecile Ferrando, Marie Fidela R Paraiso, Ly Pung, Annette Graham, Geetha Krishnan, Kathleen Dastoli, Maryori Edington, Mark Walters
Duke University Medical Center, Durham, NC
Anthony G. Visco, Alison Weidner, Cindy Amundsen, Nazema Siddiqui, Amie Kawasaki, Shantae McLean, Mary Raynor, Nicole Longoria, Akira Hayes, Robin Gilliam, Acacia Harris
Kaiser Permanente – San Diego, San Diego, CA
Shawn A. Menefee, Jasmine Tan-Kim, Gouri B. Diwadkar, Keisha Y. Dyer, Linda M. Mackinnon, Gisselle Zazueta-Damian
Magee-Womens Research Institute, Pittsburgh, PA
Pamela Moalli, Michael Bonidie, Jerry Lowder, Jonathan Shepherd, Gary Sutkin, Judy Gruss, Karen Mislanovich, Kate Amodei, Lindsey Baranski
RTI International, Research Triangle Park, NC
Dennis Wallace, Sonia Thomas, Kimberly McMillian, Ryan Whitworth, Amanda Shaffer, Tracey Grant, Kelly Koeller-Anna, Ben Carper, Emily Honeycutt, Katrina Burson, Kendra Glass, James Pickett
University of Alabama at Birmingham, Birmingham, AL
Holly E Richter, R. Edward Varner, Robert L. Holley, Tracey Wilson, Alicia Ballard, David Ellington, Ryanne Johnson, Alyssa Long, Lisa Pair, Velria Willis, Alice Howell, Nancy Saxon, Kathy Carter, Robin Willingham, Ryanne Johnson, Jill Hyde, Sunita Patel
UC San Diego Health, San Diego, CA
Charles Nager, Emily S. Lukacz, Michael E. Albo, Keisha Y. Dyer, Marianna Alperin, Anna C. Kirby, Kimberly Ferrante, Erika Wasenda, Joann Columbo, Erika Ruppert, Kyle Herrala, Sherella Johnson
University of New Mexico, Albuquerque, NM
Rebecca G Rogers, Yuko Komesu, Gena Dunivan, Peter Jeppson, Sara Cichowski, Julia Middendorf, Karen Box.
University of Pennsylvania, Philadelphia, PA
Lily Arya, Uduak Andy, Ariana Smith, Lorraine Flick. Michelle Kingslee, Teresa Carney, Donna Thompson
Funding
Eunice Kennedy Shriver National Institute of Child Health and Human Development grants HD069006, HD069031, HD069025, HD041261, HD069010, HD069013, HD054214, HD041267, HD054215 and NIH Office of Research on Women’s Health. Boston Scientific Corporation provided partial study support through an unrestricted grant.
Author information
Authors and Affiliations
Contributions
G.S. Napoe: project development, manuscript writing and editing
D. Luchristt: manuscript writing and editing
A. Sridhar: project development, data analysis, manuscript writing and editing
D. Ellington: manuscript writing and editing
B. Ridgeway: manuscript writing and editing
D. Mazloomdoost: manuscript writing and editing
V. Sung: manuscript writing and editing
C. Ninivaggio: manuscript writing and editing
H. Harvie: manuscript writing and editing
Y. Santiago-Lastra: manuscript writing and editing
M.G. Gantz: project development, data management, data analysis, manuscript writing and editing
H.M. Zyczynski: project development, data collection, manuscript writing and editing
Corresponding author
Ethics declarations
Conflicts of interests
Marie Gantz reports that Boston Scientific Corporation provided partial support for the SUPeR study through an unrestricted grant. All other authors report no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Paper presentation information
An abstract of this paper was presented as a poster at the Society of Gynecologic Surgeons 48th Annual Scientific Meeting in San Antonio, TX, March 27–30, 2022
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Napoe, G.S., Luchristt, D., Sridhar, A. et al. Reoperation for prolapse recurrence after sacrospinous mesh hysteropexy: characteristics of women choosing retreatment. Int Urogynecol J 34, 255–261 (2023). https://doi.org/10.1007/s00192-022-05411-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05411-2