Abstract
Introduction and hypothesis
The objective of this study was to evaluate long-term outcomes of laparoscopic sacrocolpopexy (LSC) versus abdominal sacrocolpopexy (ASC) for vaginal vault prolapse (VVP).
Methods
Long-term follow-up of a multicenter randomized controlled trial (SALTO trial). A total of 74 women were randomly assigned to LSC (n=37) or ASC (n=37). Primary outcome was disease-specific quality of life, measured with validated questionnaires. Secondary outcomes included anatomical outcome, composite outcome of success, complications, and retreatment.
Results
We analyzed 22 patients in the LSC group and 19 patients in the ASC group for long-term follow-up, with a median follow-up of 109 months (9.1 years). Disease-specific quality of life did not differ after long-term follow-up with median scores of 0.0 (LSC: IQR 0–17; ASC: IQR 0–0) on the “genital prolapse” domain of the Urogenital Distress Inventory in both groups (p = 0.175). Anatomical outcomes were the same for both groups on all points of the POP-Q. The composite outcome of success for the apical compartment is 78.6% (n = 11) in the LSC group and 84.6% (n = 11) in the ASC group (p = 0.686). Mesh exposures occurred in 2 patients (12.5%) in the LSC group and 1 patient (7.7%) in the ASC group. There were 5 surgical reinterventions in both groups (LSC: 22.7%; ASC: 26.3%, p = 0.729).
Conclusions
At long-term follow-up no substantial differences in quality of life, anatomical results, complications, or reinterventions between LSC and ASC were observed. Therefore, the laparoscopic approach is preferable, considering the short-term advantages.
Trial registration
Dutch Trial Register NTR6330, 18 January 2017, https://www.trialregister.nl/trial/5964
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of vaginal vault prolapse (VVP), requiring apical surgery, has been reported in 23% of women who underwent vaginal hysterectomy for pelvic organ prolapse (POP) [1]. The risk of developing VVP increases in the years after hysterectomy, especially in women whose initial hysterectomy was performed for POP [2, 3]. Pelvic floor symptoms due to POP can have a severe impact on women’s quality of life, requiring an effective treatment [4].
Sacrocolpopexy is one of the surgical options in the treatment of VVP, with success rates between 93 and 99% [5,6,7,8]. Sacrocolpopexy is associated with a lower risk of awareness of prolapse, recurrent prolapse on examination, repeat surgery for prolapse, and dyspareunia than other vaginal interventions for POP [9]. Previously, the results of the SALTO trial were published [10, 11]. In this multicenter RCT, we compared laparoscopic sacrocolpopexy (LSC) with abdominal sacrocolpopexy (ASC) as treatment for VVP, with a follow-up time of 12 months. The results showed less blood loss, a shorter hospital stay, and less related morbidity in favor of the laparoscopic group. There was a significant improvement in quality of life in both groups [10, 11].
Evidence for long-term clinical outcomes of LSC versus ASC is essential to reach consensus on the optimal surgical treatment, adequate patient selection and preoperative counselling. Therefore, this follow-up study was performed to evaluate the long-term outcome in terms of disease-specific quality of life of patients who participated in the SALTO trial.
Materials and methods
Study design
Details of the SALTO trial were published previously [10, 11]. In short, a multicenter randomized controlled trial was performed, comparing LSC and ASC as treatment for VVP, in four teaching hospitals and two university hospitals in the Netherlands. Eligible women with vault prolapse who met the inclusion criteria were informed about the trial, and randomized after consent. Inclusion criteria were women with a history of hysterectomy presenting with symptomatic vaginal vault prolapse, with or without concomitant cystocele or rectocele, who chose to undergo surgery.
This observational long-term follow-up study was approved by the ethical research committee (METC) of the Máxima Medical Centre (file number METC W17.015, CCMO NL60618.015.17) and by the board of directors of each of the participating hospitals, separately from the original SALTO trial. This trial was registered in the Dutch Trial Register (NTR6330). The study was developed and described in accordance with the Consolidated Standards of Reporting Trials (CONSORT) 2010 statement [12]. The results are reported by means of the joint International Urogynecological Association (IUGA)/International Continence Society (ICS) recommendations for reporting outcomes of surgical procedures for pelvic organ prolapse [13].
Primary and secondary outcomes
The primary outcome of this trial was long-term disease-specific quality of life, measured with the Urogenital Distress Inventory (UDI). The primary outcome in our follow-up study is similar to the original SALTO trial. Secondary outcomes were the effects of the surgical treatment on POP-related functional symptoms such as micturition, defecation, sexuality, and patient satisfaction, using validated questionnaires. Moreover, long-term complications such as mesh exposure and retreatment were evaluated. Surgical retreatment was categorized according to the joint IUGA/ICS recommendations for reporting outcomes. Surgeries were subdivided into repeat surgery for the apical compartment, surgery for a different site (anterior or posterior compartment), surgery for complications, and surgery for non-POP-related conditions (e.g., stress urinary incontinence) [13, 14].
More outcome definitions were used in the literature after the initial SALTO study [14]. To make studies more comparable, we have added several secondary outcome measures. We analyzed composite outcome of success, defined as no POP beyond the hymen (apical compartment), absence of bothersome bulge symptoms, and no repeat surgery. Additionally, we examined surgical failure, which meant prolapse POP-Q ≥ stage 2 (in the apical compartment or in any compartment) or surgical reintervention. Last, anatomical failure (POP-Q ≥ stage 2) was evaluated [13,14,15].
Data collection
All patients from the initial SALTO trial were sent a letter to ask for participation in this observational follow-up study. When they failed to respond, they were called and asked to participate. All participants gave new informed consent to participate in the long-term follow-up trial. They were asked to fill in various Dutch validated questionnaires and were invited to visit an outpatient clinic to undergo pelvic examination. The observer was an independent researcher, gynecologist or resident who had not performed the surgery and was trained in the POP-Q examination [16]. The observer was not blinded to the type of surgery, because of visible abdominal scars.
Disease-specific quality of life was tested with the UDI [17], the Defecatory Distress Inventory (DDI) [18], and the Incontinence Impact Questionnaire (IIQ) [17]. The UDI and DDI, containing of 19 and 11 items respectively, indicate whether complaints of micturition, prolapse, or defecation are present and to what extent these complaints are bothersome. These questionnaires consist of four-point Likert scales, ranging from “no bother” to “greatly bothersome.” The result of the IIQ questionnaire, composed of 13 questions, shows the disease-specific quality of life for urine incontinence. The score of each domain ranges from 0–100, a high score indicates more frequent or more bothersome symptoms (UDI and DDI), and hence, a poorer quality of life (IIQ). Patient satisfaction of their postoperative condition was verified by the Patient Global Impression of Improvement (PGI-I). The PGI-I is a seven-point Likert scale answering the question: “check the number that best describes what your post-operative condition is like now, compared with what it was like before you had the surgery” [19]. “Much better” or “very much better” was considered affirmative and presented as dichotomous outcome [9]. Furthermore, we evaluated sexual functioning using the Prolapse/Incontinence Sexual Questionnaire (PISQ), containing 12 questions. These items were scored on a five-point Likert scale ranging from 0 (always) to 4 (never), for which higher score indicates better sexual function [20, 21].
Bothersome bulge symptoms were measured using the UDI. A positive answer to any of the following questions is scored as a subjective recurrence: “Do you experience a sensation of bulging or protrusion from the vagina?” and “Do you have a bulge or something protruding that you can see in the vagina?”, in combination with a response “moderately bothersome” or “greatly bothersome” to the question “how much does this bother you?”
Interventions
Laparoscopic sacrocolpopexy
Laparoscopic sacrocolpopexy was performed under general anesthesia using four trocars, one for the scope and three side trocars. The vaginal vault was elevated with a vaginal probe. The peritoneum from the promontory to the vault was incised laparoscopically by scissors to expose the rectovaginal and vesicovaginal fascia. A type 1 polypropylene mesh was used, which was cut into two pieces; 3 cm wide and approximately 15 cm long. One piece of the mesh was attached anteriorly and another as low as possible on the posterior vaginal wall, using non-absorbable multifilament sutures. The mesh was fixated to the anterior part of the vaginal vault with four stitches, and six stitches were used to fixate the mesh posteriorly. The mesh was attached to the sacral promontory using staples and was peritonealized [10].
Abdominal sacrocolpopexy
The ASC was performed by a laparotomy under general anesthesia, preferably using a Pfannenstiel incision. The essence of the procedure was the same as for the laparoscopic procedure. The peritoneum from the promontory to the vault was incised to expose the rectovaginal and vesicovaginal fascia, extending to the sacral promontory. One piece of type 1 polypropylene mesh was attached between the vagina and the bladder anteriorly, and another as far down the posterior vaginal wall as possible. The sutures, the size of the mesh and its fixation were the same as in the laparoscopic approach. The two meshes were sutured to each other, after which only the posterior mesh was fixed to the longitudinal vertebral ligament by staples or non-absorbable sutures, depending on the surgeon’s preference. The mesh was peritonealized. All centers used polypropylene meshes and the same sutures [10].
Sample size
Sample size calculation was performed for the initial SALTO trial and 74 patients were included accordingly [10]. Loss to follow-up from the initial trial was taken into account and a response rate of 60% was estimated. A difference of 15 points between the two groups on the “genital prolapse” domain from the UDI was considered a clinically relevant difference. The standard deviation of the UDI score was 15.8 [22]. With an α level of 0.05 and a 60% response rate, the calculated power would be 83% and was considered to be adequate.
Statistical analysis
The domain scores were calculated for the UDI, DDI, IIQ, PISQ, and PGI-I questionnaires. To examine differences between the two groups the independent-samples t test was used for continuous variables. The Mann–Whitney U test was used in the case of non-normally distributed variables. For dichotomous variables, Pearson’s Chi-squared test was used. The log-rank test was used for survival analysis of the time to surgical retreatment. Two-sided significance tests were used, and a p value of less than 0.05 was considered to be statistically significant. All statistical analyses were performed using IBM SPSS for Windows (version 25).
Results
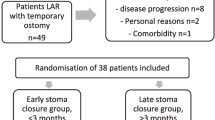
In the original trial 74 women were randomly assigned to LSC (n = 37) or ASC (n = 37) between 2007 and 2012. Figure 1 shows the flow diagram of the study population. In total 71 participants were eligible for long-term follow-up, 36 participants in the LSC group and 35 patients in the ASC group. We included 22 patients (61.1%) from the LSC group and 19 patients (54.3%) from the ASC group. Fourteen patients (38.9%) were lost to follow-up in the LSC group versus 16 patients (45.7%) in the ASC group; 9 patients died and 8 patients were not able to participate owing to old age or serious health conditions (unrelated to pelvic floor symptoms, e.g., terminal stage cancer). Nine patients were not willing to participate in this follow-up study. For most of them it was too much of a burden, none reported any POP-related complaints. In the LSC group 1 patient was lost to follow-up in the initial trial owing to postponed surgery, but agreed to participate now. Meanwhile, she received the allocated intervention (LSC).
Table 1 shows the baseline characteristics and peri-operative data of the patients in the SALTO trial. The median duration of follow-up was 109 months (9.1 years), 105 months (8.75 years) in the LSC group and 111 months (9.25 years) in the ASC group. In the LSC group 88.2% (n = 30) had two vaginal deliveries or more, compared with 94.1% (n = 32) in the ASC group. Also, the majority is postmenopausal at the time of surgery (LSC: 97.2%, n = 35; ASC: 100%, n = 37).
The primary outcome of long-term disease-specific quality of life, measured with the UDI, was not different between groups. The median score for the domain “genital prolapse” was 0 (IQR 0–17) in the LSC group as well as in the ASC group (IQR 0–0; p = 0.175). On the other domains of the UDI, DDI, and IIQ, we did not observe any statistically significant differences, as is shown in Table 2. An improvement of “much better” or “very much better” on the PGI-I was reported by 11 patients (57.9%) in the LSC group, and 10 patients (58.8%) in the ASC group (p = 0.955). Sexual function was the same in both groups, with total PISQ scores of 34.2 (range 19–45) and 32.5 (range 28–37) in the LSC and ASC group respectively (p = 0.132). Thirty percent (n = 6) of the participants in the LSC group were sexually active, compared with 63% (n = 20) before surgery. In the ASC group there was also a reduction, from 45% (n = 14) to 10.5% (n = 2). Four patients were reported to have dyspareunia, two patients in each group (p = 0.102). Two patients also reported this pre-operatively, one in each group. From one patient, pre-operative data on sexuality are missing (ASC group) and the other patient was not sexually active before surgery (LSC group). Therefore, it was unclear whether the reported dyspareunia of these two patients occurred after surgery.
As shown in Table 3, the composite outcome of success for the apical compartment was 78.6% (n = 11) in the LSC group and 84.6% (n = 11) in the ASC group (p = 0.686). Surgical failure for the apical compartment was also statistically comparable, with 12.5% (n = 2) in the LSC group and 0% (n = 0) in the ASC group (p = 0.186). Anatomical failure and prolapse beyond the hymen also showed the same results for both groups (p = 0.186 and p = 0.359 respectively for the apical compartment).
Last, Table 3 shows the reinterventions. In both groups five participants had surgical treatment, 22.7% in the LSC group and 26.3% in the ASC group (p = 0.729). Three patients in the LSC group and four patients in the ASC group underwent further surgery due to a bothersome cystocele or rectocele. One patient in the LSC group had de novo stress urine incontinence, for which she received a mid-urethral sling. Mean time to surgical reintervention (Fig. 2) was comparable in the two groups (LSC 41.2 months (SEM 22.7) versus ASC 55.8 months (SEM 13.5), p = 0.814). Two patients had surgery to remove the mesh, owing to severe complications. One patient presented with complaints of vaginal mesh exposure. The mesh got infected and extensive surgery was performed, 5.6 years (67 months) after she had undergone the ASC. During surgery it was discovered that the mesh fistulated through the vaginal vault. Adhesiolysis and resection of part of the ileum was performed. There was no descensus of the vaginal vault (POP-Q point C: −7) and an asymptomatic rectocele (POP-Q point Bp: 0) was left untreated. This surgery was otherwise uncomplicated and the patient made a good recovery. After 4 years, this patient had no POP-related complaints or pain. In the LSC group one patient also had a vaginal exposure and the mesh was infected. A robot-assisted procedure was performed to remove the mesh, 10.2 years (122 months) after she had undergone the LSC. The patient fully recovered from this complication. One patient from the ASC group had a diagnostic laparoscopy owing to complaints of abdominal pain. In each group, three patients were reported to have had pelvic floor physical therapy after the initial surgery (LSC 14.3% versus ASC 15.8%; p = 0.894). The initial sacrocolpopexy was without peri-operative complications for both patients.
Table 4 shows the mean POP-Q scores. Point C is at −4.7 in the LSC group (SD ± 3.9, range −8 to 8) and at −5.8 in the ASC group (SD ± 1.5, range −8 to −3), p = 0.353. The larger standard deviation is due to one patient in the LSC group, who had a stage 4 vaginal vault prolapse at long-term follow-up with “greatly bothersome” vaginal bulge symptoms.
Three mesh exposures and three suture exposures were described, and are shown in Table 5. Two mesh exposures, one in each group, were part of the complications described above. The other mesh exposure was in the LSC group and was left untreated, because it was only minor and without complaints. One patient in the LSC group and two patients in the ASC group had a suture exposure. The suture exposure for the patient in the LSC group was discovered at the follow-up visit for this study. She complained of vaginal blood loss and dyspareunia. After removal of this suture at the outpatient clinic she had no more complaints. In the ASC group, one suture exposure was discovered during an earlier visit of the patient to the outpatient clinic because of POP complaints, due to a rectocele. The suture was removed during subsequent vaginal surgery (posterior colporrhaphy). The suture exposure of the second patient in the ASC group was discovered by coincidence during vaginal examination for this follow-up study; the patient experienced no complaints and no treatment was performed.
Discussion
Main findings
This observational long-term follow-up study of a multicenter randomized controlled trial shows that there was no difference in disease-specific quality of life whether after laparoscopic or after abdominal sacrocolpopexy, with median scores of 0.0 (LSC: IQR 0–17; ASC: IQR 0–0) on the “genital prolapse” domain of the UDI in both groups (p = 0.175). This corresponds with our previously published SALTO trial and LAS trial, both comparing the laparoscopic and the abdominal procedure, with 1-year follow-up [10, 23].
Composite outcome of success, surgical failure, and anatomical failure were the same in both groups for all compartments. We found no relation between the type of surgery and the compartment of the recurrence. Also, no relation was found between the pre-operative POP-Q stage and the compartment of the recurrence. Some patients had a recurrence in the same compartment as they did pre-operatively; others did not.
In our study, mesh exposures were reported in 12.5% and 7.7% in the LSC and ASC groups respectively. A retrospective cohort study from 2019 reports exposure rates of 1.4% [24]. We expect this to be an underestimation of the exposure rate, as they detected only patients with bothersome exposures. Three prospective cohort studies reported an exposure rate of 2.9%, 3.7%, and 4.5%. These studies had a shorter follow-up time, median of 60 months (5 years) instead of the 109 months (9.1 years) in our study, which could explain why they reported lower exposure rates [25,26,27]. Three suture exposures were found in our study population. In the SALTO trial nonresorbable sutures were used, which might contribute to these exposures. Nowadays, it is common practice to use resorbable sutures, which might lead to fewer suture exposures [28]. There were no other surgery-related risk factors in our study population, such as concomitant hysterectomy [29].
Patient satisfaction on the PGI-I is 57.9% (n = 11) in the LSC group and 58.8% (n = 10) in the ASC group (p = 0.955). This seems lower than patient satisfaction reported in other long-term follow-up studies [27, 30]. These studies report trials with a median follow-up time of 5 and 6 years, compared with the 9 years of our follow-up. The lower satisfaction in our trial might be due to a longer period of follow-up. It is understandable that patients find it more difficult to compare their situation now and before surgery, solely considering POP complaints after a longer period of time. The PGI-I asks patients to describe their post-operative condition, compared with how it was before surgery. Perhaps this question was not specific enough for the participants. Moreover, the PGI-I was only validated for a follow-up duration of 12 months [19].
Strengths and limitations
We performed a randomized controlled trial, which is considered to yield the highest level of evidence when comparing two different treatment options. One of the main strengths of our study is the duration of follow-up, with a median of 109 months (9.1 years), which may be stated as “very long” (> 5 years) duration of follow-up, according to the IUGA/ICS joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse [13]. To our knowledge, there is no other comparative study with similar or longer duration of follow-up for the laparoscopic versus the open abdominal approach to sacrocolpopexy. Another strength of our study is that we reported on additional outcomes; such as combined outcome measure, objective outcome, and subjective outcome [14, 15]. By conforming to more commonly used clinical outcomes, our data are easy to interpret and could be used for meta-analyses in the future.
One of the limitations of our study is the relatively high rate of loss to follow-up. However, the statistical power remains >80% for the primary outcome measure disease-specific quality of life. From the 36 eligible patients in the LSC group, 14 patients (38.9%) were lost to follow-up, compared with 16 (45.7%) of the 35 eligible participants in the ASC group. Nine patients died and eight patients were not able to participate owing to old age or serious health issues, which was beyond our control. Perhaps the SARS-CoV-2 pandemic added to the loss to follow-up; however, we have no complete data on this matter. Other studies reported attrition rates of 46% at 5 years [31], rising to 62% at 7 years [6]. Loss to follow-up generally increases with review time [9]. Although we opted for a higher response rate, our loss to follow-up is not more than could be expected.
Most of our study population were postmenopausal and multiparous, with two or more vaginal births. This makes our results mainly applicable for patients with comparable characteristics.
Interpretation
The laparoscopic approach to sacrocolpopexy is preferable, compared with the open abdominal technique, mainly because of better short-term outcomes. The laparoscopic approach has less blood loss and a shorter hospital stay [10, 32]. Functional outcomes, complications, and retreatment were comparable for both techniques [10, 23, 32]. After a median follow-up of 109 months (9.1 years) the results are in line with the results after short-term follow-up. Therefore, laparoscopic sacrocolpopexy proves to be an effective and safe treatment for vaginal vault prolapse. More is known about patient-related and surgery-related risk factors for developing mesh exposure after sacrocolpopexy. Patients should be counseled accordingly and gynecologists should consider adjusting their technique to minimize the risk of mesh-related complications [29, 33]. LSC is a difficult procedure with a long learning curve; therefore, we believe this surgery should be performed by experienced surgeons and centralized care is preferable when the volumes are low.
Conclusion
At long-term follow-up there was no substantial difference in disease-specific quality of life, anatomical results on the POP-Q, complications as mesh or suture erosions, and reinterventions between the LSC and the ASC groups. Therefore, the laparoscopic approach of sacrocolpopexy is preferable, considering the previously discovered advantages in the short term.
References
Vermeulen CKM, Veen J, Adang C, van Leijsen SAL, Coolen ALWM, Bongers MY. Pelvic organ prolapse after laparoscopic hysterectomy compared with vaginal hysterectomy: the POP-UP study. Int Urogynecol J. 2021;32(4):841–50. https://doi.org/10.1007/s00192-020-04591-z.
Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol. 1997;104(5):579–85. https://doi.org/10.1111/j.1471-0528.1997.tb11536.x.
Marchionni M, Bracco GL, Checcucci V, Carabaneanu A, Coccia EM, Mecacci F, et al. True incidence of vaginal vault prolapse. Thirteen years of experience. J Reprod Med. 1999;44(8):679–84.
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004;104(4):805–23. https://doi.org/10.1097/01.AOG.0000139514.90897.07.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;4:CD004014. https://doi.org/10.1002/14651858.CD004014.pub5.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–24. https://doi.org/10.1001/jama.2013.4919.
Ganatra AM, Rozet F, Sanchez-Salas R, Barret E, Galiano M, Cathelineau X, et al. The current status of laparoscopic sacrocolpopexy: a review. Eur Urol. 2009;55(5):1089–103. https://doi.org/10.1016/j.eururo.2009.01.048.
Hilger WS, Poulson M, Norton PA. Long-term results of abdominal sacrocolpopexy. Am J Obstet Gynecol. 2003;189(6):1606–10; discussion 1610–1. https://doi.org/10.1016/j.ajog.2003.10.689.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016;10:CD012376. https://doi.org/10.1002/14651858.CD012376.
Coolen ALWM, van Oudheusden AMJ, Mol BWJ, van Eijndhoven HWF, Roovers JPWR, Bongers MY. Laparoscopic sacrocolpopexy compared with open abdominal sacrocolpopexy for vault prolapse repair: a randomised controlled trial. Int Urogynecol J. 2017;28(10):1469–79. https://doi.org/10.1007/s00192-017-3296-5.
Coolen ALWM, van Oudheusden AMJ, van Eijndhoven HWF, van der Heijden TP, Stokmans RA, Mol BWJ, et al. A comparison of complications between open abdominal sacrocolpopexy and laparoscopic sacrocolpopexy for the treatment of vault prolapse. Obstet Gynecol Int. 2013;2013:528636. https://doi.org/10.1155/2013/528636.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. https://doi.org/10.1136/bmj.c332.
Toozs-Hobson P, Freeman R, Barber M, Maher C, Haylen B, Athanasiou S, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Int Urogynecol J. 2012;23(5):527–35. https://doi.org/10.1007/s00192-012-1726-y.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–90. https://doi.org/10.1007/s00192-013-2169-9.
Barber MD, Brubaker L, Nygaard I, Wheeler TL 2nd, Schaffer J, Chen Z, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9. https://doi.org/10.1097/AOG.0b013e3181b2b1ae.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7. https://doi.org/10.1016/s0002-9378(96)70243-0.
Van der Vaart CH, de Leeuw JR, Roovers JP, Heintz AP. Measuring health-related quality of life in women with urogenital dysfunction: the Urogenital Distress Inventory and Incontinence Impact Questionnaire revisited. Neurourol Urodyn. 2003;22(2):97–104. https://doi.org/10.1002/nau.10038.
Roovers JP, van der Bom JG, van der Vaart CH, Heintz AP. Prediction of findings at defecography in patients with genital prolapse. BJOG. 2005;112(11):1547–53. https://doi.org/10.1111/j.1471-0528.2005.00734.x.
Srikrishna S, Robinson D, Cardozo L. Validation of the Patient Global Impression of Improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–8. https://doi.org/10.1007/s00192-009-1069-5.
t Hoen LA, Utomo E, Steensma AB, Blok BF, Korfage IJ. The Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12): validation of the Dutch version. Int Urogynecol J. 2015;26(9):1293–303. https://doi.org/10.1007/s00192-015-2692-y.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J. 2003;14(3):164–8. https://doi.org/10.1007/s00192-003-1063-2.
Roovers JP, van der Vaart CH, van der Bom JG, van Leeuwen JH, Scholten PC, Heintz AP. A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG 2004;111(1):50–6. doi:https://doi.org/10.1111/j.1471-0528.2004.00001.x
Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L, Moran P, et al. A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J. 2013;24(3):377–84. https://doi.org/10.1007/s00192-012-1885-x.
Baines G, Price N, Jefferis H, Cartwright R, Jackson SR. Mesh-related complications of laparoscopic sacrocolpopexy. Int Urogynecol J. 2019;30(9):1475–81. https://doi.org/10.1007/s00192-019-03952-7.
Sarlos D, Kots L, Ryu G, Schaer G. Long-term follow-up of laparoscopic sacrocolpopexy. Int Urogynecol J. 2014;25(9):1207–12. https://doi.org/10.1007/s00192-014-2369-y.
Wagner L, Chevrot A, Llinares E, Costa P, Droupy S. Long-term anatomic and functional results of laparoscopic sacrocolpopexy: a prospective study. Int Urol Nephrol. 2019;51(5):795–802. https://doi.org/10.1007/s11255-019-02124-2.
Illiano E, Giannitsas K, Zucchi A, Di Biase M, Del Zingaro M, Bini V, et al. Sacrocolpopexy for posthysterectomy vaginal vault prolapse: long-term follow-up. Int Urogynecol J. 2016;27(10):1563–9. https://doi.org/10.1007/s00192-016-2998-4.
Reisenauer C, Andress J, Schoenfisch B, Huebner M, Brucker SY, Lippkowski A, et al. Absorbable versus non-absorbable sutures for vaginal mesh attachment during sacrocolpopexy: a randomized controlled trial. Int Urogynecol J. 2022;33(2):411–9. https://doi.org/10.1007/s00192-021-04853-4.
Durst PJ, Heit MH. Polypropylene mesh predicts mesh/suture exposure after sacrocolpopexy independent of known risk factors: a retrospective case-control study. Female Pelvic Med Reconstr Surg. 2018;24(5):360–6. https://doi.org/10.1097/spv.0000000000000452.
Nightingale G, Phillips C. Long-term safety and efficacy of laparoscopically placed mesh for apical prolapse. Int Urogynecol J. 2021;32(4):871–7. https://doi.org/10.1007/s00192-020-04374-6.
Tate SB, Blackwell L, Lorenz DJ, Steptoe MM, Culligan PJ. Randomized trial of fascia lata and polypropylene mesh for abdominal sacrocolpopexy: 5-year follow-up. Int Urogynecol J. 2011;22(2):137–43. https://doi.org/10.1007/s00192-010-1249-3.
De Gouveia De Sa M, Claydon LS, Whitlow B, Dolcet Artahona MA. Laparoscopic versus open sacrocolpopexy for treatment of prolapse of the apical segment of the vagina: a systematic review and meta-analysis. Int Urogynecol J. 2016;27(1):3–17. https://doi.org/10.1007/s00192-015-2765-y.
Deblaere S, Hauspy J, Hansen K. Mesh exposure following minimally invasive sacrocolpopexy: a narrative review. Int Urogynecol J. 2022. https://doi.org/10.1007/s00192-021-04998-2.
Author information
Authors and Affiliations
Contributions
Anique M.J. van Oudheusden: project development, data analysis, manuscript writing; Josephine Eissing: data collection, manuscript writing; Ivon M. Terink: project development, data collection, manuscript editing; Maarten D.H. Vink: data collection, manuscript editing; Sander M.J. van Kuijk: data analysis, manuscript editing; Marlies Y. Bongers: project development, manuscript editing; Anne-Lotte W.M. Coolen: project development, manuscript editing
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Oudheusden, A.M.J., Eissing, J., Terink, I.M. et al. Laparoscopic sacrocolpopexy versus abdominal sacrocolpopexy for vaginal vault prolapse: long-term follow-up of a randomized controlled trial. Int Urogynecol J 34, 93–104 (2023). https://doi.org/10.1007/s00192-022-05350-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05350-y