Abstract
Introduction and hypothesis
Reliable risk factors for persistent urgency following pelvic organ prolapse (POP) surgery are still unclear. We aimed to identify preoperative parameters related to persistent postoperative urgency in a cohort of women following surgery for POP stage 3-4 with concomitant overactive bladder (OAB).
Methods
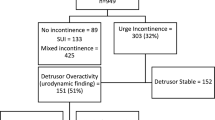
In this retrospective analysis, women with POP stage 3–4 and OAB who underwent POP repair during November 2012–December 2020 were included. Preoperative evaluation included history, Pelvic Organ Prolapse Quantification (POP-Q), multi-channel urodynamic studies and Pelvic Floor Distress Inventory (PFDI-20). Surgical procedures included: anterior and posterior colporrhaphy, sacrospinous ligament suspension, anterior vaginal wall mesh repair and robotic-assisted laparoscopic sacrocolpopexy. At the 12-month follow-up, urogynecological history, POP-Q evaluation, cough stress test and the PFDI-20 questionnaire were repeated.
Results
One hundred seventy-three patients were included in the analysis. Resolution of urgency was observed in 56% of women. Variables associated with persistent postoperative urgency included body mass index (BMI) (27 kg/m2 vs 25.7 kg/m2, p = 0.04), preoperative increased daytime frequency (46.39% vs 61.84%, p = 0.05), urgency urinary incontinence (UUI) (51.46% vs 80.26%, p = 0.0001), detrusor overactivity (DO) (40.2% vs 61.84%, p = 0.009) and lower maximum flow rate on UDS (13.9 ml/s vs 15 ml/s, p = 0.04). Multivariate analysis confirmed preoperative DO (OR: 12.2 [95% CI: 1.4–16.6]; p = 0.01), preoperative UUI (OR 3.8 [95% CI: 1.3–11.0]; p = 0.008) and BMI > 25 kg/m2 (OR 1.8 [95% CI: 1.1–7.2]; p = 0.04) as predictive factor for persistent urgency.
Conclusions
In women with advanced POP and OAB, being overweight, preoperative UUI and DO are related to persistent postoperative urgency. These findings will guide our future preoperative counseling and reinforce the role of UDS in POP management.

Similar content being viewed by others
References
Irwin DE, Milsom I, Hunskaar S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–14; discussion 1314-1315. https://doi.org/10.1016/j.eururo.2006.09.019.
Handa VL, Garrett E, Hendrix S, et al. Progression and remission of pelvic organ prolapse: A longitudinal study of menopausal women. Am J Obstet Gynecol. 2004;190:27–32. https://doi.org/10.1016/j.ajog.2003.07.017.
Hendrix SL, Clark A, Nygaard I, et al. Pelvic organ prolapse in the women’s health initiative: Gravity and gravidity. Am J Obstet Gynecol. 2002;186:1160–6. https://doi.org/10.1067/mob.2002.123819.
Wu JM, Vaughan CP, Goode PS, et al. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstet Gynecol. 2014;123:141–8. https://doi.org/10.1097/AOG.0000000000000057.
Rortveit G, Brown JS, Thom DH, et al. Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol. 2007;109:1396–403. https://doi.org/10.1097/01.AOG.0000263469.68106.90.
Karjalainen PK, Tolppanen A-M, Mattsson NK, et al. Pelvic organ prolapse surgery and overactive bladder symptoms—a population-based cohort (FINPOP). Int Urogynecol J. 2022;33:95–105. https://doi.org/10.1007/s00192-021-04920-w.
Johnson JR, High RA, Dziadek O, et al. Overactive bladder symptoms after pelvic organ prolapse repair. Female Pelvic Med Reconstr Surg. 2020;26:742–5. https://doi.org/10.1097/SPV.0000000000000700.
Miranne JM, Lopes V, Carberry CL, Sung VW. The effect of pelvic organ prolapse severity on improvement in overactive bladder symptoms after pelvic reconstructive surgery. Int Urogynecol J. 2013;24:1303–8. https://doi.org/10.1007/s00192-012-2000-z.
Otsuka A, Watanabe K, Matsushita Y, et al. Predictive factors for persistence of preoperative overactive bladder symptoms after transvaginal mesh surgery in women with pelvic organ prolapse. Lower Urinary Tract Symptoms. 2020;12:167–72. https://doi.org/10.1111/luts.12299.
Long C-Y, Hsu C-S, Wu M-P, et al. Predictors of improved overactive bladder symptoms after transvaginal mesh repair for the treatment of pelvic organ prolapse: Predictors of improved OAB after POP repair. Int Urogynecol J. 2011;22:535–42. https://doi.org/10.1007/s00192-010-1312-0.
Nguyen JK, Bhatia NN. Resolution of motor urge incontinence after surgical repair of pelvic organ prolapse. J Urol. 2001;166:2263–6.
Fletcher SG, Haverkorn RM, Yan J, et al. Demographic and urodynamic factors associated with persistent OAB after anterior compartment prolapse repair: Persistence of OAB symptoms after AVP repair. Neurourol Urodyn. 2010;29:1414–8. https://doi.org/10.1002/nau.20881.
Serati M, Giarenis I, Meschia M, Cardozo L. Role of urodynamics before prolapse surgery. Int Urogynecol J. 2015;26:165–8. https://doi.org/10.1007/s00192-014-2534-3.
Araki I, Haneda Y, Mikami Y, Takeda M. Incontinence and detrusor dysfunction associated with pelvic organ prolapse: clinical value of preoperative urodynamic evaluation. Int Urogynecol J. 2009;20:1301–6. https://doi.org/10.1007/s00192-009-0954-2.
Lee DM, Ryu YW, Lee YT, et al. A predictive factor in overactive bladder symptoms improvement after combined anterior vaginal wall prolapse repair: A pilot study. Korean J Urol. 2012;53:405. https://doi.org/10.4111/kju.2012.53.6.405.
Solomon E, Yasmin H, Duffy M, et al. Developing and validating a new nomogram for diagnosing bladder outlet obstruction in women. Neurourol Urodyn. 2018;37:368–78. https://doi.org/10.1002/nau.23307.
Abrams (1999) Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding function: DISCUSSION PAPER. BJU Int 84:14–15. https://doi.org/10.1046/j.1464-410x.1999.00121.x
Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7. https://doi.org/10.1016/s0002-9378(96)70243-0.
Haylen BT, de Ridder D, Freeman RM, et al. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodynamics n/a-n/a. 2009. https://doi.org/10.1002/nau.20798.
de Boer TA, Kluivers KB, Withagen MIJ, et al. Predictive factors for overactive bladder symptoms after pelvic organ prolapse surgery. Int Urogynecol J. 2010;21:1143–9. https://doi.org/10.1007/s00192-010-1152-y.
Digesu GA, Chaliha C, Salvatore S, et al. The relationship of vaginal prolapse severity tosymptoms and quality of life. BJOG:An Int J O&G. 2005;112:971–6. https://doi.org/10.1111/j.1471-0528.2005.00568.x.
Abrar S, Rizvi RM, Zahid N. The association of symptoms of overactive bladder with pelvic organ prolapse and its improvement after pelvic reconstructive surgery. Pak. J Med Sci. 2021;37. https://doi.org/10.12669/pjms.37.3.3312.
Kim MS, Lee GH, Na ED, et al. The association of pelvic organ prolapse severity and improvement in overactive bladder symptoms after surgery for pelvic organ prolapse. Obstet Gynecol Sci. 2016;59:214. https://doi.org/10.5468/ogs.2016.59.3.214.
Fry CH. Obesity and the overactive bladder. Curr Bladder Dysfunct Rep. 2013;8:62–8. https://doi.org/10.1007/s11884-012-0172-5.
Elbaset MA, Taha D-E, Sharaf DE, et al. Obesity and overactive bladder: Is it a matter of body weight, fat distribution or function? A preliminary result. Urology. 2020;143:91–6. https://doi.org/10.1016/j.urology.2020.04.115.
Liu R-T, Chung M-S, Lee W-C, et al. Prevalence of overactive bladder and associated risk factors in 1359 patients with type 2 diabetes. Urology. 2011;78:1040–5. https://doi.org/10.1016/j.urology.2011.05.017.
Richter HE, Creasman JM, Myers DL, et al. Urodynamic characterization of obese women with urinary incontinence undergoing a weight loss program: the Program to Reduce Incontinence by Diet and Exercise (PRIDE) trial. Int Urogynecol J. 2008;19:1653–8. https://doi.org/10.1007/s00192-008-0694-8.
Uzun H, Zorba OÜ. Metabolic syndrome in female patients With overactive bladder. Urology. 2012;79:72–5. https://doi.org/10.1016/j.urology.2011.08.050.
Leiria LO, Sollon C, Báu FR, et al. Insulin relaxes bladder via PI3K/AKT/eNOS pathway activation in mucosa: unfolded protein response-dependent insulin resistance as a cause of obesity-associated overactive bladder: Insulin relaxes bladder via PI3K/AKT/eNOS pathway. J Physiol. 2013;591:2259–73. https://doi.org/10.1113/jphysiol.2013.251843.
Leiria LO, Silva FH, Davel APC, et al. The soluble guanylyl cyclase activator BAY 60-2770 ameliorates overactive bladder in obese mice. J Urol. 2014;191:539–47. https://doi.org/10.1016/j.juro.2013.09.020.
Basu M, Duckett J. Effect of prolapse repair on voiding and the relationship to overactive bladder and detrusor overactivity. Int Urogynecol J. 2009;20:499–504. https://doi.org/10.1007/s00192-009-0807-z.
Lindsay J, Solomon E, Nadeem M, et al. Treatment validation of the Solomon-Greenwell nomogram for female bladder outlet obstruction. Neurourol Urodyn. 2020;39:1371–7. https://doi.org/10.1002/nau.24347.
Harrison SCW, Hunnam GR, Farman P, et al. Bladder instability and denervation in patients with bladder outflow obstruction. Br J Urol. 1987;60:519–22. https://doi.org/10.1111/j.1464-410X.1987.tb05033.x.
Harrison SCW, Ferguson DR, Doyle PT. Effect of bladder outflow obstruction on the innervation of the rabbit urinary bladder. Br J Urol. 1990;66:372–9. https://doi.org/10.1111/j.1464-410X.1990.tb14957.x.
Ferguson DR, Kennedy I, Burton TJ. ATP is released from rabbit urinary bladder epithelial cells by hydrostatic pressure changes-possible sensory mechanism? J Physiol. 1997;505:503–11. https://doi.org/10.1111/j.1469-7793.1997.503bb.x.
Yoshida M, Inadome A, Maeda Y, et al. Non-neuronal cholinergic system in human bladder urothelium. Urology. 2006;67:425–30. https://doi.org/10.1016/j.urology.2005.08.014.
Frigerio M, Manodoro S, Cola A, et al. Detrusor underactivity in pelvic organ prolapse. Int Urogynecol J. 2018;29:1111–6. https://doi.org/10.1007/s00192-017-3532-z.
Glass D, Lin FC, Khan AA, et al. Impact of preoperative urodynamics on women undergoing pelvic organ prolapse surgery. Int Urogynecol J. 2020;31:1663–8. https://doi.org/10.1007/s00192-019-04084-8.
Financial disclaimer
AP is currently board member of the International Society for the Study of Interstitial Cystitis (ESSIC)
MS is currently president of the European Urogynecological Association (EUGA)
Author information
Authors and Affiliations
Contributions
A. Padoa: protocol development; data collection, management and analysis; manuscript writing and editing
E. Levy: protocol development; data collection, management and analysis
T. Fligelman: protocol development; data collection, management and analysis; manuscript editing
R. Tomashev-Dinkovich: data collection
A. Tsviban: data collection
M. Serati: protocol development; data management and analysis; manuscript editing
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Maurizio Serati is President of the European Urogyneclogical Association (EUGA)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Padoa, A., Levy, E., Fligelman, T. et al. Predictors of persistent overactive bladder following surgery for advanced pelvic organ prolapse. Int Urogynecol J 34, 759–767 (2023). https://doi.org/10.1007/s00192-022-05313-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05313-3