Abstract
Introduction and aim
Observational studies have associated oral anticholinergic medications for overactive bladder (OAB) with cognitive impairment. This is the first pilot trial to compare the effects of two classes of OAB medications on brain activity in women. We evaluated the effect of anticholinergic versus non-anticholinergic (Non-Ach) interventions on regional brain activation during a cognitive task.
Methods
Twelve cognitively normal women seeking OAB therapy were recruited to a randomized, double-blind, parallel, controlled pilot trial. Whole-brain regional activity at baseline and 29 ± 1 days postintervention was assessed with functional magnetic resonance imaging during a working memory task. Average activation strength by region was compared after anticholinergic, beta-3 agonist, or placebo. Two-way ANOVA compared effects of group and time on average activation strength in anticholinergic versus Non-Ach (beta-3 agonists or placebo) groups.
Results
The mean (SD) age and body mass index of 12 women were 61 (7) years and 36 (7) kg/m2. Baseline depression and learning scores differed in the anticholinergic group (n = 3) versus the Non-Ach group (n = 9). Right mamillary body activation postintervention was higher after Non-Ach exposure (F 4.9, p < 0.04). In the full sample of participants at follow-up, there was less activation of the right middle frontal gyrus (p = 0.02), superior frontal gyrus (p < 0.01), and supramarginal (p < 0.01) gyrus.
Conclusion
Activation strength in brain regions underlying working memory was lower over time, and recognition scores improved. A powered trial is needed to adequately evaluate for differential effects of OAB oral medications on regional brain activation.
Similar content being viewed by others
Introduction
Overactive bladder syndrome (OAB) is characterized by urinary urgency, usually with urinary frequency and nocturia, with or without urgency urinary incontinence [1]. OAB increases in prevalence with advanced age, and urgency urinary incontinence (UUI) is more prevalent in women [2, 3]. OAB symptoms have a negative effect on emotional well-being and activities of daily living such as work productivity and social and family relationships [2]. UUI is associated with numerous comorbid conditions and may be an early manifestation of declining cognitive function [4, 5].
Longitudinal studies have associated dementia with lower urinary tract symptoms such as urinary incontinence [5, 6]. In cross-sectional studies of community-dwelling older adults, those with OAB demonstrate inferior performance on tests of executive function [7, 8] compared to their peers with stress incontinence or no urinary complaints.
Conservative therapies including behavioral modifications, pelvic floor therapy, and oral medications are typical initial therapies for OAB. The widespread use of anticholinergic (Ach) oral medication for OAB has been challenged because of association with incident dementia in several longitudinal population-based studies [9,10,11]. Ach oral medications for bladder indications increased odds of dementia compared to those for other indications [9, 10]. Other than oxybutynin specifically, the association of OAB Ach with short-term cognitive effects has not been demonstrated consistently [11]. The newer β-3 adrenergic agonist (β3) medications are similar in efficacy without known short- or long-term cognitive effects [12, 13].
Biomarkers of OAB and UUI are present in functional neuroimaging studies of brain activity and functional connectivity [13]. Similarly, biomarkers of cognitive impairment have been identified with functional magnetic resonance imaging (fMRI) [14]. The effect of the Ach oral medications on brain activity has not been compared to β3 oral medications or placebo. This study aims to evaluate the effect of short-term exposure to Ach OAB medication on regional brain activity during a working memory task in older women. We hypothesized activation of regions involved in working memory will be lower after Ach exposure compared to placebo or β3.
Methods
Patient selection and enrollment
This registered clinical trial (NCT03817931, clinicaltrials.gov) was initiated in August 2019 with a randomized, parallel, controlled trial. The study was approved by the Baylor Scott and White (#160362), Houston Methodist Research Institute (#Pro00019252) institutional review boards. Recruitment took place from September 2019 through July 2020. The SARS COVID-19 pandemic presented persistent barriers to recruitment starting in March 2020; thus, subject recruitment was discontinued before meeting goals in the original published protocol [15]. English-speaking women ages 50 to 90 years of age seeking therapy from community urology and urogynecology clinics were recruited and screened for eligibility. Exclusion criteria were voiding dysfunction (post-void residual volume ≥ 250 ml), neurogenic bladder, or positive screen for bladder pain syndrome. Per protocol, any recruits screening positive for mild cognitive impairment, severe depression, or severe anxiety were excluded. These screening criteria were defined as Montreal Cognitive assessment (MoCA) score ≤ 26, Patient Health Questionnaire-9 (PHQ9) score ≥ 14, and Hamilton Anxiety Assessment (HAMA) score ≥ 20, respectively. Patients with presence of a self-reported history of central neurologic conditions, stroke, pregnancy, use of medications, or pelvic floor therapy for OAB in the past 6 months were excluded. Patients with contraindications to MRI (metal implants, claustrophobia) or study medications were excluded.
After full informed consent and eligibility were confirmed, all participants were provided an informational handout on behavioral modifications and treatment options for OAB. Baseline data collection included validated questionnaires on OAB symptoms: The Patient Perception of Bladder Condition (PPBC), Overactive Bladder Questionnaire-Short Form including the Symptom Bother Score (SBS), and health-related quality of life score (QOL) were completed. Higher PPBC and QOL scores are indicative of improvement while higher SBS indicates worsening of symptoms. Subjects were instructed on how to complete a 24-h bladder diary prior to their baseline imaging. A health history questionnaire and review of all current medications were performed. Subjects were instructed to avoid any changes to their current medications during the study period.
Study aims
The primary aim of this study was to compare regional brain activity after Ach oral medication versus placebo and β3 medication. The secondary aim was to compare cognitive scores after exposure to Ach oral medication versus placebo and β3 medication. Prior to unmasking the study team to allocations, the investigators met to reach consensus on how to proceed with the most clinically relevant analysis given the early closure of this study. To evaluate the primary and secondary study aims, the decision was made to combine the β3 and placebo groups into a group titled “Non-Anticholinergic (Non-Ach)” for comparison to the Ach cohort.
Interventions
Baseline and postintervention imaging and questionnaires were completed at the Houston Methodist Hospital Translational Imaging Center. The day of baseline testing, patients received 30 capsules in a vial from the Investigational Drug Service pharmacy. Blinding to allocation and randomization was managed by an investigational drug pharmacy. To blind subjects and investigators to allocation, the Ach tablets and the β3 tablets as manufactured are placed intact within methylcellulose in an opaque locking gelatin capsule.
Subjects were randomized 1:1:1 to receive 29 ± 1 days of intervention with Ach (solifenacin 5 mg), β3 (mirabegron 25 mg), or placebo. Participants received standardized counseling on lifestyle modifications and fluid management before randomization. Participants, investigators, and outcome assessors were blinded to allocation. Blinding was maintained until after recruitment and all data collection was complete. Subjects initiated their intervention (1 capsule daily for 29 ± 1 days) following the baseline imaging and cognitive testing.
Outcome assessment
The Rey Auditory Verbal Learning test (RAVLT) is a neuropsychological test widely used to assess cognition in pre-dementia and dementia conditions. RAVLT is sensitive to verbal memory deficits caused by a variety of neurological diseases causing cognitive impairment [16]. During the RAVLT, lists of 15 words are used to assess recognition, learning, and immediate and delayed recall. These raw scores were used to calculate the following summary scores: short-term retention (STR), long-term retention (LTR), learning over trials (LOT), and recognition percentage correct (Recog).
On the dates of imaging, a modification of the RAVLT test was completed where the recognition component was visual rather than auditory. Tests for recall and recognition of RAVLT word lists were performed prior to entering the scanner. Anatomic scans and resting state imaging were followed by a video providing non-verbal instructions for the delayed recognition task. The sequence for the RAVLT testing and imaging protocol is given in Fig. 1. Subjects were instructed to push a button with their dominant hand when they recognized a word from the trial lists. Each single word was displayed on the screen for 5 s. After 29 ± 1 days of the intervention, the same imaging and cognitive testing procedure was performed using different word lists from the RAVLT handbook.
Flow chart of the RAVLT and fMRI testing: After six recall trials, participants were positioned for fMRI. Anatomic and resting state images were acquired first. Next, the recognition trial was performed with a television screen displaying single words for 5 seconds each. Participants indicated word recognition by pushing a button. Intervening resting state periods were taken after every six words. This cycle was repeated five times for a total of thirty words
Data acquisition and image processing
Images were acquired in a 3.0-Tesla full-body scanner (Siemens MAGNETOM Vida) with a 20-channel head coil. The baseline and post-intervention sessions included the following scans: (1) three-dimensional T1-weighted MPRAGE structural scan (0.86 × 0.86 × 1.00 mm3 spatial resolution); (2) T2*-weighted blood oxygen level-dependent (BOLD) fMRI scans in resting state (TR = 2000 ms, TE = 30 ms, isotropic spatial resolution 2.98 mm) and then during the recognition task. Analysis of Functional NeuroImages (AFNI) software was used for fMRI data processing [17]. The imaging protocol included slice time correction, motion correction, spatial normalization to the Montreal Neurological Institute (MNI) template, and spatial smoothing using a 5-mm full-width-at-half-maximum Gaussian kernel. The resting-state fMRI time series were then temporally bandpass-filtered between 0.01 and 0.1 Hz. After spatial smoothing, individual fMRI activation maps were created using a generalized linear model in MNI space. An averaged group fMRI activation map during the recognition task was then created in which significantly activated voxels were identified using a Student’s t-test. The threshold for results was at an uncorrected p-value of 0.01, and statistical significance was assessed after correction for multiple comparisons at cluster level (corrected p < 0.05).
Statistical analysis
Baseline characteristics and questionnaire scores were described using mean [standard deviation (SD)], median [(interquartile range (IQR)], or number (%). Shapiro-Wilk test for normality was used to identify parametric and nonparametric characteristics and score data. Bivariate analysis compared characteristics with Fisher’s exact test and two-sample t-test or Mann-Whitney test for parametric and nonparametric data. Bladder symptom scores (SBS, QOL, PPBC) and cognitive scores (LOT, STR, LTR, Recog) were compared by two-way ANOVA to assess differences by group, time, and group:time. Group by time interactions were not explored further due the sample size.
Regarding the fMRI results, the mean and standard deviation of the activation strength were calculated for 154 regions. The average activation strength (AveAS) in each region was quantified as the average of the t-statistic within that region. Baseline regional AveAS were evaluated with two-sample t-tests for differences by group. Two-way ANOVA was used to explore differences in regional AveAS by group and by time using baseline AveAS as a covariate. Due to small sample sizes, correction for multiple comparisons was not pursued. P-values were reported with p < 0.05 defining the significance threshold. For the primary outcome measured (regional AveAS), F-statistics and p-values are reported for regions with a significant p-value (< 0.05) for time, group, or group by time effect. Statistical analysis was completed using RStudio 2021.09.1 © 2009-2021 RStudio, PBC.
Results
Fourteen women were recruited and consented (Fig. 2). Two women dropped out prior to randomization because of scheduling issues (2/14, 14%). Twelve participants were randomized to Ach (n = 3), β3 (n = 5), and placebo (n = 4). There was no post-randomization attrition, and data collection was complete except one missing daily void (n) on a participant’s bladder diary.
Flow chart of recruitment: 41 potential subjects were approached; 14 were screened for eligibility. All 14 were eligible and consented to the study. Dropout occurred in two subjects because of scheduling conflicts before randomization. The final analytic sample included the Ach (n = 3) and Non-Ach cohorts (n = 9)
Participants were a mean (SD) age of 61.6 (7) years and mean (SD) BMI of 36 (7). The ACB score was higher in the Ach group at study end [4 (2,5) vs 8 (4,9), p < 0.03]. Depression score (PHQ-9) was higher in the Non-Ach group [7 (3) vs 2 (2), p < 0.04]. Baseline learning over trials score was higher in the Ach group [16 (8) vs 29 (7), p < 0.04]. Scores on the HAMA and Montreal cognitive assessment did not differ in Ach versus Non-Ach. Cognitive scores (LTR, STR, Recog) did not differ at baseline. Table 1 shows the full list of descriptive statistics for other variables which did not significantly differ.
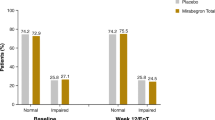
Cognitive scores and overactive bladder assessment comparisons
Descriptions of data and comparison over time of the Ach and Non-Ach groups are given in Table 2.. By two-way ANOVA, these measures did not differ by group at postintervention. In the overall sample, PPBC decreased from baseline to postintervention (F 7.1, p < 0.01). The recognition percentage correct (Rec%) increased from baseline to postintervention (F 6.4, p < 0.02). Of note, the final sample was not adequately powered to detect differences by group for PPBC and R or other variables.
Recognition task activation maps
During the recognition task, there was activation of the middle cingulate gyrus, supplemental motor area, inferior frontal gyrus, inferior parietal lobules, and angular gyrus. The right middle frontal gyrus was activated during this task. There was bilateral deactivation of the precuneus, precentral gyrus, paracentral gyrus, and rectal gyrus. Excerpts from activation maps in the sagittal and axial planes are presented in Fig. 3.
Activation maps show regions of significant signal change during the memory task. Activated: Superior frontal gyrus (SFG) and medial frontal gyrus (MFG), bilateral inferior frontal gyrus (L&R IFG), middle cingulate gyrus (MidCin), supplemental motor area (SMA), right middle frontal gyrus (r MFG). Deactivated: paracentral gyrus (PCG) and rectal gyrus (RG)
Primary comparison: anticholinergic versus non-anticholinergic
Baseline AveAS by region did not differ in women who received Ach (n = 3) versus Non-Ach (n = 9). Seven regions with a significant difference in AveAS by group, time, or group by time interaction (p < 0.05) are presented in Table 3.. There were 147/154 (95%) regions which did not demonstrate differences in AveAS by group, time, or group by time interaction (all p ≥ 0.05); thus, they are not listed in the table.
AveAS was lower from baseline to post-intervention in three distinct regions. This decreased response during the working memory task was found in the right middle frontal gyrus (F 6.3, p = 0.02), right superior frontal gyrus (F 7.9, p = 0.01), and right supramarginal gyrus (F 8.5, p = 0.008). There was a difference in AveAS by group in one region. The right mamillary body AveAS was lower in the Ach group (F 4.9, p < 0.04) compared to the Non-Ach group. Significant group by time interactions were found in the left amygdala (F 4.9, p = 0.04), left cerebellar lingual (F 7.6, p = 0.01), and left mamillary body (F 7.0, p = 0.02).
Discussion
Regional brain activation differed in the right mamillary body after Ach versus Non-Ach interventions. The sample of participants exposed to Ach was small, and group differences should be interpreted with caution. Activation in the right middle frontal gyrus, right superior frontal gyrus, and right supramarginal gyrus was lower in participants at follow-up. Scores on the recognition task (Recog) improved at the follow-up assessment.
At baseline, groups were similar except for a higher depression score (PHQ-9) in the Non-Ach group. All study participants scored a minimal to mild depression risk, so this is not likely of meaningful clinical significance. Baseline LOT scores in the Ach group at baseline were higher; however, over time the LOT scores did not differ in either group. There was improvement of patient’s perception of bladder condition in all participants at the follow-up visit without difference by groups.
The superior and middle frontal gyrus are implied in executive control and have roles in reorienting attention, impulse control, and language [18,19,20]. The supramarginal gyrus is in the inferior parietal lobule and has a role in visuospatial orientation and language processing [21]. Our findings of lower activation in these three regions with repetition of working memory tasks, further support existing literature. In a meta-analysis of 36 fMRI studies, working memory training (i.e., task repetition) was associated with decreased activity of the inferior parietal lobules, middle frontal gyri, and superior frontal gyri [22]. Our analysis of 12 participants showed less activation during a working memory task, specifically visual recognition, in the same three regions. Performance on most working memory domains (learning over trials, short- and long-term retention) did not change over time; however, recognition domain performance increased on repetition of memory testing. This study adds to the abundant literature on cognitive performance in the short term after solifenacin or mirabegron, which shows no negative effect [23, 24]. The task during imaging was a recognition task specifically; the increase in domain performance may be related to a short interval practice effect.
Though this study sample was too small to adequately assess group effects, there were trends with possible effect of anticholinergics on mamillary body activation. The mamillary bodies are thalamic nuclei with connections with the hippocampus and anterior thalamic nuclei [25]. Mamillary bodies are a part of the theorized circuit for working memory and as part of this circuit their primary function is in recollective memory [25].
Effects of Ach exposure on functional connectivity have been demonstrated after 1 year of exposure. Functional connectivity was decreased in the Ach exposure group, with a greater effect noted in adults with mild cognitive impairment [26]. Functional connectivity and regional activation have been associated with differences in the hippocampus, parahippocampus, and medial temporal gyrus across healthy adults versus cognitively impaired in systematic reviews and meta-analyses [14, 27, 28]. Those functional neuroimaging biomarkers are reflective of degeneration over years or decades. In contrast, our study population of women was cognitively normal at baseline screening and measured memory outcomes in the short term.
Strengths and limitations
This is the first pilot study to include neural correlates to a working memory after exposure to anticholinergic medication in women with OAB. The working memory task activated frontal and parietal regions and the cingulate gyrus as expected in whole-brain activation studies with visual recognition tasks [22, 27]. In short-term (< 1 year) clinical assessments of cognitive performance after oral OAB Ach, only oxybutynin has consistently shown a consistent negative effect [29]. Functional neuroimaging has reflected working memory clinical performance and changes after Ach exposure in general populations [26,27,28]. This RCT pilot achieved good participant retention and compliance, no adverse events, and maintained blinding of the participants and all assessors and may inform future studies adequately powered to detect differences in women with OAB.
There are several limitations of this pilot study; most apparent is the inadequate sample size, which poses a high risk of type I and type II error. Improvement of OAB measures did not differ by group or time in most measures. Symptom improvement (and activation outcome measures) could be affected by the combination of the β3 and placebo groups. All participants were uniformly counseled on behavioral modifications for OAB (including placebo group) upon study initiation; differences in implementation and other unmeasured psychosocial factors could influence symptoms and activation over time. This population included non-responding participants who may differ from women who are clinical responders; a longer exposure and flexible drug dosing may be beneficial in future investigations. The study duration of 1 month is brief but may reflect a common exposure period for many adults prescribed OAB medications. Prescription database literature indicates mean persistence of use of oral Ach is around 30–60 days [30]. Cognitive function is comprised of many domains: neuropsychiatric testing for attention, association, and processing speed was not assessed in this protocol. Future studies of cognitive effects may benefit from more extensive assessments and should be powered to detect differences across groups.
In conclusion, this pilot study presents a novel longitudinal evaluation of regional brain activation during a working memory task in OAB patients receiving oral medications. Cognitive changes are typically not detectable in short-term studies and may be difficult to detect in clinical settings. Detection of short-term effects, if present, may be detected through neural activity during a working memory task but larger studies are needed.
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26.
Coyne KS, Sexton CC, Irwin DE, et al. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional wellbeing in men and women: results from the EPIC study. BJU Int. 2008;101:1388–95.
Stewart WF, Van Rooyen JB, Cundiff GW, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327–36.
Coyne KS, Wein A, Nicholson S, et al. Comorbidities and personal burden of urgency urinary incontinence: a systematic review. Int J Clin Pract. 2013;67(10):1015–33.
Chiang CH, Wu MP, Ho CH, et al. Lower urinary tract symptoms are associated with increased risk of dementia among the elderly: a nationwide study. Biomed Res Int. 2015;2015:187819.
Grant RL, Drennan VM, Rait G, Petersen I, Iliffe S. First diagnosis and management of incontinence in older people with and without dementia in primary care: a cohort study using The Health Improvement Network primary care database. PLoS Med. 2013;10(8):e1001505.
Gibson W, Makhani A, Hunter KF, Wagg A. Do older adults with overactive bladder demonstrate impaired executive function compared to their peers without OAB? Can Geriatrics J. 2020;23(4):329–34.
Lussier M, Renaud M, Chiva-Razavi S, et al. Are stress and mixed urinary incontinence associated with impaired executive control in community-dwelling older women? J Clin Exp Neuropsychol. 2013;35(5):445–54.
Coupland CAC, Hill T, Dening T, Morriss R, Moore M, Hippisley-Cox J. Anticholinergic drug exposure and the risk of dementia: a nested case-control study. JAMA Intern Med. 2019;179(8):1084–93.
Gray SL, Anderson ML, Dublin S, et al. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med. 2015;175(3):401–7.
Welk B, Richardson K, Panicker JN. The cognitive effect of anticholinergics for patients with overactive bladder. Nature Reviews Urology. 2021;18(11):686–700.
Griebling TL, Compbell NL, Mangel J, et al. Effect of mirabegron on cognitive function in elderly patients with overactive bladder: MoCA results from a phase 4 randomized, placebo-controlled study (PILLAR). BMC Geriatr. 2020;20:109.
Griffiths D, Tadic SD, Schaefer W, Resnick NM. Cerebral control of the bladder in normal and urge-incontinent women. Neuroimage. 2007;37(1):1–7.
Terry DP, Sabatinelli D, Puente AN, et al. A meta-analysis of fMRI activation differences during episodic memory in Alzheimer’s disease and mild cognitive impairment. J Neuroimaging. 2015;25:849–60.
High RA, Danford JM, Shi Z, Karmonik C, Kuehl TJ, Bird ET, Khavari R. Protocol for a multicenter randomized, double blind, controlled pilot trial of higher neural function in overactive bladder patients after anticholinergic, beta-3 adrenergic agonist, or placebo. Contemp Clin Trials Commun. 2020;14(19):100621.
Schoenberg MR, Dawson KA, Duff K, Patton D, Scott JG, Adams RL. Test performance and classification statistics for the Rey auditory verbal learning test in selected clinical samples. Arch Clin Neuropsychol. 2006;21:693–703.
Gold S, Christian B, Arndt S, Zeien G, et al. Functional MRI statistical software packages: a comparative analysis. Hum Brain Mapp. 1998;6:73–84.
Hu S, Ide JS, Zhang S, Chiang-shan RL. The right superior frontal gyrus and individual variation in proactive control of impulsive response. J Neurosci. 2016;36(50):12688–96.
El-Baba RM, Schury MP. Neuroanatomy, Frontal Cortex. [Updated 2021 Jun 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
Reber J, Tranel D. The Frontal Lobes. Handb Clin Neurol. 2019;163:147–64.
Ben-Shabat E, Matyas TA, Pell GS, et al. The right supramarginal gyrus is important for proprioception in healthy and stroke-affected participants: a functional MRI study. Front Neurol. 2015;6:248.
Vartanian O, Replete V, Saint SA, et al. What is targeted when we train working memory? Evidence from a meta-analysis of the neural correlates of working memory training using activation likelihood estimation. Front Psychol. 2022;202213:868001.
Wagg A, Dale M, Tretter R, Stow B, Compion G. Randomised, multicentre, placebo- controlled, double blind crossover study investigating the effect of solifenacin and oxybutynin in elderly people with mild cognitive impairment: the SENIOR study. Eur Urol. 2013;64:74–81.
Griebling TL, Campbell NL, Mangel J, et al. Effect of mirabegron on cognitive function in elderly patients with overactive bladder: MoCA results from a phase 4 randomized, placebo-controlled study (PILLAR). BMC Geriatr. 2020;20(1):109.
Peterson DC, Reddy V, Mayes DA. Neuroanatomy, Mammillary Bodies. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-
Meng D, Mohammadi-Nejad AR, Sotiropoulos SN, Auer DP. Alzheimer's Disease Neuroimaging Initiative. Anticholinergic drugs and forebrain magnetic resonance imaging changes in cognitively normal people and those with mild cognitive impairment. Eur J Neurol. 2022;29(5):1344–53.
Chai WJ, Abd Hamid AI, Abdullah JM. Working memory from the psychological and neurosciences perspectives: a review. Front Psychol. 2018;27(9):401.
Bayram E, Caldwell JZK, Banks SJ. Current understanding of magnetic resonance imaging biomarkers and memory in Alzheimer's disease. Alzheimers Dement (N Y). 2018;14(4):395–413.
Welk B, Richardson K, Panicker JN. The cognitive effect of anticholinergics for patients with overactive bladder. Nat Rev Urol. 2021;18(11):686–700.
Linder BJ, Gebhart JB, Elliott DS, Van Houten HK, Sangaralingham LR, Habermann EB. National Patterns of filled prescriptions and third-line treatment utilization for privately insured women with overactive bladder. Female Pelvic Med Reconstructive Surg. 2021;27(2):e261–6.
Author information
Authors and Affiliations
Contributions
RA High: protocol development, statistical analysis, manuscript writing and reviewing
Z Shi: protocol development, statistical and image analysis
JM Danford protocol development, manuscript reviewing
ET Bird: protocol development, manuscript reviewing
C Karmonik: protocol development, analysis
R Khavari: protocol development, manuscript writing and reviewing
Corresponding author
Ethics declarations
Conflicts of interest
Rachel A. High: International Urogynecological Association Clinical Research Grant and a Baylor Scott and White Health Anderle Foundation grant supported work presented in this manuscript.
Zhaoyue Shi: none
Jill M Danford: none
Erin T Bird: none
Christof Karmonik: none
Rose Khavari: RK is partially supported by R03DK126994 and K23DK118209
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
High, R.A., Shi, Z., Danford, J.M. et al. The effect of oral medications on fMRI brain activation: A randomized, double blind, controlled pilot trial of older women with overactive bladder. Int Urogynecol J 34, 1035–1042 (2023). https://doi.org/10.1007/s00192-022-05300-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05300-8