Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) is a defect of the female pelvic floor. Stress urinary incontinence (SUI), urge urinary incontinence (UUI), and obstructive symptoms may occur in these patients. The objective of surgical treatment is to restore the anatomy and function of the pelvic floor; however, it may prompt urinary symptoms not present previously. We performed a systematic review and meta-analysis to determine urodynamic changes in patients undergoing surgical correction for POP.
Methods
PubMed and Cochrane databases were searched for studies that contained data from urodynamic evaluation before and after vaginal surgery for POP. The main urodynamic data collected were free uroflowmetry (maximum flow [Qmax], voided volume, and post-void residual volume [PVR]), cystometry (bladder capacity, presence of detrusor overactivity [DO], SUI or UUI, and Valsalva leak point pressure), and pressure × flow study (detrusor pressure at maximum flow [PdetQmax], Qmax, and PVR).
Results
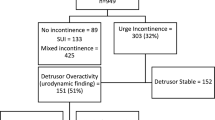
A total of 22 studies were included (1,549 women). Patients had a significantly higher prevalence of DO before surgery (OR = 1.56; 95% CI = 1.06–2.29), and surgeries without sling placement demonstrated a tendency to ameliorate DO. Patients who did not receive a sling were more incontinent after surgery. Bladder-emptying parameters improved after surgery, with higher PdetQmax before surgery (IV = 3.23; 95% CI = 0.45–1.18). Patients who did not receive MUS presented a lower Qmax (IV = −3.19; 95%CI = −4.09 to −2.30) and a higher PVR (IV = 27.89; 95%CI = 15.68–40.1) before surgery.
Conclusion
Correction surgery for POP yields better urodynamic emptying parameters, with a reduction in the prevalence of DO. In contrast, sling placement enhances obstructive parameters.






Similar content being viewed by others
Abbreviations
- CI:
-
Confidence intervals
- DO:
-
Detrusor overactivity
- LUTS:
-
Lower urinary tract symptoms
- MUS:
-
Mid-urethral sling
- PdetQmax:
-
Detrusor pressure at maximum flow
- PVR:
-
Post-void residual volume
- Qmax:
-
Maximum flow
- SUI:
-
Stress Urinary Incontinence
- UUI:
-
Urgency urinary incontinence
- VLPP:
-
Valsalva leak point pressure
References
Barber MD. Pelvic organ prolapse. BMJ. 2016;354:i3853. https://doi.org/10.1136/bmj.i3853.
Al-Mandeel H, Ross S, Robert M, Milne J. Incidence of stress urinary incontinence following vaginal repair of pelvic organ prolapse in objectively continent women. Neurourol Urodyn. 2011;30(3):390–4. https://doi.org/10.1002/nau.20947.
Kawasaki A, Corey EG, Laskey RA, Weidner AC, Siddiqui NY, Wu JM. Obesity as a risk for the recurrence of anterior vaginal wall prolapse after anterior colporrhaphy. J Reprod Med. 2013;58:195–9.
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185:1332–7; discussion 1337–8. https://doi.org/10.1067/mob.2001.119078.
Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183:277–85. https://doi.org/10.1067/mob.2000.107583.
Trowbridge ER, Fultz NH, Patel DA, DeLancey JO, Fenner DE. Distribution of pelvic organ support measures in a population-based sample of middle-aged, community-dwelling African American and white women in southeastern Michigan. Am J Obstet Gynecol. 2008;198:548.e1–6. https://doi.org/10.1016/j.ajog.2008.01.054.
NICE Guidance—Urinary incontinence and pelvic organ prolapse in women: management: © NICE. Urinary incontinence and pelvic organ prolapse in women: management. BJU Int. 2019;123:777–803. https://doi.org/10.1111/bju.14763.
Lensen EJ, Withagen MI, Kluivers KB, Milani AL, Vierhout ME. Urinary incontinence after surgery for pelvic organ prolapse. Neurourol Urodyn. 2013;32:455–9. https://doi.org/10.1002/nau.22327.
Baessler K, Christmann-Schmid C, Maher C, Haya N, Crawford TJ, Brown J. Surgery for women with pelvic organ prolapse with or without stress urinary incontinence. Cochrane Database Syst Rev. 2018;8:CD013108. https://doi.org/10.1002/14651858.CD013108.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. https://doi.org/10.1186/1471-2288-14-135.
Bump RC, Hurt WG, Theofrastous JP, Addison WA, Fantl JA, Wyman JF, et al. (1996) randomized prospective comparison of needle colposuspension versus endopelvic fascia plication for potential stress incontinence prophylaxis in women undergoing vaginal reconstruction for stage III or IV pelvic organ prolapse. The continence program for women research group. Am J Obstet Gynecol. 1996;175(2):326–33; discussion 333–5. https://doi.org/10.1016/s0002-9378(96)70142-4.
Ek M, Tegerstedt G, Falconer C, Kjaeldgaard A, Rezapour M, Rudnicki M, et al. Urodynamic assessment of anterior vaginal wall surgery: a randomized comparison between colporrhaphy and transvaginal mesh. Comparative study; journal article; multicenter study; randomized controlled trial. Neurourol Urodyn. 2010;29:527–31. https://doi.org/10.1002/nau.20811.
Natale F, La Penna C, Padoa A, Agostini M, Panei M, Cervigni M. High levator myorrhaphy versus uterosacral ligament suspension for vaginal vault fixation: a prospective, randomized study. Int Urogynecol J. 2010;21:515–22. https://doi.org/10.1007/s00192-009-1064-x.
Liang CC, Tseng LH, Lo TS, Lin YH, Lin YJ, Chang SD. Sexual function following outside-in transobturator midurethral sling procedures: a prospective study. Int Urogynecol J. 2012;23:1693–8. https://doi.org/10.1007/s00192-012-1792-1.
Lo TS, Bt Karim N, Cortes EFM, Wu PY, Lin YH, Tan YL. Comparison between Elevate anterior/apical system and Perigee system in pelvic organ prolapse surgery: clinical and sonographic outcomes. Int Urogynecol J. 2015;26:391–400. https://doi.org/10.1007/s00192-014-2492-9.
Long CY, Wang CL, Wu MP, Wu CH, Lin KL, Liu CM, et al. Comparison of clinical outcomes using "Elevate Anterior" versus "Perigee" system devices for the treatment of pelvic organ prolapse. Biomed Res Int. 2015;2015:479610.
Lo TS, Al-Kharabsheh AM, Tan YL, Pue LB, Hsieh WC, Uy-Patrimonio MC. Single incision anterior apical mesh and sacrospinous ligament fixation in pelvic prolapse surgery at 36 months follow-up. Taiwan J Obstet Gynecol. 2017;56:793–800. https://doi.org/10.1016/j.tjog.2017.10.016.
Bakas P, Papadakis E, Karachalios C, Beta A, Liapis A. Long-term efficacy follow-up of tension-free vaginal tape obturator in patients with stress urinary incontinence with or without cystocele. Int J Gynaecol Obstet. 2018;143:339–43. https://doi.org/10.1002/ijgo.12682.
Ker CR, Lin KL, Loo ZX, Juan YS, Long CY. Comparison of UpholdTM vaginal mesh procedure with hysterectomy or uterine preservation for the treatment of pelvic organ prolapse. Sci Rep. 2018;8:9438. https://doi.org/10.1038/s41598-018-27765-8.
Lo TS, Chua S, Kao CC, Hsieh WC, Wu MP, Tseng LH. Prophylactic midurethral sling insertion during transvaginal pelvic reconstructive surgery for advanced prolapse patients with high-risk predictors of postoperative de novo stress urinary incontinence. Int Urogynecol J. 2019;30:1541–9. https://doi.org/10.1007/s00192-018-3787-z.
Borstad E, Rud T. The risk of developing urinary stress-incontinence after vaginal repair in continent women. A clinical and urodynamic follow-up study. Acta Obstet Gynecol Scand. 1989;68:545–9.
Colakoğlu M, Capar M, Kiliç M, Colakoğlu U, Kaya H, Acar A. A new needle suspension procedure for genuine stress incontinence and anterior vaginal wall prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7:64–7; discussion 67–8. https://doi.org/10.1007/bf01902374.
Gordon D, Groutz A, Wolman I, Lessing JB, David MP. Development of postoperative urinary stress incontinence in clinically continent patients undergoing prophylactic Kelly plication during genitourinary prolapse repair. Neurourol Urodyn. 1999;18:193–7; discussion 197–8. https://doi.org/10.1002/(sici)1520-6777(1999)18:3<193::aid-nau5>3.0.co;2-e
Groutz A, Gordon D, Wolman I, Jaffa AJ, Kupferminc MJ, David MP, et al. The use of prophylactic Stamey bladder neck suspension to prevent post-operative stress urinary incontinence in clinically continent women undergoing genitourinary prolapse repair. Neurourol Urodyn. 2000;19:671–6. https://doi.org/10.1002/1520-6777(2000)19:6<671::aid-nau4>3.0.co;2-3
Gordon D, Gold RS, Pauzner D, Lessing JB, Groutz A. Combined genitourinary prolapse repair and prophylactic tension-free vaginal tape in women with severe prolapse and occult stress urinary incontinence: preliminary results. Urology. 2001;58:547–50. https://doi.org/10.1016/s0090-4295(01)01327-9.
Costantini E, Pajoncini C, Zucchi A, Lombi R, Bini V, Mearini E, et al. Four-corner colposuspension: clinical and functional results. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:113–8. https://doi.org/10.1007/s00192-002-1015-2.
Digesu GA, Salvatore S, Chaliha C, Athanasiou S, Milani R, Khullar V. Do overactive bladder symptoms improve after repair of anterior vaginal wall prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1439–43. https://doi.org/10.1007/s00192-007-0375-z.
Chin HY, Chiang CH, Lin KC, Wang CJ, Lee CL, Soong YK. Prospective assessment of overactive bladder symptoms in women who have undergone transvaginal surgery for advanced vaginal wall prolapse: a preliminary report. J Obstet Gynaecol Res. 2009;35:732–7. https://doi.org/10.1111/j.1447-0756.2008.00999.x.
Lakeman MM, Hakvoort RA, Van de Weijer EP, Emanuel MH, Roovers JP. Anterior colporrhaphy does not induce bladder outlet obstruction. Int Urogynecol J. 2012;23:723–8. https://doi.org/10.1007/s00192-012-1688-0.
Lo TS, Tan YL, Cortes EF, Pue LB, Wu PY, Al-Kharabsheh A. Anterior-apical single-incision mesh surgery (SIMS): surgical and functional outcomes at 1 year. J Minim Invasive Gynecol. 2015;22:50–6. https://doi.org/10.1016/j.jmig.2014.07.002.
Natale F, Costantini E, La Penna C, Illiano E, Balsamo R, Carbone A, Cervigni M. Trocar-guided trans-vaginal mesh surgery for pelvic organ prolapse: effects on urinary continence and anatomical and functional outcomes. A prospective observational study. Eur J Obstet Gynecol Reprod Biol. 2017;210:29–34. https://doi.org/10.1016/j.ejogrb.2016.10.052.
Sayed Ahmed WA, Taha OT, Hamdy MA, Ibrahim ZM, Elshahat AM. Bladder function after sacrospinous hysteropexy and vaginal wall repair in women with uterovaginal prolapse. Eur J Obstet Gynecol Reprod Biol. 2018;224:170–4. https://doi.org/10.1016/j.ejogrb.2018.03.041.
Wen L, Shek KL, Dietz HP. Changes in urethral mobility and configuration after prolapse repair. Ultrasound Obstet Gynecol. 2019;53:124–8. https://doi.org/10.1002/uog.19165.
Lo TS, Chua S, Uy-Patrimonio MC, Kao CC, Lin CH. Clinical outcomes of detrusor underactivity in female with advanced pelvic organ prolapse following vaginal pelvic reconstructive surgery. Neurourol Urodyn. 2018;37:2242–8. https://doi.org/10.1002/nau.23576.
Frigerio M, Manodoro S, Cola A, Palmieri S, Spelzini F, Milani R. Detrusor underactivity in pelvic organ prolapse. Int Urogynecol J. 2018;29:1111–6. https://doi.org/10.1007/s00192-017-3532-z.
Levin RM, Longhurst PA, Barasha B, McGuire EJ, Elbadawi A, Wein AJ. Studies on experimental bladder outlet obstruction in the cat: long-term functional effects. J Urol. 1992;148:939–43. https://doi.org/10.1016/s0022-5347(17)36782-4.
Dancz CE, Ozel B. Is there a pelvic organ prolapse threshold that predicts bladder outflow obstruction? Int Urogynecol J. 2011;22:863–8. https://doi.org/10.1007/s00192-011-1373-8.
Chang TC, Hsiao SM, Chen CH, Wu WY, Lin HH. Utilizing preoperative 20-minute pad testing with vaginal gauze packing for indicating concomitant midurethral sling during cystocele repair. Eur J Obstet Gynecol Reprod Biol. 2014;172:127–30. https://doi.org/10.1016/j.ejogrb.2013.10.008.
Ploeg JM, Rengerink KO, Steen A, Leeuwen JH, Vaart CH, Roovers JP. Vaginal prolapse repair with or without a midurethral sling in women with genital prolapse and occult stress urinary incontinence: a randomized trial. Int Urogynecol J. 2016;27:1029–38. https://doi.org/10.1007/s00192-015-2924-1.
Crescenze IM, Abraham N, Li J, Goldman HB, Vasavada S. Urgency incontinence before and after revision of a synthetic mid urethral sling. J Urol. 2016;196:478–83. https://doi.org/10.1016/j.juro.2016.01.091.
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. Continence program for women research group. Neurourol Urodyn. 1995;14:131–9. https://doi.org/10.1002/nau.1930140206.
Shoureshi PS, Lee W, Kobashi KC, Sajadi KP. Media coverage of the 2019 United States Food and Drug Administration ordered withdrawal of vaginal mesh products for pelvic organ prolapse. Int Urogynecol J. 2021;32:375–9. https://doi.org/10.1007/s00192-020-04401-6.
Author information
Authors and Affiliations
Contributions
H.O.D. Santos: project conceptualization and development, data extraction/analysis, data curation, visualization, manuscript writing/editing; D.B. Lourenço: project conceptualization and development, data extraction/analysis, data curation, visualization, manuscript writing/editing; A.D. Partezani: data extraction/analysis and manuscript editing; S.B. Teles: data extraction/analysis and manuscript editing; B. Bianco: resources, manuscript review and editing; L.A.S. Rios: visualization, manuscript review and editing; G.C. Lemos: resources, supervision, manuscript review, and editing; A. Carneiro: project conceptualization, supervision and administration, resources, manuscript writing/editing. All authors critically reviewed the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Supplementary information

Supplementary Fig. 1
UDI-6 questionnaire scores before and after surgery for correction of pelvic organ prolapse with or without sling placement (PNG 156 kb)
Supplementary Table 1
(DOCX 30 kb)
Rights and permissions
About this article
Cite this article
Lourenço, D.B., Duarte-Santos, H.O., Partezani, A.D. et al. Urodynamic profile of voiding in patients with pelvic organ prolapse after surgery: a systematic review with meta-analysis. Int Urogynecol J 34, 53–65 (2023). https://doi.org/10.1007/s00192-022-05086-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05086-9