Abstract
Introduction and hypothesis
Labor is a known risk factor for pelvic floor dysfunction (PFD); however, the impact of operative vaginal delivery (OVD), particularly spatulas, remains unclear. The aim of this study was to compare postpartum PFD symptoms in women undergoing spontaneous vaginal delivery (SVD) and those undergoing OVD.
Methods
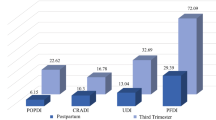
An observational prospective study (MOODS: Maternal-neonatal Outcomes in Operative Vaginal Delivery) was enrolled at Hospital de Braga from February to October 2018. All singleton term OVD (Thierry spatulas and vacuum extractor) and a convenience SVD sample were recruited, in a 2:1 ratio. To assess PFD symptoms Pelvic Floor Distress Inventory-20 (PFDI-20) was applied at 3, 6, and 12 months postpartum. The questionnaire is divided into three subscales: Urinary (UDI), Colorectal-Anal (CRADI), and Pelvic Organ Prolapse Distress Inventory (POPDI).
Results
Of the 304 women recruited, 207 were included, 34.3% with SVD and 65.7% with OVD. Thierry spatulas were used in 53.7% of women undergoing OVD. Frequency of nulliparous (p < 0.001), episiotomy (p < 0.001), neuraxial anesthesia (p < 0.001), postpartum pain (p = 0.001) and occiput-posterior fetal position (p < 0.001) were significantly higher in OVD. Second phase of labor duration was longer in OVD (p = 0.001). At 3 months postpartum, women undergoing OVD and spatula-assisted delivery had higher UDI score, POPDI score, and global score, with no differences at 6 months and 1 year. After controlling for confounding variables, OVD and spatulas were still associated with greater POPDI scores at 3 months postpartum.
Conclusions
Operative vaginal delivery, particularly with spatulas, seems to be associated with a higher prevalence of early PFD symptoms, mainly regarding pelvic organ prolapse.

Similar content being viewed by others
References
Bo K, Frawley HC, Haylen BT, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J. 2017;28:191–213. https://doi.org/10.1007/s00192-016-3123-4.
Dolan LM, Hilton P. Obstetric risk factors and pelvic floor dysfunction 20 years after first delivery. Int Urogynecol J. 2010;21:535–44. https://doi.org/10.1007/s00192-009-1074-8.
Torrisi G, Minini G, Bernasconi F, Perrone A, Trezza G, Guardabasso V, Ettore G. A prospective study of pelvic floor dysfunctions related to delivery. Eur J Obstet Gynecol Reprod Biol. 2012;160(1):110–5. https://doi.org/10.1016/j.ejogrb.2011.10.010.
Durnea CM, Khashan AS, Kenny LC, Durnea UA, Dornan JC, O’Sullivan SM, O’Reilly BA. What is to blame for postnatal pelvic floor dysfunction in primiparous women—pre-pregnancy or intrapartum risk factors? Eur J Obstet Gynecol Reprod Biol. 2017;214:36–43. https://doi.org/10.1016/j.ejogrb.2017.04.036.
Memon H, Handa VL. Pelvic floor disorders following vaginal or cesarean delivery. Curr Opin Obstet Gynecol. 2012;24(5):349–54. https://doi.org/10.1097/GCO.0b013e328357628b.
O'Mahony F, Hofmeyr GJ, Menon V. Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev. (11):CD005455. 2010. https://doi.org/10.1002/14651858.CD005455.pub2.
Rørtveit G, Hannestad YS. Association between mode of delivery and pelvic floor dysfunction. Tidsskr Nor Laegeforen. 2014;134(19):1848–52. https://doi.org/10.4045/tidsskr.13.0860.
Urbankova I, Grohregin K, Hanacek J, Krcmar M, Feyereisl J, Deprest J, Krofta L. The effect of the first vaginal birth on pelvic floor anatomy and dysfunction. Int Urogynecol J. 2019;30:1689–96. https://doi.org/10.1007/s00192-019-04044-2.
ACOG. Practice bulletin no. 219: operative vaginal delivery. Obstet Gynecol. 2020;135(4):e151.
Colla C, Paiva LL, Ferla L, Trento MJB, de Vargas IMP, Dos Santos BA, Ferreira CF, Ramos JGL. Pelvic floor dysfunction in the immediate puerperium, and 1 month and 3 months after vaginal or cesarean delivery. Int J Gynaecol Obstet. 2018;143(1):94–100. https://doi.org/10.1002/ijgo.12561.
Fitzpatrick M, Behan M, O'Connell PR, O'Herlihy C. Randomised clinical trial to assess anal sphincter function following forceps or vacuum assisted vaginal delivery. BJOG. 2003;110(4):424–9. https://doi.org/10.1046/j.1471-0528.2003.02173.x.
Handa VL, Blomquist JL, Knoepp LR, Hoskey KA, McDermott KC, Muñoz A. Pelvic floor disorders 5–10 years after vaginal or cesarean childbirth. Obstet Gynecol. 2011;118(4):777–84. https://doi.org/10.1097/AOG.0b013e3182267f2f.
Deane RP. Operative vaginal delivery and pelvic floor complications. Best Pract Res Clin Obstet Gynaecol. 2019;56:81–92. https://doi.org/10.1016/j.bpobgyn.2019.01.013.
Johanson RB, Heycock E, Carter J, Sultan AH, Walklate K, Jones PW. Maternal and child health after assisted vaginal delivery: five-year follow up of a randomised controlled study comparing forceps and ventouse. BJOG. 1999;106(6):544–9. https://doi.org/10.1111/j.1471-0528.1999.tb08322.x.
Hamoud S, Mancini J, Marchand F, Bretelle F, Boubli L, D’Ercole C, Carcopino X. Severe perineal morbidity of instrumental deliveries using Thierry's spatulas and vacuum extraction: a prospective observational cohort study. J Gynecol Obstet Hum Reprod. 2017;46(1):43–51. https://doi.org/10.1016/j.jgyn.2015.11.003.
Vanlieferinghen S, Girard G, Mandelbrot L. A comparison of maternal and fetal complications during operative vaginal delivery using Thierry's spatulas and the vacuum extractor. J Gynecol Obstet Biol Reprod (Paris). 2009;38(8):648–54. https://doi.org/10.1016/j.jgyn.2009.09.015.
Boucoiran I, Valerio L, Bafghi A, Delotte J, Bongain A. Spatula-assisted deliveries: a large cohort of 1065 cases. Eur J Obstet Gynecol Reprod Biol. 2010;151(1):46–51. https://doi.org/10.1016/j.ejogrb.2010.03.024.
Durand-Maison O, Mangin-Meyniel M, Tabard F, Bulot P, Cottenet J, Gobenceaux A-S. Thierry’s spatulas or forceps—a comparison between maternal-fetal morbidities. Gynecol Obstet Fertil. 2016;44(1):17–22. https://doi.org/10.1016/j.gyobfe.2015.09.013.
Parant O, Simon-Toulza C, Cristini C, Vayssiere C, Arnaud C, Reme JM. Faecal incontinence after first instrumental vaginal delivery using Thierry’s spatulas. Int Urogynecol J. 2010;21(10):1195–203. https://doi.org/10.1007/s00192-010-1176-3.
Arouca M, Duarte T, Lott D, Magnani P, Nogueira A, Silva J, Brito L. Validation and cultural translation for Brazilian Portuguese version of the Pelvic Floor Impact Questionnaire (PFIQ-7) and Pelvic Floor Distress Inventory (PFDI-20). Int Urogynecol J. 2016;27:1097–106. https://doi.org/10.1007/s00192-015-2938-8.
Barber M, Walters M, Bump R. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193:103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Reimers C, Siafarikas F, Jensen J, Småstuen M, Bø K, Engh M. Risk factors for anatomic pelvic organ prolapse at 6 weeks postpartum: a prospective observational study. Int Urogynecol J. 2019;30(3):477–82. https://doi.org/10.1007/s00192-018-3650-2.
Driusso P, Beleza ACS, Mira DM, de Oliveira Sato T, de Carvalho Cavalli R, Ferreira CHJ, de Fatima Carreira M. Are there differences in short-term pelvic floor muscle function after cesarean section or vaginal delivery in primiparous women? A systematic review with meta-analysis. Int Urogynecol J. 2020;31(8):1497–506. https://doi.org/10.1007/s00192-020-04231-6.
Sartore A, De Seta F, Maso G, Pregazzi R, Grimaldi E, Guaschino S. The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstet Gynecol. 2004;103(4):669–73. https://doi.org/10.1097/01.AOG.0000119223.04441.c9.
Ponkey SE, Cohen AP, Heffner LJ, Lieberman E. Persistent fetal occiput posterior position: obstetric outcomes. Obstet Gynecol. 2003;101(5):915–20. https://doi.org/10.1016/S0029-7844(03)00068-1.
Guerby P, Parant O, Chantalat E, Vayssiere C, Vidal F. Operative vaginal delivery in case of persistent occiput posterior position after manual rotation failure: a 6-month follow-up on pelvic floor function. Arch Gynecol Obstet. 2018;298(1):111–20. https://doi.org/10.1007/s00404-018-4794-5.
Pardo E, Rotem R, Erenberg M, Yahav L, Yohay Z, Yohay D, Weintraub AY. Recovery from pelvic floor dysfunction symptoms in the postpartum is associated with the duration of the second stage of labor. Arch Gynecol Obstet. 2019;300(1):127–33. https://doi.org/10.1007/s00404-019-05173-1.
Anim-Somuah M, Smyth RM, Jones L (2011) Epidural versus non-epidural or no analgesia in labour. Cochrane Database Syst Rev. (12):CD000331. https://doi.org/10.1002/14651858.CD000331.pub3.
Thomas V, Shek KL, Guzmán RR, Dietz HP. Temporal latency between pelvic floor trauma and presentation for prolapse surgery: a retrospective observational study. Int Urogynecol. 2015;26(8):1185–9. https://doi.org/10.1007/s00192-015-2677-x.
Acknowledgements
The authors wish to acknowledge the support of several clinicians and midwives from the Department of Obstetrics and Gynecology of the Hospital de Braga for their help with patient recruitment, and to all the participants for their contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclaimer/conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borges, A.C., Sousa, N., Sarabando, R. et al. Pelvic floor dysfunction after vaginal delivery: MOODS—a prospective study. Int Urogynecol J 33, 1539–1547 (2022). https://doi.org/10.1007/s00192-021-04982-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04982-w