Abstract
Introduction and hypothesis
While approximately 225,000 pelvic organ prolapse (POP) surgeries are performed annually in the US, there is no consensus on the optimal route for pelvic support for the initial treatment of uterovaginal prolapse (UVP). Our objective is to compare the outcomes of abdominal sacrocolpopexy (ASC) to vaginal pelvic support (VPS) with either uterosacral ligament suspension (USLS) or sacrospinous ligament fixation (SSF) in combination with hysterectomy for treating apical prolapse.
Methods
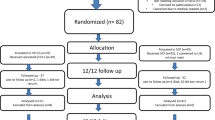
A systematic search was performed through March 2021. Studies comparing ASC with VPS for treatment of UVP were included in the review. The primary outcome was the rate of overall anatomic prolapse failure per studies' definition. Secondary outcomes included evaluating isolated recurrent vaginal wall prolapse, postoperative POP-Q points, total vaginal length (TVL), and Pelvic Floor Distress Inventory (PFDI-20) scores. Random effect analyses were generated utilizing R 4.0.2.
Results
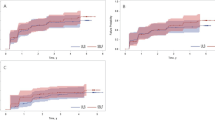
Out of 4225 total studies, 4 met our inclusion criteria, including 226 patients in the ASC group and 199 patients in the VPS group. ASC was not found to be associated with a higher rate of vaginal wall prolapse recurrence (OR = 0.6; 95% CI = 0.2–2.4; P = 0.33). There was no significant difference between groups for anterior or apical vaginal wall prolapse recurrence (P = 0.58 and P = 0.97, respectively). ASC was associated with significantly longer TVL (mean difference [MD]: 1.01; 95% CI = 0.33–1.70; P = 0.02) and better POP-Q Ba scores [MD = −0.23; 95% CI = −0.37; −0.10; P = 0.01].
Conclusions
ASC and vaginal pelvic support (either USLS or SSF) have comparable anatomical outcomes. However, weak evidence of a difference in TVL and Ba was found. The strength of the evidence in this study is based on the small number of observational studies. A large, randomized trial is highly warranted.






Similar content being viewed by others
Abbreviations
- POP:
-
Pelvic organ prolapse
- UVP:
-
Uterovaginal prolapse
- ASC:
-
Abdominal sacrocolpopexy
- SSF:
-
Sacrospinous ligament fixation
- USLS:
-
Uterosacral ligament suspension
- GRADE:
-
Grading of Recommendations, Assessment, Development, and Evaluation
- VPS:
-
Vaginal pelvic support
- TVL:
-
Total vaginal length
- PFDI-20:
-
Pelvic Floor Disability Index
- PFIQ-7:
-
Pelvic Floor Impact Questionnaire
- PISQ-12:
-
Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire
- ICIQ:
-
International Consultation on Incontinence Questionnaire
- HRQoL:
-
Health-related quality of life
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20. https://doi.org/10.1002/nau.20798.
Costantini E, Brubaker L, Cervigni M, Matthews CA, O’Reilly BA, Rizk D, et al. Sacrocolpopexy for pelvic organ prolapse: evidence-based review and recommendations. Eur J Obstet Gynecol Reprod Biol. 2016;205(October):60–5. https://doi.org/10.1016/j.ejogrb.2016.07.503.
Jones KA, Shepherd JP, Oliphant SS, Wang L, Bunker CH, Lowder JL. Trends in inpatient prolapse procedures in the United States, 1979–2006. Am J Obstet Gynecol. 2010;202(5):501.e1–7. https://doi.org/10.1016/j.ajog.2010.01.017.
Oliphant SS, Jones KA, Wang L, Bunker CH, Lowder JL. Trends over time with commonly performed obstetric and gynecologic inpatient procedures. Obstet Gynecol. 2010;116(4):926–31. https://doi.org/10.1097/AOG.0b013e3181f38599.
Wilkins MF, Jennifer MW. Lifetime risk of surgery for stress urinary incontinence or pelvic organ prolapse. Minerva Ginecol. 2017;69(2):171–7. https://doi.org/10.23736/S0026-4784.16.04011-9.
Blandon RE, Bharucha AE, Joseph Melton L 3rd, Schleck CD, Babalola EO, Zinsmeister AR, et al. Incidence of pelvic floor repair after hysterectomy: a population-based cohort study. Am J Obstet Gynecol. 2007;197(6):664.e1–7. https://doi.org/10.1016/j.ajog.2007.08.064.
Chung S-H, Kim WB. Various approaches and treatments for pelvic organ prolapse in women. J Menopausal Med. 2018;24(3):155–62. https://doi.org/10.6118/jmm.2018.24.3.155.
ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin no. 85: pelvic organ prolapse. Obstet Gynecol. 2007;110(3):717–29. https://doi.org/10.1097/01.AOG.0000263925.97887.72.
Fairchild PS, Kamdar NS, Berger MB, Morgan DM. Rates of colpopexy and colporrhaphy at the time of hysterectomy for prolapse. Am J Obstet Gynecol. 2016;214(2):262.e1–7. https://doi.org/10.1016/j.ajog.2015.08.053.
Ross WT, Meister MR, Shepherd JP, Olsen MA, Lowder JL. Utilization of apical vaginal support procedures at time of inpatient hysterectomy performed for benign conditions: a national estimate. Am J Obstet Gynecol. 2017;217(4):436.e1–8. https://doi.org/10.1016/j.ajog.2017.07.010.
Kong MK, Bai SW. Surgical treatments for vaginal apical prolapse. Obstet Gynecol Sci. 2016;59(4):253–60. https://doi.org/10.5468/ogs.2016.59.4.253.
Westermann LB, Crisp CC, Mazloomdoost D, Kleeman SD, Pauls RN. Comparative perioperative pain and recovery in women undergoing vaginal reconstruction versus robotic Sacrocolpopexy. Female Pelvic Med Reconstruct Surg. 2017;23(2):95–100. https://doi.org/10.1097/SPV.0000000000000368.
Petri E, Ashok K. Sacrospinous vaginal fixation—current status. Acta Obstet Gynecol Scand. 2011;90(5):429–36. https://doi.org/10.1111/j.1600-0412.2011.01084.x.
Margulies RU, Rogers MAM, Morgan DM. Outcomes of transvaginal uterosacral ligament suspension: systematic review and metaanalysis. Am J Obstet Gynecol. 2010;202(2):124–34. https://doi.org/10.1016/j.ajog.2009.07.052.
Rogers RG, Nolen TL, Weidner AC, Richter HE, Eric Jelovsek J, Shepherd JP, et al. Surgical outcomes after apical repair for vault compared with uterovaginal prolapse. Obstet Gynecol. 2018;131(3):475–83. https://doi.org/10.1097/AOG.0000000000002492.
Maher, Christopher, Benjamin Feiner, Kaven Baessler, and Corina Schmid. 2013. Surgical management of pelvic organ prolapse in women. Cochrane Database Systematic Rev 4(April):CD004014. https://doi.org/10.1002/14651858.CD004014.pub5.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
GRADEpro Guideline Development Tool [Software]. McMaster University, 2020 (developed by Evidence Prime, Inc.). http://www.gradeworkinggroup.org.
Chen Y, Hua K. Medium-term outcomes of laparoscopic sacrocolpopexy or sacrohysteropexy versus vaginal sacrospinous ligament fixation for middle compartment prolapse. Intl J Gynaecol Obstet: Off Organ Intl Federation Gynaecol Obstet. 2017;137(2):164–9. https://doi.org/10.1002/ijgo.12097.
La Cruz D, Jacquia F, Myers EM, Geller EJ. Vaginal versus robotic hysterectomy and concomitant pelvic support surgery: a comparison of postoperative vaginal length and sexual function. J Minim Invasive Gynecol. 2014;21(6):1010–4. https://doi.org/10.1016/j.jmig.2014.04.011.
Bastawros DA, Tarr ME, Templin MA, Stepp KJ, Bernard Taylor G, Myers EM. Anterior wall success at 1 year after vaginal uterosacral ligament suspension and sacral colpopexy. Female Pelvic Med Reconstruct Surg. 2020;26(10):612–6. https://doi.org/10.1097/SPV.0000000000000647.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
de Castro EB, Brito LGO, Juliato CRT. Vaginal hysterectomy with bilateral sacrospinous fixation plus an anterior mesh versus abdominal sacrocervicopexy for the treatment of primary apical prolapse in postmenopausal women: a randomized controlled study. Int Urogynecol J. 2020;31(2):365–72. https://doi.org/10.1007/s00192-019-03948-3.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(October):d5928. https://doi.org/10.1136/bmj.d5928.
Core Team R. R: A language and environment for statistical computing. Vienna: R Foundation for statistical computing; 2014. http://www.R-project.org/
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Benson JT, Lucente V, McClellan E. Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. Am J Obstet Gynecol. 1996;175(6):1418–21; discussion 1421–22. https://doi.org/10.1016/s0002-9378(96)70084-4.
Ng CCM, Han WHC. Comparison of effectiveness of vaginal and abdominal routes in treating severe uterovaginal or vault prolapse. Singap Med J. 2004;45(10):475–81 https://www.ncbi.nlm.nih.gov/pubmed/15455168.
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004;104(4):805–23. https://doi.org/10.1097/01.AOG.0000139514.90897.07.
Roovers, Jan-Paul W. R., C. Huub van der Vaart, Johanna G. van der Bom, Jules H. Schagen van Leeuwen, Piet C. Scholten, and A. Peter M. Heintz. 2004. “A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function.” BJOG: Intl J Obstet Gynaecol 111(1):50–56. https://doi.org/10.1111/j.1471-0528.2004.00001.x.
Cvach K, Dwyer P. Surgical management of pelvic organ prolapse: abdominal and vaginal approaches. World J Urol. 2012;30(4):471–7. https://doi.org/10.1007/s00345-011-0776-y.
Tsia-Shu Lo, Alex C. Wang. J Gynecol Surg. 1998;59–64. https://doi.org/10.1089/gyn.1998.14.59.
Maher CF, Qatawneh AM, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol. 2004;190(1):20–6. https://doi.org/10.1016/j.ajog.2003.08.031.
Slopnick EA, Petrikovets A, Sheyn D, Kim SP, Nguyen CT, Hijaz AK. Surgical trends and patient factors associated with the treatment of apical pelvic organ prolapse from a national sample. Int Urogynecol J. 2019;30(4):603–9. https://doi.org/10.1007/s00192-018-3769-1.
Lourenço M, de Thais R, Pergialiotis V, Durnea C, Elfituri A, Haddad JM, et al. A systematic review of reported outcomes and outcome measures in randomized controlled trials on apical prolapse surgery. Intl J Gynaecol Obstet: Off Organ Intl Federation Gynaecol Obstet. 2019;145(1):4–11. https://doi.org/10.1002/ijgo.12766.
Barber MD, Brubaker L, Nygaard I, Wheeler TL 2nd, Schaffer J, Chen Z, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9. https://doi.org/10.1097/AOG.0b013e3181b2b1ae.
Acknowledgements
The authors would like to thank Amber Catherine Stout for her help with the search.
Author information
Authors and Affiliations
Contributions
A Alfahmy: Data collection, Manuscript writing/editing.
A Mahran: Idea conceptualization, Data collection, Manuscript writing/editing, Data analysis and management
B Conroy: Manuscript writing/editing.
RR Brewka: Manuscript editing and development
M Ibrahim: Data collection and search strategy
D Sheyn: Manuscript editing and development
S El-Nashar: Idea conceptualization, Manuscript editing and development
AK Hijaz: Idea conceptualization, Protocol development, Manuscript editing and development
Corresponding author
Ethics declarations
Conflicts of interest
Adonis K Hijaz is a member of the Astellas, Inc. Speaker’s Bureau. David D Sheyn receives grant funding from Renalis. Anood Alfahmy, Amr Mahran, Britt Conroy, Rosemary R. Brewka, Mostafa Ibrahim, and Sherif A. El-Nashar declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alfahmy, A., Mahran, A., Conroy, B. et al. Abdominal and vaginal pelvic support with concomitant hysterectomy for uterovaginal pelvic prolapse: a comparative systematic review and meta-analysis. Int Urogynecol J 32, 2021–2031 (2021). https://doi.org/10.1007/s00192-021-04861-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04861-4