Abstract
Introduction and hypothesis
Pregnancy and delivery are known risk factors for stress and mixed urinary incontinence. The most common surgical treatment is mid-urethral sling (MUS) surgery. This study evaluated the potential impact of the obstetrical history on the short-term subjective and objective failure rates after MUS surgery.
Methods
A registry-based surgical cohort study using data from the Medical Birth Registry of Norway (MBRN) and the national Norwegian Female Incontinence Registry (NFIR). Data from 14,787 women that underwent MUS surgery from 1998 to 2016 with complete registrations in the MBRN were included. Outcomes were 6–12-month postoperative subjective and objective failure rates. The potential impact of obstetrical and constitutional factors on both outcomes was tested in a multivariate logistic regression model.
Results
Several obstetrical variables seemed to impact both outcomes in the univariate analyses. However, in the multivariate analyses, none of the obstetrical variables significantly impacted subjective failure, and only being nulliparous before MUS surgery remained a risk factor for objective failure [aOR 1.60, (95% CI 1.07–2.40), p = 0.022]. High body mass index at time of surgery, non-retropubic slings, high preoperative urgency symptom load, and surgical complications were all strong risk factors for poor outcomes in the multivariate analyses.
Conclusion
Although childbirth is considered a risk factor for developing stress urinary incontinence, childbirth does not appear to affect the result of MUS in parous women. Our results suggest that nulliparous women with SUI may have a different pathophysiology than SUI after childbirth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Female urinary incontinence (UI) is the most prevalent long-term pelvic floor disorder with a substantial negative impact on women’s quality of life, productivity, socializing, and sexuality [1, 2]. Stress urinary incontinence (SUI), defined as involuntary loss of urine on physical exertion, sneezing, or coughing [3], affects approximately 15% of the female population, with the highest prevalence found in women between 25 and 49 years of age [1].
Although the etiology of SUI is multifactorial, childbirth is uniformly considered a significant risk factor [4,5,6,7]. The underlying pathophysiology has not been entirely determined, but it has been proposed that pelvic floor injuries may weaken the supportive structures around the bladder neck and urethra through mechanical forces such as compression, stretching, or tearing of nerves, muscles, and/or connective tissue, causing SUI [8]. However, there is an ongoing debate regarding the possible long-term effects of pregnancy itself on later pelvic floor dysfunction and the additive effects of vaginal delivery in combination with other risk factors, such as birth weight, operative vaginal delivery and maternal age. There is also some evidence of a protective effect on pelvic floor function from cesarean delivery in the short term compared to vaginal delivery, but long-term protection has been questioned [4, 5, 9].
Surgical treatment is usually recommended when conservative treatment options fail [10]. Over the last decades, mid-urethral slings (MUS) have been established as the standard surgical treatment for SUI and stress-dominant mixed urinary incontinence (MUI) mainly due to their high efficacy, long-term durability, and lower rates of repeat surgery compared to other incontinence procedures [11]. Despite the high cure rates, there is still a group of women for whom the surgery fails in obtaining continence. Some of the risk factors identified are age at time of surgery, obesity, concomitant pelvic organ prolapse surgery, and surgical technique [12,13,14,15,16].
Even though childbirth is considered a significant risk factor for SUI development, we have to date little knowledge on whether the same obstetrical factors that caused injuries to the pelvic floor leading to SUI could potentially also determine the success of later SUI surgery. Norway has maintained national medical registries for many years. A national compulsory birth registry has been in place since 1967 and a national quality registry for female urinary incontinence surgery since 1998. Combining these two registries, we aimed to investigate the potential impact of various obstetrical factors on short-term subjective and objective failure rates after MUS surgery.
Materials and methods
This was a registry-based surgical cohort study of women recorded in the national Norwegian Female Incontinence Registry (NFIR) as having undergone MUS surgery for either stress or stress-dominant mixed urinary incontinence in Norway from 1998 to 2016. As the main aim of the study was to evaluate the impact from previous obstetrical history on surgical outcomes of later MUS operations, data on these women from the NFIR were then merged with data from the Medical Birth Registry of Norway (MBR) from its inception to 2016.
The Medical Birth Registry of Norway (MBRN) was established in 1967 as a mandatory population-based registry for all deliveries in Norway with nearly complete coverage. It receives notification of all deliveries in Norway with information on maternal health as well as prenatal, obstetrical, and neonatal outcomes.
The NFIR was established in 1998 and is a national quality registry for women undergoing urinary incontinence surgeries in Norway [17]. Participating is not mandatory, but > 95% of all female incontinence operations in Norway are performed in public hospitals that regularly report to the registry. The registry is used to improve the quality of incontinence surgeries at reporting hospitals by comparing results and complication rates to a national average in addition to collecting data for research. In recent years the registry has achieved almost complete coverage of women undergoing incontinence surgery and shown high reliability of reported and stored data [18]. Hospitals performing female incontinence surgery report their preoperative and 6–12-month postoperative subjective and objective data to NFIR. Subjective data are collected using a validated short-form urinary incontinence disease-specific questionnaire that calculates indices for the load of stress and urgency symptom bother [19]. The stress and urgency urinary incontinence indices are calculated from two domains of clustered questions and range from 0 to 12 (stress) and 0 to 8 (urgency), respectively. A high index score indicates a high symptom load with 0 indicating no symptoms. In addition, objective clinical data are reported by the surgeon at the time of the operation including results from preoperative objective testing, urodynamic findings, type of incontinence procedure, and any surgical complications occurring at or following surgery. Lastly, subjective and objective data from a mandatory follow-up 6–12 months after surgery are reported using the same validated questionnaire for subjective data as well as reporting results from objective testing, uroflowmetry, and post-void residual urine measurements. At the time of data extraction, 29 of the 39 hospital departments performing female incontinence surgery in Norway reported to the registry, which included approximately 70% of the incontinence surgeries performed in Norway during this time period (data given to authors from the NFIR).
The two outcomes for this study were short-term (6–12-month) subjective and objective SUI failure rates after primary MUS surgery. Patients with concomitant pelvic organ prolapse (POP) surgery or lacking information on whether the surgery was a primary or recurrent SUI operation were excluded. Subjective failure was defined as a stress urinary incontinence index score > 0 at the postoperative 6–12-month follow-up. Objective failure was defined as an increase in pad weight ≥ 1 g during a standardized cough-jump pad-weighing stress test consisting of 20 jumping jacks on the spot and three forceful coughs in the standing position with 300 ml bladder volume [20]. Women who were registered in the NFIR as having undergone a later operation for recurrent SUI after previous MUS before the 6–12-month follow-up were defined as both subjective and objective failures in the statistical analyses.
From the NFIR, the following data were extracted: date of surgery, type of mid-urethral sling (retropubic, inside-out obturator, outside-in obturator, or mini-sling), body mass index (BMI) at time of surgery, preoperative post-void residual urine, preoperative maximum urinary flow rate, maximum urethra closure pressure, pre- and 6–12-month postoperative results from the cough-jump pad-weighing stress tests, pre- and 6–12-month postoperative stress, and urgency urinary incontinence indices and complications (yes/no) during or immediately after surgery (complete list of complications provided in supplemental Appendix 1).
From the MBRN, the following data were extracted: parity, mode of delivery, offspring birth weight, head circumference, presentation, episiotomy, grade 3 and 4 perineal tears, and mothers’ age at delivery. In addition, time from last delivery until MUS surgery was calculated. To ensure complete data from the birth registry and accurately determine which women were nulliparous at the time of surgery, we chose to exclude women born before 1949 as these could theoretically have given birth to non-registered children before the inception of the MBRN.
Potential obstetrical and constitutional risk factors were tested against both subjective and objective failure as previously defined, using a multivariate logistic regression model. The risk factors evaluated in the model were parity (0, 1, 2, or ≥ 3), mode of delivery, presentation, episiotomy (yes/no), offspring birth weight (< or ≥ 4000 g), head circumference (< or ≥ 36 cm), perineal tear grade 3 or 4 (yes/no), age at first delivery (< or ≥ 25 years), age at surgery (in decades), BMI at surgery (normal weight: 18.5–24.9, overweight: 25.0–29.9, and obese: ≥ 30.0 as defined by the World Health Organization), time from last delivery until surgery (in decades), preoperative stress and urgency urinary incontinence index scores (in quartiles), preoperative cough-jump pad-weighing stress test results (in quartiles), preoperative post-void residual urine (< or ≥ 100 ml), preoperative maximum urinary flow rate (< or ≥ 15 ml/s), type of mid-urethral sling (4 groups), and surgical complications (yes/no). Fetal macrosomia, defined as ≥ 4000 g, was used as a dichotomization of birth weight. Head circumference and age at first delivery were dichotomized around the median. Mode of delivery was stratified in three groups (spontaneous vaginal only, instrumental vaginal, cesarean only). Women who had at least one instrumental vaginal delivery were stratified to the instrumental vaginal delivery group regardless of whether they had also had cesarean or spontaneous vaginal deliveries. Women stratified to the cesarean group had only had cesarean deliveries.
Methods, definitions, and units in the study conform to the standards recommended by the International Urogynecological Association and International Continence Society joint report on the terminology for female pelvic floor dysfunction [3].
The study was approved by the Regional Committee for Medical and Health Research Ethics in Norway (#2015/434) and the Institutional Personal Data Officer at Oslo University Hospital. Exemption from the requirement for patient consent was given because there was no foreseen risk of violation of personal data in the study combined with the need for completeness of data for study validity. Full anonymity of participating women was maintained in the final study file used for data analysis. The study was registered at ClinicalTrials.gov (NCT02999347).
Statistical analyses were performed using STATA: Software for Statistics and Data Science version 16.0 (StataCorp). Continuous variables are presented as medians with interquartile range (IQR), and dichotomous variables are presented as frequencies (percentages). Mann-Whitney U-test was used to compare continuous variables and Fisher's exact test for dichotomous variables. Potential risk factors for objective or subjective short-term failure after MUS are presented as crude and adjusted odds ratios (OR) with 95% confidence intervals (CI) and p-values in the logistic regression model. A significance level of 5% was used. Covariates with a significance level of 0.20 in the univariate crude analysis were included in the multivariate regression model. A backward variable selection was then used by stepwise removal of variables with significance levels > 0.05. No significant interactions were found between the independent variables. The final model was tested using a goodness-of-fit test (Hosmer-Lemeshow).
Results
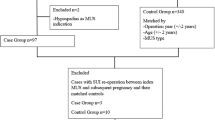
After merging data from the Norwegian Incontinence Registry and the Medical Birth Registry of Norway, 18,027 women from 29 reporting departments who had undergone a mid-urethral sling (MUS) procedure were found eligible for inclusion (Fig. 1). Women with duplicate records, those who had undergone non-MUS surgery for their stress urinary incontinence (SUI) or those who lacked information regarding this being their primary operation or an operation for recurrent SUI were excluded. The remaining 14,787 women were included in the study analyses, of which 14,171 (96%) had undergone at least one childbirth and 616 (4%) were nulliparous before their primary MUS procedure (Fig. 1).
Baseline clinical characteristics and short-term (6–12-month) subjective and objective failure rates for both parous and nulliparous women are presented in Table 1. The median age was 47 years (IQR: 42–52) and median BMI 25.4 kg/m² (IQR: 23.0–29.0) for the total study group. For parous women, the median time from last delivery until MUS operation was 14 years (IQR: 0–46). Additional obstetrical descriptive factors such as parity, age at first delivery, presentation, maximum birth weight, episiotomy, perineal tear grade 3/4, and mode of delivery are presented in Table 1.
Retropubic MUS was the most common sling type utilized (78.4%). For the total population, the subjective and objective 6–12-month failure rate was 28.9% and 7.7%, respectively (Table 1).
In the non-parametric analysis, nulliparous women had a significantly higher subjective and objective short-term failure rate compared with parous woman (subjective failure in 33.8% vs. 28.7%, p = 0.010 and objective failure in: 10.3% vs. 7.6%, p = 0.036) (Table 1). However, at baseline, the nulliparous women were significantly older (p < 0.001), had a higher BMI (p < 0.001), and had a higher preoperative symptom load for both stress and urgency urinary incontinence reflected by their higher preoperative stress and urgency urinary incontinence symptom scores (p < 0.001) (Table 1).
In the univariate analysis, being nulliparous also seemed to impact both subjective and objective failure rates [OR 1.27 (95% CI 1.05–1.53), p = 0.012, and 1.41 (95% CI 1.02–1.95), p = 0.037] (Tables 2 and 3). Additional obstetrical factors seemingly impacting failure rates in the univariate analyses were head circumference (subjective failure), age at first delivery (objective failure), and time from last delivery until surgery (objective failure) (Tables 2 and 3). In the multivariate analyses, however, the only obstetrical factor significantly impacting the short-term objective failure rate was being nulliparous before MUS surgery, with an increased risk of 60% [aOR 1.60 (95% CI 1.07–2.40), p = 0.022] when compared with parous women having a median of two deliveries (Table 3). For subjective failure, none of the obstetrical factors investigated exerted any significant impact (Table 2). Constitutional factors that were significantly associated with the subjective and/or objective failure rate in the adjusted regression analyses included BMI at time of surgery, preoperative cough-jump stress test results, preoperative stress and urgency symptom loads expressed as preoperative stress and urgency urinary incontinence index scores, preoperative low maximum urinary flow rate, type of sling utilized, and surgical complications (Tables 2 and 3).
Discussion
This nationwide prospective cohort study based on high-quality registry data investigated the potential impact of women’s obstetrical history expressed as various obstetrical factors on short-term subjective and objective failure rates after MUS surgery. The results initially indicated that several obstetrical variables might exert an impact on both outcomes as shown in the univariate analyses. However, in the final multivariate model when adjusting for known constitutional factors, none of the obstetrical variables remained independent risk factors for subjective failure. Only nulliparity before MUS surgery remained an independent risk factor for objective failure. Risk factors such as high BMI at time of surgery, a high preoperative degree of objective leakage, a high preoperative symptom load for both stress and urgency symptoms, preoperative maximum urinary flow rate < 15 ml/s, type of sling utilized and surgical complications, however, remained strong risk factors for both subjective and objective outcomes in the multivariate model. These constitutional risk factors for SUI have previously been well documented in the literature [11, 16, 21, 22].
Childbearing is identified as an important independent risk factor for SUI. In a large cross-sectional study including 27,900 women in Norway, SUI prevalence was associated with increasing parity, with a relative risk of 1.9 (95% CI, 1.6–2.2) for primiparous women and 2.3 (95% CI, 2.0–2.6) for women with two deliveries [6]. The association between childbearing and urinary incontinence is, however, not fully understood. Data suggest that pregnancy and delivery induce pelvic floor injury through mechanical forces [8], causing increased bladder neck hypermobility and decreased pelvic floor contractility [23, 24]. Parous women have an attributable risk of 50% for SUI development related to pregnancy and childbirth [9]. Furthermore, several studies have shown that vaginal delivery is a significant risk factor for the development of SUI [4, 5, 9, 25].
However, to date it is unknown whether these obstetrical factors such as delivery mode, obstetric anal sphincter injury, levator ani avulsion, and fetal factors also impact surgical outcomes in women with SUI. Parity is, to our knowledge, the only obstetrical factor previously studied [13, 15]. Laterza et al. evaluated the effect of parity at the time of surgery on short- and long-term outcomes in women who underwent SUI surgery by MUS [15]. This study utilized data from a previously published randomized controlled trial that included 554 patients in which subjective and objective outcomes of TVT and TVT-O were compared. They found no significant association between parity and the risk of either subjective or objective SUI recurrence. Furthermore, in a prospective cohort study by Majkusiak and co-workers including 238 women who had a retropubic MUS operation, the number of vaginal deliveries showed no impact on short-term sling failure [13]. Thus, the findings of both of these studies are consistent with the results in the present study. However, as we had the possibility of also including a sufficiently large group of women who had not given birth before their MUS operation, we were able to demonstrate that being nulliparous before MUS surgery seems to be an independent risk factor for objective failure compared with parous women, even after adjusting for obstetrical and known constitutional risk factors. We know from published literature that even though childbirth is a risk factor for stress urinary incontinence, studies have also demonstrated that stress urinary incontinence occurs in approximately 5%–11% of nulliparous women 25–64 years old [6, 26]. It is reasonable, therefore, to hypothesize that nulliparous women with SUI might have a different or additional underlying pathophysiological mechanism for their incontinence rather than a simple urethral hypermobility caused by trauma to the pelvic floor. In the present study, the nulliparous women had a higher BMI, which by itself is a known risk factor for SUI [16]. There is also evidence that hereditary factors could play a part, such as a different connective tissue composition in nulliparous women with increased risk of developing SUI. This was demonstrated in a study from Keane et al. which found significantly less periurethral collagen in nulliparous women with pure SUI compared to continent nulliparous controls, indicating a genetically higher susceptibility to SUI development [27]. Other potential explanations for SUI developing in nulliparous women with no known trauma to the pelvic floor could include a poor sphincter function of unknown cause, a dysfunctional pelvic floor due to age-related atrophy of muscles, and/or undiagnosed neurological diseases. It has been demonstrated that women with sphincter insufficiency have lower cure rates after MUS compared to women with urethral hypermobility [12].
Constitutional factors were confirmed in this study as strong risk factors for both subjective and objective short-term failure. In population-based studies high BMI has proved to be one of the main risk factors for both the development of stress urinary incontinence [28] and poor outcomes after MUS [16]. Retropubic MUS are considered to be more effective than trans-obturator and mini-slings [11]. This was also confirmed in our study demonstrating a significantly lower failure rate when retropubic MUS was utilized. A high preoperative urgency symptom load almost doubled the odds of subjective and objective failure after MUS surgery in our study, which is in agreement with previous published studies [21, 22]. Several studies have also found advancing age to be a risk factor for MUS failure [14, 21, 29]. In our study, age at surgery was not a risk factor for subjective or objective failure. However, we believe the reason for this are that women > 67 years (born before 1949) were excluded from our study as these could theoretically have given birth to non-registered children before the inception of the MBRN. In a study by Engen et al., also based on data from approximately the same cohort of women, it was demonstrated that a significant increase in MUS failure only occurred for women in the 7th decade and older [29].
This study’s main strength was the use of data from a large population-based cohort. The cohort was identified through a surgical incontinence registry with proven high coverage and data reliability [18]. All inhabitants in Norway are provided with a public healthcare system where surgical treatment for urinary incontinence is free of charge. This ensured a low degree of selection bias and a high degree of statistical precision in the analysis. Consequently, we believe the present study has a high level of external validity. Furthermore, we were also able to explore the women’s obstetrical history in detail because of the merging with data from the Medical Birth Registry of Norway (MBRN), which has been proven suitable for population-based studies [30].
There are also several important limitations to this study, the most important being that we were only able to study the potential impact of obstetrical factors on short-term results, as the NFIR only has high coverage for the first postoperative 6–12 months of follow-up. Later follow-ups are optional for the reporting hospitals and were therefore deemed to have a too high risk of selection bias to be used in the present study. We realize that a potential impact from obstetrical factors on long-term results therefore cannot be ruled out with certainty based on our study. Other important limitations to this study were the inability to adjust for factors related to the surgeon’s experience (surgical volume), local differences in incontinence assessment, and local preferences regarding the type of sling. Furthermore, all use of registry data carries the risk of missing data and inaccuracy in the individual entries, potentially impacting the results, and should always be interpreted with that in mind.
Knowledge about factors associated with treatment failure is essential when counseling patients regarding MUS surgery’s efficacy and to facilitate appropriate expectations of women with SUI women prior to their decision on surgery. Although pregnancy and childbirth are considered significant risk factors for developing stress urinary incontinence, these obstetrical factors do not seem to majorly impact the short-term surgical results. However, the negative impact on objective failure rates of being nulliparous before MUS surgery calls for further research to fully understand the mechanism behind the development of SUI in this sub-group of women.
References
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. J Clin Epidemiol. 2000;53:1150–7. https://doi.org/10.1016/s0895-4356(00)00232-8.
Hunskaar S, Lose G, Sykes D, Voss S. The prevalence of urinary incontinence in women in four European countries. BJU Int. 2004;93:324–30. https://doi.org/10.1111/j.1464-410x.2003.04609.x.
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
Gyhagen M, Åkervall S, Molin M, Milsom I. The effect of childbirth on urinary incontinence: a matched cohort study in women aged 40-64 years. Am J Obstet Gynecol. 2019;221:322.e1–322.e17. https://doi.org/10.1016/j.ajog.2019.05.022.
Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900–7. https://doi.org/10.1056/nejmoa021788.
Rortveit G, Hannestad YS, Daltveit AK, Hunskaar S. Age- and type-dependent effects of parity on urinary incontinence: the Norwegian EPINCONT study. Obstet Gynecol. 2001;98:1004–10. https://doi.org/10.1016/s0029-7844(01)01566-6.
Goldberg RP, Abramov Y, Botros S, et al. Delivery mode is a major environmental determinant of stress urinary incontinence: results of the Evanston-Northwestern Twin Sisters Study. Am J Obstet Gynecol. 2005;193:2149–53. https://doi.org/10.1016/j.ajog.2005.08.055.
Alperin M, Cook M, Tuttle LJ, et al. Impact of vaginal parity and aging on the architectural design of pelvic floor muscles. Am J Obstet Gynecol. 2016;215:312.e1–9. https://doi.org/10.1016/j.ajog.2016.02.033.
Patel DA, Xu X, Thomason AD, et al. Childbirth and pelvic floor dysfunction: an epidemiologic approach to the assessment of prevention opportunities at delivery. Am J Obstet Gynecol. 2006;195:23–8. https://doi.org/10.1016/j.ajog.2006.01.042.
(n.d.) NICE - Nationale Institute for Health and Care Excellence: Urinary incontinence and pelvic organ prolapse in women: management - 2019. https://www.nice.org.uk/guidance/ng123/chapter/Recommendations#surgical-management-of-stress-urinary-incontinence. Accessed 20 Dec 2020.
Ford AA, Rogerson L, Cody JD, et al. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017;5:CD006375. https://doi.org/10.1002/14651858.cd006375.pub4.
Houwert RM, Venema PL, Aquarius AE, et al. Risk factors for failure of retropubic and transobturator midurethral slings. Am J Obstet Gynecol. 2009;201:202.e1–8. https://doi.org/10.1016/j.ajog.2009.04.009.
Majkusiak W, Pomian A, Horosz E, et al. Demographic risk factors for mid-urethral sling failure. Do they really matter? PLoS ONE. 2018;13(11):e0207185. https://doi.org/10.1371/journal.pone.0207185.
Toozs-Hobson P, Devani P, Pick J, et al. Does age affect the outcome of suburethral tape surgery? The importance of national registries in answering bigger questions. Int Urogynecol J. 2016;27:1541–5. https://doi.org/10.1007/s00192-016-2995-7.
Laterza RM, Halpern K, Ulrich D, et al. Influence of age, BMI and parity on the success rate of midurethral slings for stress urinary incontinence. PLoS One. 2018;13:e0201167. https://doi.org/10.1371/journal.pone.0201167.
Bach F, Hill S, Toozs-Hobson P. The effect of body mass index on retropubic midurethral slings. Am J Obstet Gynecol. 2019;220:371.e1–9. https://doi.org/10.1016/j.ajog.2018.12.018.
Kulseng-Hanssen S. The development of a national database of the results of surgery for urinary incontinence in women. BJOG Int J Obstet Gynaecol. 2003;110:975–82.
Dyrkorn OA, Staff AC, Kulseng-Hanssen S, et al. The completeness and accuracy of the Norwegian Female Incontinence Registry. Acta Obstet Gynecol Scand. 2020;99:1618–25. https://doi.org/10.1111/aogs.13951.
Kulseng-Hanssen S, Borstad E. The development of a questionnaire to measure the severity of symptoms and the quality of life before and after surgery for stress incontinence. BJOG Int J Obstet Gynaecol. 2003;110:983–8.
Berild GH, Kulseng-Hanssen S. Reproducibility of a cough and jump stress test for the evaluation of urinary incontinence. Int Urogynecol J. 2012;23:1449–53. https://doi.org/10.1007/s00192-012-1733-z.
Svenningsen R, Staff AC, Schiøtz HA, et al. Risk factors for long-term failure of the retropubic tension-free vaginal tape procedure. Neurourol Urodyn. 2014;33:1140–6. https://doi.org/10.1002/nau.22466.
Gleason JL, Parden AM, Jauk V, et al. Outcomes of midurethral sling procedures in women with mixed urinary incontinence. Int Urogynecol J. 2015;26:715–20. https://doi.org/10.1007/s00192-014-2580-x.
McGuire EJ. Pathophysiology of stress urinary incontinence. Rev Urol. 2004;6(Suppl 5):S11–7.
Stær-Jensen J, Siafarikas F, Hilde G, et al. Postpartum recovery of Levator Hiatus and bladder neck mobility in relation to pregnancy. Obstet Gynecol. 2015;125:531–9. https://doi.org/10.1097/aog.0000000000000645.
Tähtinen RM, Cartwright R, Tsui JF, et al. Long-term impact of mode of delivery on stress urinary incontinence and urgency urinary incontinence: a systematic review and meta-analysis. Eur Urol. 2016;70:148–58. https://doi.org/10.1016/j.eururo.2016.01.037.
Othman JA-M, Åkervall S, Milsom I, Gyhagen M. Urinary incontinence in nulliparous women aged 25–64 years: a national survey. Am J Obstet Gynecol. 2017;216:149.e1–149.e11. https://doi.org/10.1016/j.ajog.2016.09.104.
Keane DP, Sims TJ, Abrams P, Bailey AJ. Analysis of collagen status in premenopausal nulliparous women with genuine stress incontinence. BJOG Int J Obstet Gynaecol. 1997;104:994–8. https://doi.org/10.1111/j.1471-0528.1997.tb12055.x.
Fuselier A, Hanberry J, Lovin JM, Gomelsky A. Obesity and stress urinary incontinence: impact on pathophysiology and treatment. Curr Urol Rep. 2018;19:10. https://doi.org/10.1007/s11934-018-0762-7.
Engen M, Svenningsen R, Schiøtz HA, Kulseng-Hanssen S. Mid-urethral slings in young, middle-aged, and older women. Neurourol Urodyn. 2018;37:2578–85. https://doi.org/10.1002/nau.23583.
Baghestan E, Børdahl PE, Rasmussen SA, et al. A validation of the diagnosis of obstetric sphincter tears in two Norwegian databases, the Medical Birth Registry and the Patient Administration System. Acta Obstet Gynecol Scand. 2007;86:205–9. https://doi.org/10.1080/00016340601111364.
Acknowledgments
Valuable help in extracting data from the Norwegian Female Incontinence Registry (NFIR) was given by Tomislav Dimoski, system developer at the Norwegian National Female Incontinence Registry. The authors also acknowledge the help in statistical analysis given by statistician Jon Michael Gran.
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital). The study was funded by Oslo University Hospital and supported by a grant from the Norwegian Medical Association (no. 14/1695). The funding sources had no role in the study design, data analysis, or writing of the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Sigurd Kulseng-Hanssen and Rune Svenningsen hold part-time positions at the Norwegian Female Incontinence Registry. Rune Svenningsen has also received speaker fees from Astellas and Gedeon Richter. The authors declare no other conflicts of interest.
Conference presentations
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 1135 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dyrkorn, O.A., Staff, A.C., Kulseng-Hanssen, S. et al. Previous obstetrical history does not impact short-term mid-urethral sling outcomes. Int Urogynecol J 32, 1733–1743 (2021). https://doi.org/10.1007/s00192-021-04836-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04836-5