Abstract
Introduction and hypothesis
The aim of this retrospective cohort study was to determine if recovery expectancies were associated with actual postdischarge recovery after laparoscopic sacrocolpopexy.
Methods
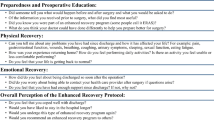
Study subjects (N = 167) undergoing laparoscopic sacrocolpopexy were asked to preoperatively predict the likelihood of a prolonged postdischarge recovery (> 42 days). Low, medium, and high recovery expectancy groups were created from responses to the likelihood of prolonged postdischarge recovery question. Previously established predictors of actual recovery 42 days after laparoscopic sacrocolpopexy included age, body mass index, Charlson co-morbidity index, short form (SF)-36 bodily pain scores, doctors’ and others’ health locus of control, and sick role investment. One parsimonious hierarchical linear and logistic regression model was constructed to determine if preoperative recovery expectancies were independently associated with PSR13 scores and “significant” postdischarge recovery after controlling for previously established predictors.
Results
Study subjects with high recovery expectancies had higher PSR13 scores than subjects with low recovery expectancies (82.32 ± 15.34 vs 73.30 ± 15.30, mean difference 9.01, 95%CI 1.08–16.94). Study subjects with low recovery expectancies scored 7.7 points lower on the PSR13 scale (minimally important difference = 5), which translated into a 73% reduction in the likelihood of being “significantly” recovered 42 days after surgery, after controlling for previously established predictors.
Conclusions
A low recovery expectancy has a negative impact on actual recovery 42 days after laparoscopic sacrocolpopexy. Our findings are important because preoperative recovery expectancies are modifiable predictors, making them a candidate for an expectancy manipulation intervention designed to optimize recovery after pelvic reconstructive surgery.

Similar content being viewed by others
References
Weiser TG, Haynes AB, Molina G, Lipsitz SR, Esquivel MM, Uribe-Leitz T, et al. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ. 2016;94(3):201–209F.
Hyder Z, Dewer P. Patients and professionals attitude towards postoperative recovery: academic competency assessment versus patient real time experience. BJMP. 2010;3(4):a339–44.
Flood AB, Lorence DP, Ding J, McPherson K, Black NA. The role of expectations in patients’ reports of post-operative outcomes and improvement following therapy. Med Care. 1993;31(11):1043–56.
Auer CJ, Glombiewski JA, Doering BK, Winkler A, Laferton JA, Broadbent E, et al. Patients’ expectations predict surgery outcomes: a meta-analysis. Int J Behav Med. 2016;23(1):49–62.
McCarthy SC, Lyons AC, Weinman J, Talbot R, Purnell D. Do expectations influence recovery from oral surgery? An illness representation approach. Psych and Health. 2003;18(1):109–26.
Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you’ll do? A systematic review of the evidence for a relation between patients’ recovery expectations and health outcomes. CMAJ. 2001;165(2):174–9.
Heit M, Carpenter JS, Chen CX, Stewart R, Hamner J, Rand KL. Predictors of postdischarge surgical recovery following laparoscopic sacrocolpopexy: a prospective cohort study. Female Pelvic Med Reconstr Surg. 2020;26(5):320–6.
Heit M, Guirguis N, Kassis N, Takase-Sanchez M, Carpenter J. Operationalizing the measurement of socioeconomic position in our urogynecology study populations: an illustrative review. Female Pelvic Med Reconstr Surg. 2017;23(3):208–15.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Wallston KA, Strudler Wallston B, DeVellis R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Monogr. 1978;6(1):160–70.
Berk M, Berk L, Dodd S, Jacka FN, Fitzgerald PB, de Castella AR, et al. Psychometric properties of a scale to measure investment in the sick role: the illness cognitions scale. J Eval Clin Pract. 2012;18:360–4.
Carpenter JS, Heit M, Chen CX, Stewart R, Hamner J, Rand KL. Validating the postdischarge surgical recovery scale 13 as a measure of perceived postoperative recovery after laparoscopic sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2017;23(2):86–9.
Pan C, Heit M. Preoperatively predicted prolonged recovery expectancies negatively impact actual postdischarge recovery 6 weeks after surgery. Female Pelvic Med Reconstr Surg. 2019;25(5):S46
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Vonk Noordegraaf A, Anema JR, Louwerse MD, Heymans MW, van Mechelen W, Brolmann HA, et al. Prediction of time to return to work after gynaecological surgery: a prospective cohort study in the Netherlands. BJOG. 2014;121(4):487–97.
Vonk Noordegraaf A, Huirne JA, Brölmann HA, Emanuel MH, van Kesteren PJ, Kleiverda G, et al. Effectiveness of a multidisciplinary care program on recovery and return to work of patients after gynaecological surgery: design of a randomized controlled trial. BMC Health Serv Res. 2012;12:29.
Arunachalam D, Heit MH. Impact of postoperative instructions on physical activity following pelvic reconstructive surgery: a randomized controlled trial. Int Urogynecol J. 2020;31:1337–45.
Mueller MG, Lewicky-Gaupp C, Collins SA, Abernethy MG, Alverdy A, Kenton K. Activity restriction recommendations and outcomes after reconstructive pelvic surgery: a randomized controlled trial. Obstet Gynecol. 2017;129(4):608–14.
Kalogera E, Nelson G, Liu J, Hu QL, Ko CY, Wick E, et al. Surgical technical evidence review for gynecologic surgery conducted for the Agency for Healthcare Research and Quality safety program for improving surgical care and recovery. Am J Obstet Gynecol. 2018;219(6):563.e1–563.e19.
Elphinston RA, Thibault P, Carriere JS, Rainville P, Sullivan MJL. Cross-sectional and prospective correlates of recovery expectancies in the rehabilitation of whiplash injury. Clin J Pain. 2018;34(4):306–12.
Clayton M, Verow P. A retrospective study of return to work following surgery. Occup Med. 2007;57(7):525–31.
Advincula AP. Vaginal hysterectomy: historical footnote or viable route? Obstet Gynecol. 2020;135(4):759–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Financial support
Dr. Chen is supported by the Grant Numbers KL2 TR002530 and UL1 TR002529 (A. Shekhar, PI) from the National Institutes of Health, National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, which had no direct role in this or the original study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Heit, M., Chen, C.X., Pan, C. et al. Recovery expectancies impact postdischarge recovery 42 days after laparoscopic sacrocolpopexy. Int Urogynecol J 32, 1527–1532 (2021). https://doi.org/10.1007/s00192-020-04586-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04586-w