Abstract
Introduction and hypothesis
We hypothesize that there will be improvement in a novice learners’ confidence and skill level with sacrospinous ligament fixation (SSLF) following a pelvic model-based simulation.
Methods
We performed a single-blinded randomized controlled trial with obstetrics and gynecology residents who were novices at SSLF. The residents were randomly assigned to two groups. The control group received a lecture on the SSLF procedure and anatomy, whereas the intervention group received the same lecture in addition to a pelvic model-based simulation session taught by urogynecologists. The residents’ knowledge of SSLF anatomy and confidence level with the procedure were measured via assessments administered before and after the educational interventions. Their technical skills were objectively assessed by one of two fellowship-trained urogynecologists who were blinded to their group allocation.
Results
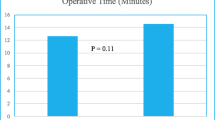
A total of 28 residents were recruited with 14 residents in each group and equal distribution of junior and senior trainees. None of the residents had previously performed the SSLF procedure. There was no difference in anatomical knowledge between the two groups. The intervention group showed a greater increase in their average confidence score compared with the control group: 4.0 ± 1.4 (95% CI 3.1–4.8) versus 2.6 ± 1.6 (95% CI 1.7–3.4) respectively, with p = 0.02. The intervention group also showed better objective scores in specific technical skills, such as instrument handling (p < 0.001), instrument movement/motion (p < 0.001), and speed (p = 0.01).
Conclusion
Our results demonstrate that inclusion of a pelvic model simulation significantly improves confidence and certain technical skills of novice trainees in performing SSLF.




Similar content being viewed by others
References
Karram MM, Ridgeway BM, Walters MD. Surgical treatment of vaginal apex prolapse. Urogynecology and reconstructive pelvic surgery, 4th ed. In: Walters MD, Karram MM, editors. Philadelphia: Mosby Elsevier; 2015. p. 360–82.
Katrikh AZ, Ettarh R, Kahn MA. Cadaveric nerve and artery proximity to sacrospinous ligament fixation sutures placed by a suture-capturing device. Obstet Gynecol. 2017;130(5):1033–8. https://doi.org/10.1097/AOG.0000000000002324.
Vaughan MH, Kim-Fine S, Hullfish KL, Smith TM, Siddiqui NY, Trowbridge ER. Validation of the simulated vaginal hysterectomy trainer. J Minim Invasive Gynecol. 2018;25(6):1101–6. https://doi.org/10.1016/j.jmig.2018.02.022.
Kisby CK, Baker MV, Green IC, Occhino JA. Teaching learners to raise the roof: a vaginal surgery simulator for apical suspension. Int Urogynecol J. 2019;30(10):1771–3. https://doi.org/10.1007/s00192-019-03985-y.
Preece R. The current role of simulation in urological training. Cent European J Urol. 2015;68(2):207–11. https://doi.org/10.5173/ceju.2015.522.
Gupta A, Herrera S, Kanitsch S, Kane L. Le Fort partial colpocleisis: a low-cost model. J Med Educ Curric Dev. 2018;5:2382120518801582. https://doi.org/10.1177/2382120518801582.
International Academy of Pelvic Surgery. Sim VaHT: simulated vaginal hysterectomy trainer. Available at https://academyofpelvicsurgery.com/2017/10/30/video-4-simvaht-simulated-vaginal-hysterectomy-trainer/ Accessed 1 March 2020.
Greer JA, Segal S, Salva CR, Arya LA. Development and validation of simulation training for vaginal hysterectomy. J Minim Invasive Gynecol. 2014;21(1):74–82. https://doi.org/10.1016/j.jmig.2013.06.006.
Petrikovets A, Fisher T, Krudy C, Sheyn D, Mangel J, Mahajan ST. LeFort colpocleisis: a step-by-step simulation video for female pelvic surgeons. Int Urogynecol J. 2018;29(6):917–9. https://doi.org/10.1007/s00192-017-3543-9.
Petrikovets A, Himler J, Henderson JW, et al. Complete colpectomy and colpocleisis: a model for simulation. Society of Gynecologic Surgeons (Videofest 13), 2016. http://www.sgsonline.org/index.php?option=com_content&view=article&id=255:2016-video-fest&catid=30:video-library&Itemid=142. Accessed 1 March 2020.
Oliphant S, Littleton EB, Gosman G, Sutkin G. Teaching the retropubic midurethral sling using a novel cadaver and model-based approach. Cureus. 2017;9(5):e1214.
Sabourin JN, Schulz JA, Flood CG. Improving resident competence and knowledge regarding tension-free vaginal tape procedure: an educational module. Female Pelvic Med Reconstr Surg. 2012;18(5):268–73.
Chong W, Downing K, Leegant A, Banks E, Fridman D, Downie S. Resident knowledge, surgical skill, and confidence in transobturator vaginal tape placement: the value of a cadaver laboratory. Female Pelvic Med Reconstr Surg. 2017;23(6):392–400.
Evans SKL, Myers EM, Anderson-Montoya B, Vilasagar S, Tarr ME. A cadaveric simulation model to teach suture placement during sacrospinous ligament fixation. Female Pelvic Med Reconstr Surg. 2019;https://doi.org/10.1007/s00192-017-3543-9.
Richter K, Albrich W. Long-term results following fixation of the vagina on the sacrospinal ligament by the vaginal route (vaginaefixatio sacrospinalis vaginalis). Am J Obstet Gynecol. 1981;141(7):811–6. https://doi.org/10.1016/0002-9378(81)90709-2.
Nichols DH. Sacrospinous fixation for massive eversion of the vagina. Am J Obstet Gynecol. 1982;142(7):901–4. https://doi.org/10.1016/s0002-9378(16)32539-x.
Martin JA, Regehr G, Reznick R, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997;84(2):273–8. https://doi.org/10.1046/j.1365-2168.1997.02502.x.
Van Hove PD, Tuijthof GJ, Verdaasdonk EG, Stassen LP, Dankelman J. Objective assessment of technical surgical skills. Br J Surg. 2010;97(7):972–87. https://doi.org/10.1002/bjs.7115.
Acknowledgements
Charles Khamis, MS, MBA, from Boston Scientific™, for assistance with cadaveric dissections; Youngju Pak for statistical analysis.
Funding
Grants received from the Committee of Interns and Residents in Los Angeles, CA (grant number: 031601–01-00), and Boston Scientific™ (grant number: ISRURO00070).
Author information
Authors and Affiliations
Contributions
Y. Takashima: project development, cadaveric dissection, involvement in the simulation session, data collection, data analysis, manuscript writing; S. Handler: project development, cadaveric dissection, involvement in the simulation session, manuscript writing; A. Zeno: project development, cadaveric dissection, involvement in the simulation session; B. Miyazaki: project development, cadaveric dissection, involvement in simulation session, manuscript writing; I. Del Canto: cadaveric dissection, involvement in the simulation session, data collection; T. Yazdany: project development, involvement in simulation session, manuscript writing; T. Le: project development, cadaveric dissection, involvement in the simulation session, manuscript writing.
Corresponding author
Ethics declarations
Financial disclaimer/conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takashima, Y., Handler, S.J., Zeno, A. et al. Use of pelvic model-based simulation for sacrospinous ligament fixation education in novice learners: a single-blinded randomized controlled trial. Int Urogynecol J 32, 897–903 (2021). https://doi.org/10.1007/s00192-020-04445-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04445-8