Abstract
Introduction and hypothesis
Vulvodynia is chronic debilitating burning vulvar pain or pain on contact. Although women who suffer from vulvodynia are more likely than others to experience co-morbid interstitial cystitis (IC) and urinary tract infections (UTIs), few studies have explored whether women with vulvodynia experience adverse urinary symptoms (lower urinary tract symptoms [LUTS]) in the absence of urological pain.
Methods
Two hundred and eleven participants with and 226 participants without clinically confirmed vulvodynia completed the Pelvic Pain and Urgency/Frequency (PUF) questionnaire and were scored using all questions, and then a subset of questions relating only to their current frequency and bother of urination during day and night, and the frequency, severity and bother of urgency after voiding. Total, symptom, and bother scores were compared in women with and without vulvodynia, and regression models estimated adjusted odds ratios and 95% confidence intervals for the various LUTS symptoms.
Results
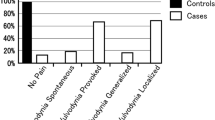
As expected, 40% of women with vulvodynia met the criteria for IC (PUF > 12) compared with 2% without vulvodynia. After excluding questions related to bladder or vulvovaginal pain, women with vulvodynia, compared with those without, were skewed toward higher PUF scores, including being 2.4 times more likely to report usually or always bothered by night-time voiding (95% CI 1.22–4.74), and 18 times more likely to report moderate/severe urgency after urination (95% CI 5.48–64.12).
Conclusions
Women with vulvodynia are substantially more likely to report voiding dysfunction and symptoms of urgency than women with no history of vulvar pain. These findings are independent of comorbid interstitial cystitis or history of UTIs.

Similar content being viewed by others
References
Moyal-Barracco M, Lynch PJ. ISSVD terminology and classification of vulvodynia: a historical perspective. J Reprod Med. 2003;49:772.
Bornstein J, Goldstein AT, Stockdale CK, Bergeron S, Pukall C, Zolnoun D, et al. ISSVD, ISSWSH, and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. J Sex Med. 2015;13:607–12.
Harlow BL, Kunitz CG, Nguyen RH, Rydell SA, Turner RM, MacLehose RF. Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. Am J Obstet Gynecol. 2014;210:40.e1–8.
Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc. 2003;58:82–8.
Gardella B, Porru D, Nappi RE, Daccò MD, Chiesa A, Spinillo A. Interstitial cystitis is associated with vulvodynia and sexual dysfunction—a case-control study. J Sex Med. 2011;8:1726–34.
Arnold LD, Bachmann GA, Rosen R, Rhoads GG. Assessment of vulvodynia symptoms in a sample of US women: a prevalence survey with a nested case control study. Am J Obstet Gynecol. 2007;196:128.e1–6.
Nguyen RH, Swanson D, Harlow BL. Urogenital infections in relation to the occurrence of vulvodynia. J Reprod Med. 2009;54:385–92.
Harlow BL, Caron RE, Parker SE, Chatterjea D, Fox MP, Nguyen RH. Recurrent yeast infections and vulvodynia: can we believe associations based on self-reported data? J Womens Health. 2017;26:1069–76.
Oakes JM, MacLehose RF, McDonald K, Harlow BL. Using administrative health care system records to recruit a community-based sample for population research. Ann Epidemiol. 2015;25:526–31.
Parsons CL, Dell J, Stanford EJ, Bullen M, Kahn BS, Waxell T, et al. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002;60:573–8.
National Heart, Lung, and Blood Institute. Clinical guidelines on identification, evaluation, and treatment of overweight and obesity in adults. Bethesda: National Institutes of Health, National Heart, Lung, and Blood Institute; 1998.
Khandker M, Brady SS, Stewart EG, Harlow BL. Is chronic stress during childhood associated with adult-onset vulvodynia? J Womens Health. 2014;23:649–56.
Arnold LD, Bachmann GA, Kelly S, Rosen R, Rhoads GG. Vulvodynia: characteristics and associations with co-morbidities and quality of life. Obstet Gynecol. 2006;107:617.
Kahn BS, Tatro C, Parsons CL, Willems JJ. Prevalence of interstitial cystitis in vulvodynia patients detected by bladder potassium sensitivity. J Sexual Med. 2010;7:996–1002.
Salonia A, Clementi MC, Graziottin A, Nappi RE, Castiglione F, Ferrari M, et al. Secondary provoked vestibulodynia in sexually active women with uncomplicated recurrent urinary tract infections. J Sex Med. 2013;10:2265–73.
Salonia A, Zanni G, Nappi RE, Briganti A, Dehò F, Fabbri F, et al. Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross-sectional study. Eur Urol. 2004;45:642–8.
Acknowledgements
The authors wish to thank Dr. Elizabeth Lukacz from the University of California San Diego and Dr. Tamara Bavendam from the National Institute of Diabetes and Digestive and Kidney Diseases for their peer review and advice on this article. No fee for this service was incurred. This research was supported by NIH-NICHD-R01 HD058608.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, Y., Harlow, B.L. The association of vulvar pain and urological urgency and frequency: findings from a community-based case–control study. Int Urogynecol J 30, 1871–1878 (2019). https://doi.org/10.1007/s00192-019-04052-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04052-2