Abstract
Introduction and hypothesis
Chronic pelvic pain is a debilitating condition, and establishing both an etiology and a successful management plan is challenging. Bladder pain syndrome (BPS) is one such etiology, with some studies reporting a prevalence of up to 50% in women with chronic pelvic pain (Van De Merwe et al. Eur Urol 53: 60–67, 2008; Cervigni and Natale Int J Urol 21: 85–88, 2014). This study aimed to assess the impact that investigative laparoscopy with treatment of endometriosis has on bladder pain syndrome in women with and without endometriosis.
Methods
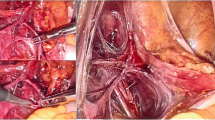
A prospective cohort study was conducted with participants recruited from a tertiary gynecology unit and the private rooms of participating gynecologists. Women included were those scheduled for laparoscopy for investigation of pelvic pain of > 6 months, aged 18–40 years. Each patient completed a preoperative questionnaire, and a standardized study operative report was used to collect laparoscopy findings. Any endometriosis found was treated with excisional surgery. Patients were then reviewed with the same questionnaire at 3, 6 and 12 months post-surgery.
Results
A total of 150 patients were included in the trial. Seventy-five percent of patients (n = 112/150) were diagnosed with endometriosis. Of them, 43% (n = 48/112) also had BPS. The overall BPS rate was 43% (n = 64/150). At 12 months, there was a significant reduction in overall pain and pelvic pain in all groups. Of the women with BPS, there was no difference in symptom score reduction between those with endometriosis treated and those without endometriosis. BPS resolved in 42% of women 12 months post-laparoscopy, regardless of whether endometriosis was diagnosed and treated or not. Of the women without BPS preoperatively, 14% developed de novo BPS at 12 months, regardless of whether endometriosis was diagnosed and treated or not.
Conclusion
Our findings show that BPS improves in the 12 months after investigative laparoscopy and treatment of endometriosis for chronic pelvic pain, regardless of presence or absence of endometriosis.

Similar content being viewed by others
References
National Action Plan for Endometriosis. The Department of Health. 2018. Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/endometriosis
Paulson JD, Delgado M. The relationship between interstitial cystitis and endometriosis in patients with chronic pelvic pain. JSLS. 2017;11:175–1812.
Chung MK, Chung RP, Gordon D. Intersitital cystitis and endometriosis in patients with chronic pelvic pain: the "evil twins" syndrome. JSLS. 2005;9:25–9.
Tirlapur SA, Kuhrt K, Chaliha C, Ball E, Meads C, Khan K. The “evil twin syndrome” in chronic pelvic pain: a systematic review of prevalence studies of bladder pain syndrome and endometriosis. Int J Surg. 2013;11:233–7.
Van De Merwe JP, Nordling J, Bouchelouche P, Bouchelouche K, Cervigni M, Daha LK, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008;53:60–7.
Hanno PM, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrom. J Urol. 2011;185(6):2162–70.
Hanno PM, et al. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53.
Cervigni M, Natale F. Gynecoloigcal disorders in bladder pain syndrome/interstitial cystitis patients. Int J Urol. 2014;21:85–8.
Cheng C, Rosamilia A, Healey M. Diagnosis of interstitial cystitis/bladder pain syndrome in women with chronic pelvic pain: a prospective observational study. Int Urogynecolo. 2011;10:1361–6.
Brewer ME, White WM, Klein FA, Klein LM, Waters WB. Validity of pelvic pain, urgency, and frequency questionnaire in patients with interstitial cystitis/painful bladder syndrome. Urology. 2007;70(4):646–9.
O’Leary MP, Sant GR, Fowler FJ Jr, Whitmore KE, Spolarich-Kroll J. The interstitial cystitis symptom index and problem index. Urology. 1997;49(5A Suppl):58–63.
Humphrey L, Arbuckle R, Moldwin R, et al. The bladder pain/interstitial cystitis symptom score: development, validation, and identification of a cut score. Eur Urol. 2012;61(2):271–9.
Cox A, Golda N, Nadeau G, Nickel JC, Carr L, Corcos J, et al. CUA guideline: diagnosis and treatment of interstitial cystitis/bladder pain syndrome. Can Urol Assoc J. 2016;10(5–6):E136–55.
Liu Y, Zhang W. Association between body mass index and endometriosis risk: a meta-analysis. Oncotarget. 2017;8(29):46928–36.
Propert KJ, Schaeffer AJ, Brensinger CM, Kusek J, Nyberg L. Landis R and the interstitial cystitis Data Base study group (2000) a prospective study of interstitial cystitis: results of longitudinal follow up of the interstitial cystitis data base cohort. the interstitial cystitis data base study group. J Urol. 163:1434.
Warren J, Greenberg P, Diggs C, Horne L, Langenberg P. A prospective early history of incident interstitial cystitis/painful bladder syndrome. J Urol. 2010;184:2333–8.
Suskind A, Berry S, Suttorp M, Elliott M, Clemens J (2014). Symptom Persistence in Communicty Cohort of Women with Intersitial Cystitis/Bladder Pain Syndrome (IC/BPS): 3, 6, 9, and 12 month follow up from the RICE Cohort. Int Urogynaecol J 25:1639–1643. C Jones, Nyberg L (1997) Epidemiology of Interstitial Cystitis. Urol 49(5) 2–8.
Allaire C, Williams C, Bodmer-Roy S, Zhu S, Arion K, Ambacher K, et al. Chronic pelvic pain in an interdisciplinary setting: 1-year prospective cohort. AJOG. 2018;12:114.
Tettamanti G, Nyman-Iliadou A, Pedersen NL, Bellocco R, Milsom I, Altman D. Influence of smoking, coffee, and tea consumption on bladder pain syndrome in female twins. Urology. 2011;77:1313–7.
Acknowledgements
Thank you to the medical staff of the Gynecology 2 Unit of the Royal Women’s Hospital, Melbourne, for their contribution of time to data collection and to the Australasian Gynecological Endoscopy and Surgery Society for the research grant supporting this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclaimer
This study received a 2016 Australasian Gynecological Endoscopy and Surgery Society (AGES) research grant.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 24 kb)
Rights and permissions
About this article
Cite this article
Collings, R., Healey, M., Dior, U. et al. Effect of investigative laparoscopy on bladder pain syndrome: a prospective cohort trial. Int Urogynecol J 31, 1583–1591 (2020). https://doi.org/10.1007/s00192-019-04023-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04023-7



