Abstract
Introduction and hypothesis
Uterine prolapse is a common health problem and the number of surgical procedures is increasing. No consensus regarding the surgical strategy for repair of uterine prolapse exists. Vaginal hysterectomy (VH) is the preferred surgical procedure worldwide, but uterus-preserving alternatives including the Manchester procedure (MP) are available. The objective was to evaluate if VH and the MP are equally efficient treatments for uterine prolapse with regard to anatomical and symptomatic outcome, quality of life score, functional outcome, re-operation and conservative re-intervention rate, complications and operative outcomes.
Methods
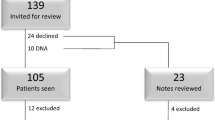
We systematically searched Embase, PubMed, the Cochrane databases, Clinicaltrials and Clinical trials register using the MeSh terms “uterine prolapse”, “uterus prolapse”, “vaginal prolapse” “pelvic organ prolapse”, “prolapsed uterus”, “Manchester procedure” and “vaginal hysterectomy”. No limitations regarding language, study design or methodology were applied. In total, nine studies published from 1966 to 2014 comparing the MP to VH were included.
Results
The anatomical recurrence rate for the middle compartment was 4–7 % after VH, whereas recurrence was very rare after the MP. The re-operation rate because of symptomatic recurrence was higher after VH (9–13.1 %) compared with MP (3.3–9.5 %) and more patients needed conservative re-intervention (14–15 %) than after MP (10–11 %). After VH, postoperative bleeding and blood loss tended to be greater, bladder lesions and infections more frequent and the operating time longer.
Conclusions
This review is in favour of the MP, which seems to be an efficient and safe treatment for uterine prolapse. We suggest that the MP might be considered a durable alternative to VH in uterine prolapse repair.

Similar content being viewed by others
References
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the women’s health initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–6.
Olsen AL, Smith VJ, Bergstrom JO, Colling JCR, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson FM. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Elterman DS, Chughtai BI, Vertosick E, Maschino A, Eastham JA, Sandhu JS. Changes in pelvic organ prolapse surgery in the last decade among United States urologists. J Urol. 2014;191(4):1022–7.
Brown JS, Waetjen LE, Subak LL, Thom DH, Van Den Eeden S, Vittinghoff E. Pelvic organ prolapse surgery in the United States, 1997. Am J Obstet Gynecol. 2002;186(4):712–6.
Vanspauwen R, Seman E, Dwyer P. Survey of current management of prolapse in Australia and New Zealand. Aust N Z J Obstet Gynaecol. 2010;50(3):262–7.
Jha S, Moran P. The UK national prolapse survey: 5 years on. Int Urogynecol J. 2011;22(5):517–28.
Oversand SH, Staff AC, Spydslaug AE, Svenningsen R, Borstad E. Long-term follow-up after native tissue repair for pelvic organ prolapse. Int Urogynecol J. 2014;25(1):81–9.
Ünlübilgin E, Sivaslioglu A, Ilhan T, Kumtepe Y, Dölen I. Which one is the appropriate approach for uterine prolapse: Manchester Procedure or vaginal hysterectomy? Turk Klin J Med Sci. 2013;33(2):321–5.
Miedel A, Tegerstedt G, Mörlin B, Hammarström M. A 5-year prospective follow-up study of vaginal surgery for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(12):1593–601.
De Boer TA, Milani AL, Kluivers KB, Withagen MIJ, Vierhout ME. The effectiveness of surgical correction of uterine prolapse: cervical amputation with uterosacral ligament plication (modified Manchester) versus vaginal hysterectomy with high uterosacral ligament plication. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(11):1313–9.
Iliev VN. Uterus preserving vaginal surgery versus vaginal hysterectomy for correction of female pelvic organ prolapse. Pril (Makedon Akad Nauk Umet Odd Med Nauki). 2014;35(1):243–7.
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn. 1995;14(2):131–9.
van der Vaart CH, de Leeuw JRJ, Roovers J-PWR, Heintz APM. Measuring health-related quality of life in women with urogenital dysfunction: the urogenital distress inventory and incontinence impact questionnaire revisited. Neurourol Urodyn. 2003;22(2):97–104.
Thys SD, Coolen A-L, Martens IR, Oosterbaan HP, Roovers J-PWR, Mol B-W, et al. A comparison of long-term outcome between Manchester Fothergill and vaginal hysterectomy as treatment for uterine descent. Int Urogynecol J. 2011;22(9):1171–8.
Rubin A. Complications of vaginal operations for pelvic floor relaxation. Am J Obstet Gynecol. 1966;95(7):972–4.
Ottesen M, Utzon J, Kehlet H, Ottesen BS. Vaginal surgery in Denmark in 1999–2001. An analysis of operations performed, hospitalization and morbidity. Ugeskr Laeger. 2004;166(41):3598–601.
Thomas AG, Brodman ML, Dottino PR, Bodian C, Friedman F, Bogursky E. Manchester procedure vs. vaginal hysterectomy for uterine prolapse. A comparison. J Reprod Med. 1995;40(4):299–304.
Kalogirou D, Antoniou G, Karakitsos P, Kalogirou O. Comparison of surgical and postoperative complications of vaginal hysterectomy and Manchester procedure. Eur J Gynaecol Oncol. 1996;17(4):278–80.
Dietz V, Koops SES, van der Vaart CH. Vaginal surgery for uterine descent; which options do we have? A review of the literature. Int Urogynecol J. 2008;20(3):349–56.
Detollenaere RJ, den Boon J, Vierhout ME, van Eijndhoven HWF. Uterussparende chirurgie versus vaginale hysterectomie als behandeling van descensus uteri. Litteratuuronderzoek Ned Tijdschr Geneeskd. 2011;155:A3623.
Shull BL, Bachofen C, Coates KW, Kuehl TJ. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183(6):1365–73, discussion 1373–1374.
Aigmueller T, Dungl A, Hinterholzer S, Geiss I, Riss P. An estimation of the frequency of surgery for posthysterectomy vault prolapse. Int Urogynecol J. 2010;21(3):299–302.
Frick AC, Walters MD, Larkin KS, Barber MD. Risk of unanticipated abnormal gynecologic pathology at the time of hysterectomy for uterovaginal prolapse. Am J Obstet Gynecol. 2010;202(5):507.e1–4.
Hanson GE, Keettel WC. The Neugebauer-Le Fort operation. A review of 288 colpocleises. Obstet Gynecol. 1969;34(3):352–7.
Jones KA. Hysterectomy at the time of colpocleisis: a decision analysis. Int Urogynecol J. 2016;27(5):805–10.
Dietz V. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J. 2010;21(2):209–16.
Lin T-Y. Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc. 2005;104(4):249–53.
Barski D, Otto T, Gerullis H. Systematic review and classification of complications after anterior, posterior, apical, and total vaginal mesh implantation for prolapse repair. Surg Technol Int. 2014;24:217–24.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;4:CD004014.
FDA. FDA Public Health Notification: Serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. 2008.
FDA. FDA Update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse: FDA Safety Communication. 2011.
Scientific Committee on Emerging and Newly Identified Health Risks, SCENIHR. Opinion on the safety of surgical meshes used in urogynecological surgery. European Commission; 2015.
Frick AC. Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg. 2013;19(2):103–9.
Korbly NB. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470–6.
Acknowledgements
We gratefully acknowledge doctor Svetlana Rygaard Nielsen for translating the Russian study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
CK Tolstrup received travel expenses and conference fees for the EUGA Annual Congress Leading Lights 2015 from by Astellas Pharma; Gunnar Lose received research grants from Astellas Pharma and consultant fees from Contura; Niels Klarskov received research grants from Astellas Pharma. None of the other authors received external funding for the study.
Authors’ contributions
CK Tolstrup: protocol development, data collection, data analysis, manuscript writing/editing.
G Lose: protocol development, manuscript editing.
N Klarskov: protocol development, data analysis, manuscript editing.
Rights and permissions
About this article
Cite this article
Tolstrup, C.K., Lose, G. & Klarskov, N. The Manchester procedure versus vaginal hysterectomy in the treatment of uterine prolapse: a review. Int Urogynecol J 28, 33–40 (2017). https://doi.org/10.1007/s00192-016-3100-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3100-y