Abstract
Introduction and hypothesis
Robotic assistance simplifies laparoscopic procedures. We hypothesize that robot-assisted sacrocolpopexy is a rapid and safe procedure with satisfying short-term and midterm functional results.
Methods
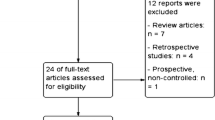
After informed consent, we enrolled 101 consecutive patients undergoing sacrocolpopexy at Alfried Krupp Hospital, Essen, Germany. After a median follow-up of 22 months, we assessed midterm functional results as the primary endpoint. Secondary endpoints included surgical duration, blood loss, intraoperative complications, and postoperative complications. We described frequencies as counts (percent) and continuous data as median [interquartile range (Q1–Q3)] or mean [standard deviation (SD)], as appropriate.
Results
We enrolled 101 patients. The mean age was 69 years (SD 11); 75 women (74.3 %) had undergone previous abdominal surgery. Among the patients, 95 (94.1 %) presented with anterior vaginal wall prolapse Baden-Walker grade 2–3, 74 (73.3 %) vaginal vault prolapse, and 9 (8.9 %) concomitant rectocele. Fifty (50 %) patients underwent a modified Burch procedure in addition to sacrocolpopexy. The median surgical duration was 96 min (Q1–Q3 83–130). There were six (5.9 %) minor intraoperative complications but no conversions to open surgery. Postoperatively, we registered five (4.9 %) Clavien-Dindo grade I complications, three (3.0 %) grade II complications, and one (1.0 %) grade III complication. After a median follow-up of 22 months (Q1–Q3 12–49), the patients reported significant decreased impact of pelvic organ prolapse (POP) on quality of life as well as bother resulting from POP symptoms. The overall success rate, defined as none or minor impact of POP on quality of life, was 75 %.
Conclusions
In this single-surgeon study, robot-assisted sacrocolpopexy was a safe and rapidly performed procedure that achieved good medium-term functional results.


Similar content being viewed by others
References
Samuelsson EC, Victor FT, Tibblin G, Svärdsudd KF (1999) Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol 180(2 Pt 1):299–305
Deval B, Haab F (2003) What’s new in prolapse surgery? Curr Opin Urol 13(4):315–323
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506
Subak LL, Waetjen LE, van den Eeden S, Thom DH, Vittinghoff E, Brown JS (2001) Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol 98(4):646–651
Luber KM, Boero S, Choe JY (2001) The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol 184(7):1496–1501, discussion 1501–1503
Ganatra AM, Rozet F, Sanchez-Salas R et al (2009) The current status of laparoscopic sacrocolpopexy: a review. Eur Urol 55(5):1089–1103
Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014. doi:10.1002/14651858.CD004014.pub5
Cosson M, Rajabally R, Bogaert E, Querleu D, Crépin G (2002) Laparoscopic sacrocolpopexy, hysterectomy, and Burch colposuspension: feasibility and short-term complications of 77 procedures. JSLS 6(2):115–119
Gadonneix P, Ercoli A, Salet-Lizée D et al (2004) Laparoscopic sacrocolpopexy with two separate meshes along the anterior and posterior vaginal walls for multicompartment pelvic organ prolapse. J Am Assoc Gynecol Laparosc 11(1):29–35
Hsiao KC, Latchamsetty K, Govier FE, Kozlowski P, Kobashi KC (2007) Comparison of laparoscopic and abdominal sacrocolpopexy for the treatment of vaginal vault prolapse. J Endourol 21(8):926–930
Klauschie JL, Suozzi BA, O’Brien MM, McBride AW (2009) A comparison of laparoscopic and abdominal sacral colpopexy: objective outcome and perioperative differences. Int Urogynecol J Pelvic Floor Dysfunct 20(3):273–279
Paraiso MF, Walters MD, Rackley RR, Melek S, Hugney C (2005) Laparoscopic and abdominal sacral colpopexies: a comparative cohort study. Am J Obstet Gynecol 192(5):1752–1758
Sundaram CP, Venkatesh R, Landman J, Klutke CG (2004) Laparoscopic sacrocolpopexy for the correction of vaginal vault prolapse. J Endourol 18(7):620–623, discussion 623–624
Akl MN, Long JB, Giles DL et al (2009) Robotic-assisted sacrocolpopexy: technique and learning curve. Surg Endosc 23(10):2390–2394
Daneshgari F, Kefer JC, Moore C, Kaouk J (2007) Robotic abdominal sacrocolpopexy/sacrouteropexy repair of advanced female pelvic organ prolapse (POP): utilizing POP-quantification-based staging and outcomes. BJU Int 100(4):875–879
Elliott DS, Krambeck AE, Chow GK (2006) Long-term results of robotic assisted laparoscopic sacrocolpopexy for the treatment of high grade vaginal vault prolapse. J Urol 176(2):655–659
Geller EJ, Siddiqui NY, Wu JM, Visco AG (2008) Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol 112(6):1201–1206
Kramer BA, Whelan CM, Powell TM, Schwartz BF (2009) Robot-assisted laparoscopic sacrocolpopexy as management for pelvic organ prolapse. J Endourol 23(4):655–658
Serati M, Bogani G, Sorice P et al (2014) Robot-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis of comparative studies. Eur Urol 66(2):303–318. doi:10.1016/j.eururo.2014.02.053
Ploumidis A, Spinoit AF, De Naeyer G et al (2014) Robot-assisted sacrocolpopexy for pelvic organ prolapse: surgical technique and outcomes at a single high-volume institution. Eur Urol 65(1):138–145. doi:10.1016/j.eururo.2013.05.054
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Baessler K, O’Neill SM, Maher CF, Battistutta D (2010) A validated self-administered female pelvic floor questionnaire. Int Urogynecol J 21(2):163–172. doi:10.1007/s00192-009-0997-4
Digesu GA, Khullar V, Cardozo L, Robinson D, Salvatore S (2005) P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J Pelvic Floor Dysfunct 16(3):176–181. doi:10.1007/s00192-004-1225-x, discussion 181
Culligan PJ, Gurshumov E, Lewis C et al (2014) Subjective and objective results 1 year after robotic sacrocolpopexy using a lightweight Y-mesh. Int Urogynecol J 25(6):731–735. doi:10.1007/s00192-013-2265-x
Conflicts of interest
Stephan Buse acts as proctor for the da Vinci Si-HD® System, Intuitive Surgical, Inc., Sunnyvale, CA, USA. C.E. Hach, J. Krude, A. Reitz, M. Reiter, and A. Haferkamp declare that they have no conflicts of interest.
Authors’ contributions
C.E. Hach: protocol/project development, data collection, data analysis, manuscript writing. J. Krude: data collection. A. Reitz: data analysis, manuscript editing. M. Reiter: data analysis, manuscript editing. A. Haferkamp: data analysis, manuscript editing. S. Buse: protocol/project development, data analysis, manuscript writing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hach, C.E., Krude, J., Reitz, A. et al. Midterm results of robot-assisted sacrocolpopexy. Int Urogynecol J 26, 1321–1326 (2015). https://doi.org/10.1007/s00192-015-2688-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2688-7