Abstract
In this study, I examine the role of health insurance cover in improving access to healthcare services and consequently its role in improving health outcomes for dependent children. I utilize differences in temporal variation of insurance cover for dependent children and their cousins, within the same Indonesian household to estimate the effect. By comparing dependent children of different biological parents, living in the same household, this study avoids potential confounders for healthcare demand, such as health endowment due to nutrition and hygiene. I find that dependent children of government employees have increased access to health insurance. In terms of healthcare use, I find no impact of insurance in providing access to preventive care as an outpatient. Instead, insurance status positively impacted first time and repeat visits to private facilities for curative care only. Insured children were 4.4 per cent more likely, than uninsured cousins, to access first-time curative care and make 63 per cent more repeat visits as an outpatient. In contrast, for inpatient services, insured children sought care at public facilities. Insurance did not have a positive impact on health outcomes for dependents. The results are robust to an instrumental variable estimation, alongside household fixed effects, which addresses concerns on potential endogeneity of insurance cover.
Similar content being viewed by others
Notes
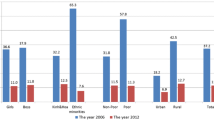
Based on calculation from the Indonesian family life survey sample.
see Sect. 2 for details.
BPDPK—Badan Penyelenggara Dana pemeliharaan Kesehatan.
Data structure in the first IFLS round (1993) does not enable identification of hierarchical family relationships and is thus not used for this study.
For sensitivity checks of the results, I also create an extended sample, which retains households with either atleast one uninsured sibling or uninsured cousin in step 2.
Jamsostek was the Askes equivalent for formal workers in private corporations and their families. Due to opt-out conditions, the coverage for parents was sparse and such dependents are not used in this study.
People either having systolic pressure (arteries pressure during contraction of the heart muscle) of 140–160 mmHg or having diastolic pressure (pressure during rest period intervening heart beats) of 90 to 100 mmHg were categorized as having Stage-1 hypertension.
Estimates and post-estimation tests are retrieved using the xtivreg2 command in Stata (Schaffer 2010).
The Sanderson and Windmeijer (2016) F-statistic, a notable correction over the Angrist-Pischke F, is only purposeful in the case of multiple endogenous regressors.
For repeated observations of dependents within a household over time, one can reasonably expect correlation in error terms.
Similar to the previous sample, I exclude ever married or employed dependents.
The point estimate for a 10% rise in X in a lin-log model is 0.095 * \({\hat{\beta }}\); \(\log (110/100)=0.095\).
References
Achyuta A, Anant N (2016) Endowments at birth and parents investments in children. Econ J 126(593):781-820
Adriana C, Emily C (2013) Effects of subsidized health insurance on newborn health in a developing country. Econ Dev Cult Change 61(3):633–658
Anderson TW, Herman R (1949) Estimation of the parameters of a single equation in a complete system of stochastic equations. Ann Math Stat 20(1):46–63
Angrist Joshua D, Jorn-Steffen P (2009) Mostly harmless econometrics: an empiricists companion. Princeton University Press, New Jersey
Anne F, Rebecca T (2019) The effects of health insurance within families: experimental evidence from nicaragua. World Bank Econ Rev 33(3):736–749
Baum Christopher F, Schaffer Mark E, Steven Stillman (2002) IVREG2: stata module for extended instrumental variables/2SLS and GMM estimation. Statistical Software Components, Boston College Department of Economics
Baum CF, Schaffer ME, Stillman S (2007) Enhanced routines for instrumental variables/generalized method of moments estimation and testing. Stand Genomic Sci 7(4):465–506
Bernal N, Carpio MA, Klein TJ (2017) The effects of access to health insurance: evidence from a regression discontinuity design in Peru. J Publ Econ 154:122–136
Boudreaux Michel H, Ezra G, Mcalpine Donna D (2016) The long-term impacts of medicaid exposure in early childhood: evidence from the programs origin. J Health Econ 45:161–175
BPJS (2018) Service guide for national health insurance - Indonensian health card. Tech. rept, BPJS
Budi H, Subhash P (2009) The selection of an appropriate count data model for modelling health insurance and health care demand: case of Indonesia. Int J Environ Res Publ Health 7(1):9–27
Budi H, Hasbullah T, Hengjin D, Rainer S (2004) The effects of mandatory health insurance on equity in access to outpatient care in Indonesia. Health Policy Plan 19(5):322–335
Budi A, De A, Souares M, Sauerborn R (2013) The impact of health insurance programs on out-of-pocket expenditures in indonesia: an increase or a decrease? Int J Environ Res Public Health 10(7):2995–3013
Calomiris Charles W, Indira R (1998) The role of ROSCAs: lumpy durables or event insurance? J Dev Econ 56:207–216
David C, Hildreth Andrew KG, Shore-Sheppard Lara D (2004) The measurement of medicaid coverage in the SIPP: evidence from a comparison of matched records. J Bus Econ Stat 22(4):410–420
Douglas A, Janet C (2011) Killing me softly: the fetal origins hypothesis. J Econ Perspect 25(3):153–172
Eleanor S, Frank W (2016) A weak instrument F-test in linear IV models with multiple endogenous variables. J Econ 190:212–221
Fang H, Keane MP, Silverman D (2008) Sources of advantageous selection: evidence from the medigap insurance market. J Polit Econ 116(2):303–350
Frank K, Richard P (2006) Generalized reduced rank tests using the singular value decomposition. J Econ 133(1):97–126
Grant M, Diana P, Marcos VH (2013) Risk protection, service use, and health outcomes under colombias health insurance program for the poor. Am Econ J Appl Econ 5(4):61–91
Hasbullah T (2003) Social health insurance in Indonesia: current status and the proposed national health insurance. Tech. rept, WHO SEARO, New Delhi
Janet C, Jonathan G (1996) Health insurance eligibility, utilization of medical care, and child health. Q J Econ 111(2):431–466
Janet C, Sandra D, Wanchuan L (2008) Has public health insurance for older children reduced disparities in access to care and health outcomes? J Health Econ 27:1567–1581
Marcus D, Karen M (2016) The effect of medicare eligibility on spousal insurance coverage. Health Econ 25(5):591–605
Michael A, Carlos D, Tal G (2012) The effect of health insurance coverage on the use of medical services. Am Econ J Econ Pol 4(1):1–27
Newacheck Paul W, Stoddard Jeffrey J, Hughes Dana C, Pearl Michelle P (1998) Health insurance and access to primary care for children. N Engl J Med 338(8):513–519
Olson Lynn M, Tang Suk-fong S, Newacheck Paul W (2005) Children in the United States with discontinuous health insurance coverage. N Engl J Med 353(4):382–391
Pascale J (2001) Measuring private and public health coverage: results from a split-ballot experiment on order effects 1. In: Proceedings of the annual meeting of the american statistical association
Prashant B, Vellesen LK, Christopher N (2013) Early life health interventions and academic achievement. Am Econ Rev 103(5):1862–1891
Rachel P, Levine David I (2011) Adverse selection based on observable and unobservable factors in health insurance in Rural Cambodia. Tech. rept, Agence Française de Développement, Paris
Rokx C, Schieber G, Harimurti P, Tandon A, Somanathan A (2009) Health financing in Indonesia: a reform roadmap. The World Bank
Schaffer ME (2010) XTIVREG2: stata module to perform extended IV/2SLS, GMM and AC/HAC. LIML and k-class regression for panel data models, Statistical Software Components, Boston College Department of Economics
Sommers Benjamin D (2006) Insuring children or insuring families: do parental and sibling coverage lead to improved retention of children in Medicaid and CHIP? J Health Econ 25(6):1154–1169
Stock JH, Yogo M (2005) Testing for weak instruments in linear IV regression. In: Andrews DWK (ed) Identification and inference for econometric models - essays in honor of thomas rothenberg. Cambridge University Press, Cambridge, pp 80–108
Sven N, Owen O (2017) Progressive universalism? the impact of targeted coverage on health care access and expenditures in Peru. Health Econ (United Kingdom) 26(12):179–203
Timothy B, Stephen C, Glenn L (1993) American economic association the economics of rotating savings and credit associations. Am Econ Rev 83(4):792–810
Wen HH, Ming LH, Ting YT (2020) Patient cost-sharing and healthcare utilization in early childhood: evidence from a regression discontinuity design. Am Econ J Econ Policy 12(3):238–278
Funding
The author declares that no funding was received to assist with conducting this study or in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that he has no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: sensitivity check—using the sibling and cousins sample
Appendix: sensitivity check—using the sibling and cousins sample
Rights and permissions
About this article
Cite this article
Kolukuluri, K. Healthcare utilization and outcomes for insured dependent children: evidence from Indonesia. Empir Econ 63, 945–977 (2022). https://doi.org/10.1007/s00181-021-02146-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00181-021-02146-9