Abstract
Purpose
Meniscal tears are common and may impair knee function and biomechanics. This meta-analysis compared meniscal repair versus resection in patients with symptomatic meniscal tears in terms of patient-reported outcomes measures (PROMs), joint width, surgical failure, and rate of progression to osteoarthritis (OA) at conventional radiography.
Methods
This study was conducted according to the 2020 PRISMA statement. In August 2023, the following databases were accessed: PubMed, Web of Science, Google Scholar, and Embase. Two reviewers independently performed the analysis and a methodological quality assessment of the included studies. All the clinical investigations which compared repair versus resection of meniscal tears were accessed.
Results
Data from 20 studies (31,783 patients) were collected. The mean BMI was 28.28 ± 3.2 kg/m2, and the mean age was 37.6 ± 14.0 years. The mean time elapsed from injury to surgery was 12.1 ± 10.2 months and the mean medial joint width was 4.9 ± 0.8 mm. Between studies comparability at baseline was found in age, women, BMI, time from injury to surgery and length of the follow-up, PROMs, medial joint width, and stage of OA. The resection group demonstrated a greater Lysholm score (P = 0.02). No difference was found in the International Knee Documentation Committee (P = 0.2). Nine studies reported data on the rate of failures at a mean of 63.00 ± 24.7 months. No difference was found between the two groups in terms of persistent meniscal symptoms (P = 0.8). Six studies reported data on the rate of progression to total knee arthroplasty at a mean of 48.0 ± 14.7 months follow-up. The repair group evidenced a lower rate of progression to knee arthroplasty (P = 0.0001). Six studies reported data on the rate of advanced knee OA at a mean of 48.0 ± 14.7 months of follow-up. The repair group evidenced a lower rate of advanced knee OA (P = 0.0001). No difference was found in the mean joint space width (P = 0.09).
Conclusion
Meniscal repair is associated with a lower progression to knee osteoarthritis at approximately six years of follow-up compared to partial meniscectomy. No difference in PROMs, medial joint width, and failures were evidenced.
Level of evidence
Level III, meta-analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal tears are common and increase with age [41, 57]. Squatting, kneeling, crawling, chair sitting while driving, stair climbing, lifting items, and walking are associated with acute meniscal tears [39, 61, 79]. Both the lateral and medial menisci help preserve the knee biomechanics, and are important for shock absorption, joint stability, joint lubrication, and proprioception [6, 66, 90]. Meniscal tears have different aetiologies and injury patterns [44, 47, 60]. First, a distinction is made between acute and degenerative tears [39, 56]. Acute tears are commonly the result of trauma or sports injuries. The development of degenerative tears is caused by increasing age, chronic joint instability, and malalignment [15, 52, 58, 96]. When planning management, the shape, form, and location of the tears must be considered [14, 57]. The most common tear patterns are horizontal tears, bucket-handle tears, longitudinal tears, oblique or flap tears, radial tears, meniscal root tears, and complex tears consisting of a combination of different tear morphologies [3, 10, 13, 67]. Total or partial meniscectomy was considered the gold standard in the management of meniscal injuries [9, 21]. However, the loss of meniscal function and the altered biomechanics of the knee have caused a concern [32, 53]. In this context, the number of clinical studies evaluating strategies for meniscal repair has recently increased [1, 11, 22, 54]. In the past few decades, several techniques for meniscal repair have been advocated [28, 80, 89]. Meniscal repair led to a satisfactory healing rate, restoring knee biomechanics and function, and preventing the development of long-term complications [9, 87]. However, arthroscopic meniscectomy is still commonly performed, and the clinical advantages of meniscal repair are often undervalued.
This meta-analysis compared meniscal repair versus resection in patients with symptomatic meniscal tears in terms of patient-reported outcomes measures (PROMs), joint width, surgical failure, and rate of progression to osteoarthritis (OA) at conventional radiography. It was hypothesised that meniscal repair performs better compared to meniscal resection.
Methods
Eligibility criteria
All the clinical investigations which compared repair versus resection of meniscal tears were accessed. Only studies published in peer reviewed journals were considered. According to the authors’ language capabilities, articles in English, German, Italian, French and Spanish were eligible. Only studies with level I to IV of evidence, according to Oxford Centre of Evidence-Based Medicine [37], were considered. Studies which enhanced meniscal surgery with regenerative therapies (e.g., platelet rich plasma, mesenchymal stem cells) were not included. All types of repairs were included irrespective of the surgical technique and materials. All types of meniscal tears were considered, irrespective to their aetiology, previous conservative management, location, or extend. Only studies with a minimum of 12 months of follow-up were considered. Reviews, opinions, letters, and editorials were not considered. Animals, in vitro, biomechanics, computational, and cadaveric studies were not eligible, nor were those evaluating experimental physiotherapeutic protocols. Missing quantitative data under the outcomes of interests warranted the exclusion of the study.
Search strategy
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the 2020 PRISMA statement [69]. The following PICOT algorithm was established:
-
P (Problem): meniscal tears;
-
I (Intervention): meniscal repair;
-
C (Comparison): meniscal resection;
-
O (Outcomes): PROMs, medial joint width, rate of OA and failure;
-
T (Timing): minimum 12 months of follow-up.
In August 2023, the following databases were accessed: PubMed, Web of Science, Google Scholar, and Embase with no time constrain. The algorithm used for the literature search is shown in supplementary material.
Selection and data collection
Two authors (**;**) independently performed the database search. All the resulting titles were screened by hand and the abstracts were accessed. The full text of the abstracts which matched the topic of interest was accessed. A cross reference of the bibliography of the full-text articles was also performed for inclusion. Disagreements were debated and mutually solved by the authors. In case of further disagreements, a third senior author (**) took the final decision.
Data items
Two authors (**;**) independently performed data extraction. The following data at baseline were extracted: author, year of publication and journal, length of the follow-up, number of patients and their mean age and BMI. Data concerning the following PROMs were collected at baseline and at last follow-up: Lysholm Knee Scoring Scale [51] and International Knee Documentation Committee (IKDC) [35]. The minimum clinically important difference (MCID) for the Lysholm score was 10/100 and 15/100 for the IKDC [2, 40, 64]. Data on the width medial joint compartment and stage of OA at conventional radiography were collected at baseline and at the last follow-up. The Kellgren–Lawrence grading score [74] was used to assess the stage of OA. Data on the rate of failure and progression to TKA (total knee arthroplasty) were collected. Failures were defined as the recurrence of symptomatic meniscal tears confirmed by imaging, or the need for subsequential surgery.
Assessment of the risk of bias
Two reviewers (**;**) independently evaluated the risk of bias of the extracted studies. Disagreements were solved by a third author (**). The software Review Manager 5.3 (The Nordic Cochrane Collaboration, Copenhagen) was used. The following endpoints were evaluated: selection, detection, performance, attrition, reporting, and other bias.
Synthesis methods
The statistical analyses were performed by the main author (**) following the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions [34]. For descriptive statistics, the IBM SPSS software version 25 was used. The arithmetic mean and standard deviation were used. The student t test was performed to assess baseline comparability, with values of P > 0.1 considered satisfactory. For the meta-analyses, the software Review Manager 5.3 (The Nordic Cochrane Collaboration, Copenhagen) was used. For continuous data, the inverse variance method with mean difference (MD) effect measure was used. For binary data, the Mantel–Haenszel method with odd ratio (OR) effect measure was used. The CI was set at 95% in all the comparisons. Heterogeneity was assessed using \(\chi\)2 and Higgins-I2 tests. If \(\chi\)2 > 0.05, no statistically significant heterogeneity was found, and a fixed model effect was used. If \(\chi\)2 < 0.05 and Higgins-I2 > 60% high heterogeneity was found, and a random model effect was used for analysis. Values of P < 0.05 were considered statistically significant. To assess the risk of publication bias, the funnel plot of the most commonly reported outcome was performed. Egger’s linear regression was performed through the STATA MP Software version 16 (StataCorp, College Station, USA) to assess funnel plot asymmetry, with values of P < 0.05 indicating statistically significant asymmetry.
Results
Study selection
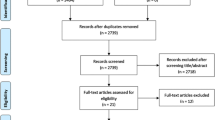
The literature search resulted in 837 articles. Of them, 420 were excluded as they were duplicates. A further 389 articles were excluded as they did not match the eligibility criteria: study type and design (N = 285), not comparing meniscal repair versus resection (N = 97), augmentation with cell therapies (N = 10), and language limitations (N = 5). A further 8 studies were excluded as they missed quantitative data under the outcomes of interests. Finally, 20 comparative studies were included: 16 retrospective and four prospective clinical investigations. The results of the literature search are shown in Fig. 1.
Analysis of publication bias
To evaluate the risk of publication bias, the funnel plot of the most reported outcome (failure) was evaluated. The Egger’s test did not identify any statistically significant asymmetry (P = 0.9), indicating acceptable risk of publication bias. The funnel plot is shown in Fig. 2.
Risk of bias assessment
Given the lack of randomised controlled trials included in the present investigation, the risk of selection bias was moderate to high. Few authors performed assessor blinding, leading to a moderate risk of detection bias. No authors performed patient blinding, which lead to a high risk of performance bias. The risk of attrition and reporting biases were moderate, as was the risk of other bias. Concluding, the risk of bias graph evidenced a moderate quality of the methodological assessment (Fig. 3).
Study characteristics and results of individual studies
Data from 31,783 patients were collected. The mean BMI was 28.3 ± 3.2 kg/m2, and the mean age was 37.6 ± 14.0 years. The mean time elapsed from injury to surgery was 12.1 ± 10.2 months, and the mean medial joint width was 4.9 ± 0.8 mm. The generalities and demographics of the included studies are shown in Table 1.
Baseline comparability
Between studies comparability at baseline was found in age, women, BMI, time from injury to surgery and length of follow-up, PROMs, medial joint width, and stage of OA. Baseline comparability is shown in Table 2.
PROMs
The resection group demonstrated a greater Lysholm score (MD 4.0; 95% CI 0.52–7.49; P = 0.02). However, this difference does not exceed the MCID. No difference was found in IKDC (P = 0.2). These results are shown in Fig. 4.
Failures
Nine studies reported data on failures at a mean of 63.00 ± 24.7 months [12, 17, 23, 75, 76, 81, 84, 85, 92]. No difference was found in the rate of failures (P = 0.8, Fig. 5).
Progression to osteoarthritis
Six studies reported data on the rate of progression to total knee arthroplasty [12, 17, 24, 46, 84, 92] at a mean of 48.0 ± 14.7 months follow-up. The repair group evidenced a lower rate of progression to TKA (OR0.51; 95% CI 0.39–0.69; P = 0.0001).
Six studies reported data on the rate of advanced knee OA [12, 17, 24, 46, 84, 92] at a mean of 48.0 ± 14.7 months follow-up. The repair group evidenced a lower rate of advanced knee OA (OR 0.51; 95% CI 0.39–0.69; P = 0.0001). No difference was found in the mean joint space width (P = 0.09). These results are shown in Fig. 6.
Discussion
According to the main findings of the present study, meniscal repair is associated with a lower progression to knee osteoarthritis at approximately six years of follow-up compared to partial meniscectomy. No difference in PROMs, medial joint width, and failures were evidenced.
Paxton et al. [70] reported in a systematic review that meniscal repair carries higher reoperation rate. No further between-groups differences were evidenced. Xu et al. [95], in a recent meta-analysis of seven studies, concluded that meniscal repair achieves greater PROMs and a lower failure rate. Faucett et al. [29] recently conducted a meta-analysis of nine studies evaluating acute tears of the medial meniscus root. Similarly, repair resulted in a lower rate of progression of OA compared to total resection or non-operative treatment [29]. Eseonu et al. [27], in a recent systematic review of 11 studies, evidenced that meniscal repair leads to a lower rate of progression of OA compared to meniscal resection and conservative management. The present meta-analysis improves the number of clinical investigations included for analysis and allows to analyse the rate of progression to OA in terms of joint space width, imaging, and rate of TKA.
Several factors influence the efficacy of meniscal repair. Geometry, location, alignment, site, size, and severity, exerts a major impact on the healing potential of the tear [26, 62]. However, the location of meniscal injury varies among the studies included in the present investigation. Eight studies exclusively investigated injuries of the medial meniscus [12, 17, 24, 45, 46, 81, 87, 88], and two, those of the lateral meniscus [23, 82]. Six of the studies that focus on medial injuries specify the location, including only injuries at the posterior root of the medial meniscus [12, 17, 24, 45, 46, 88]. Another eight studies included tears of both medial and lateral meniscus [36, 49, 50, 75, 76, 83, 85, 92]. Two studies did not specify the site of the injury [71, 84]. Injuries of the lateral and medial meniscus have different characteristics in terms of biomechanical function, aetiology, risk factors, and concomitant injuries [48, 72]. Given the lack of quantitative data on the outcomes of interest, it was not possible to analyse injury pattern separately.
The menisci are classically divided into three zones that differ in terms of vascularisation and metabolic activity [4, 5, 19]. Tears at the inner edge show the lowest repair capacity given the avascular nature of the tissue [18]. Initially, tears in the white and red–white zones were thought to be only partially suitable for repair procedure [38]. The described supply zones of the meniscus are considered in seven included studies of the present meta-analysis [36, 49, 71, 75, 76, 81, 87]. Stein et al. [87], Shelbourne et al. [81], and Hoshino et al. [36] reported tears in the red–red and red–white zones, whereas ruptures in the white–white zones underwent partial meniscectomy. The remaining studies do not describe in detail the tear location in relation to the vascular zones [12, 17, 23, 25, 45, 46, 82,83,84,85, 88, 92]. Although removal or partial resection of the meniscus is preferred for tears located in the less vascularised zones, there are increasing reports of successful repairs in the critical zones as well [18, 77]. These results indicate that repair should be attempted in all three zones if at all possible [18, 65].
Depending on the location and type of meniscal tear, inside-out, outside-in, and all-inside techniques are used [68]. The inside-out technique is still considered the gold standard for a variety of tear types [33]. The outside-in technique has become less popular compared to the inside-out technique [63, 93]. Both techniques involve a mini-incision and suturing the meniscus to the capsule [73, 86]. The all-inside technique offers many options, including arthroscopic suture tying and the availability of numerous absorbable fixation devices such as arrows, fastens, darts, and staples [20, 52, 53]. In particular, the ease and associated shorter operating times have led to the great popularity of the all-inside technique [30, 31, 91]. The influence of different repair techniques on clinical outcomes is not conclusive. Stein et al. [87] and Shelbourne et al. [81, 82] used the standard inside-out method. In four studies [49, 50, 83, 88], the outside-in or all-inside technique was used, depending on the location of the tear. Three studies considered all common repair techniques [23, 75, 92]. All studies dealing exclusively with the repair of root tears used the transtibial pull-out method, a modified inside-out technique [12, 17, 24, 45, 46]. No detailed information on the procedure used was found in two of the included studies [36, 84]. Two studies performed open meniscal repair [76, 85]. Open meniscus repair is indicated in selected patients with complex posterior horn tears in combination with an extremely narrow medial compartment to facilitate access [42, 78].
The majority of included studies excluded patients with concurrent knee ligament injury [12, 17, 23, 24, 45, 46, 50, 75, 76, 81, 82, 84, 85, 87]. Person et al. [71] did not exclude ACL injuries, but performed statistical adjustments, when necessary, for age and sex, before evaluating the results. However, meniscal injuries are frequently associated with cruciate ligament injuries, especially tears of the anterior cruciate ligament [55]. When ACL reconstruction is performed concomitantly with the repair of meniscal tears, significantly better healing of meniscal tears is reported [16]. Conversely, meniscal repair leads to increased ACL stability, and ACL reconstruction also benefits from meniscal repair [43]. Therefore, seven of the included studies required ACL injury as an inclusion criterion [36, 49, 81,82,83, 88, 92]. The applicability of the results to knees without ACL damage is uncertain.
Between studies heterogeneity in the resection technique are evident. Only three studies [23, 83, 84] did not define the type of meniscectomy in detail. The other authors [12, 17, 24, 36, 45, 46, 49, 50, 71, 75, 76, 81, 82, 85, 87, 88, 92] conducted a partial meniscectomy [1, 7, 94]. An arthroscopic procedure for partial meniscectomy is used in five studies [50, 71, 75, 76, 87]. Despite the results of the repair and controversies in the current literature, partial resection continues to be indicated in complex, degenerative, avascular tears, or following failure of a previous meniscal repair [52, 59]. Partial meniscectomy is believed to achieve faster recovery and symptoms remission, is simple to perform and requires a short operation time [8, 13, 49].
Additional limitations are evident. Patient age significantly influences the aetiology of meniscus tears, but it is also an important factor regarding the development of OA. Most studies included patients aged 20–30 years [36, 71, 75, 76, 81, 82, 84, 85, 87]. Data from patients aged 40 to 60 years or older are considered in eight studies [12, 17, 24, 45, 46, 49, 88, 92]. Lutz et al. [50] and Shrestha et al. [83] included patients aged 20–40 years. On the other hand, Duethman et al. [23] included patients aged 17 years old. This different age may lead to selection bias. Further, heterogeneity in the outcomes of interest was evident. This can be attributed to the fact that there are no standard criteria to define successful tear healing. Most authors used radiographs for the diagnosis and follow-up [17, 24, 36, 45, 46, 50, 76, 81, 82, 85]. Magnetic resonance imaging was used in four studies [24, 45, 46, 88]. Second-look arthroscopy was performed in two studies [45, 46]. Five studies exclusively referred to PROMs to assess outcomes [71, 75, 83, 84, 92]. Most authors did not specify whether-radiographs of knees were undertaken under weight-bearing condition. Most of the current studies are retrospective [17, 24, 45, 49, 50, 81,82,83, 88, 92]. Level I studies are completely missing, only four have an evidence level of II [36, 71, 75, 81], and 80% (16 of 20) of the included studies achieve level III evidence [12, 17, 23, 24, 45, 46, 49, 50, 76, 82,83,84,85, 87, 88, 92]. Further long-term high-quality studies considering the limitations mentioned above are needed to confirm the advantage of meniscal repair over resection. Moreover, the importance of adequate post-surgery rehabilitation programmes should also be investigated in long-term high-quality larger-scale studies.
Conclusion
Meniscal repair is associated with a lower progression to knee osteoarthritis at approximately six years of follow-up compared to partial meniscectomy. No difference in PROMs, medial joint width, and failures were evidenced.
Data availability
The datasets generated during and/or analysed during the current study are available throughout the manuscript.
References
Abrams GD, Frank RM, Gupta AK, Harris JD, McCormick FM, Cole BJ (2013) Trends in meniscus repair and meniscectomy in the United States, 2005–2011. Am J Sports Med 41:2333–2339
Agarwalla A, Liu JN, Garcia GH, Gowd AK, Puzzitiello RN, Yanke AB et al (2021) Return to sport following isolated lateral opening wedge distal femoral osteotomy. Cartilage 13:846S-852S
Alvarez-Diaz P, Alentorn-Geli E, Llobet F, Granados N, Steinbacher G, Cugat R (2016) Return to play after all-inside meniscal repair in competitive football players: a minimum 5-year follow-up. Knee Surg Sports Traumatol Arthrosc 24:1997–2001
Anderson AF, Irrgang JJ, Dunn W, Beaufils P, Cohen M, Cole BJ et al (2011) Interobserver reliability of the international society of arthroscopy, knee surgery and orthopaedic sports medicine (ISAKOS) classification of meniscal tears. Am J Sports Med 39:926–932
Arnoczky SP, Warren RF (1982) Microvasculature of the human meniscus. Am J Sports Med 10:90–95
Asawatreratanakul P, Boonriong T, Parinyakhup W, Chuaychoosakoon C (2023) Screening for or diagnosing medial meniscal root injury using peripheral medial joint space width ratio in plain radiographs. Sci Rep 13:4982
Bakowski P, Bakowska-Zywicka K, Ciemniewska-Gorzela K, Piontek T (2022) Meniscectomy is still a frequent orthopedic procedure: a pending need for education on the meniscus treatment possibilities. Knee Surg Sports Traumatol Arthrosc 30:1430–1435
Beaufils P, Becker R, Verdonk R, Aagaard H, Karlsson J (2015) Focusing on results after meniscus surgery. Knee Surg Sports Traumatol Arthrosc 23:3–7
Beaufils P, Pujol N (2017) Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res 103:S237–S244
Beaufils P, Seil R, Becker R, Karlsson J, Menetrey J (2021) The orthopaedic community does not oppose the non-surgical treatment of degenerative meniscal lesions. Knee Surg Sports Traumatol Arthrosc 29:329–332
Becker R, Kopf S, Seil R, Hirschmann MT, Beaufils P, Karlsson J (2020) From meniscal resection to meniscal repair: a journey of the last decade. Knee Surg Sports Traumatol Arthrosc 28:3401–3404
Bernard CD, Kennedy NI, Tagliero AJ, Camp CL, Saris DBF, Levy BA et al (2020) Medial meniscus posterior root tear treatment: a matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med 48:128–132
Biedert RM (2000) Treatment of intrasubstance meniscal lesions: a randomized prospective study of four different methods. Knee Surg Sports Traumatol Arthrosc 8:104–108
Bin SI, Jeong TW, Kim SJ, Lee DH (2016) A new arthroscopic classification of degenerative medial meniscus root tear that correlates with meniscus extrusion on magnetic resonance imaging. Knee 23:246–250
Bloch B, Asplin L, Smith N, Thompson P, Spalding T (2019) Higher survivorship following meniscal allograft transplantation in less worn knees justifies earlier referral for symptomatic patients: experience from 240 patients. Knee Surg Sports Traumatol Arthrosc 27:1891–1899
Cannon WD Jr, Vittori JM (1992) The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med 20:176–181
Chung KS, Ha JK, Yeom CH, Ra HJ, Jang HS, Choi SH et al (2015) Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy 31:1941–1950
Cinque ME, DePhillipo NN, Moatshe G, Chahla J, Kennedy MI, Dornan GJ et al (2019) Clinical outcomes of inside-out meniscal repair according to anatomic zone of the meniscal tear. Orthop J Sports Med 7:2325967119860806
Day B, Mackenzie WG, Shim SS, Leung G (1985) The vascular and nerve supply of the human meniscus. Arthroscopy 1:58–62
DeHaven KE (1999) Meniscus repair. Am J Sports Med 27:242–250
Di Matteo B, Moran CJ, Tarabella V, Vigano A, Tomba P, Marcacci M et al (2016) A history of meniscal surgery: from ancient times to the twenty-first century. Knee Surg Sports Traumatol Arthrosc 24:1510–1518
Doral MN, Bilge O, Huri G, Turhan E, Verdonk R (2018) Modern treatment of meniscal tears. EFORT Open Rev 3:260–268
Duethman NC, Wilbur RR, Song BM, Stuart MJ, Levy BA, Camp CL et al (2021) Lateral meniscal tears in young patients: a comparison of meniscectomy and surgical repair. Orthop J Sports Med 9:23259671211046056
Dzidzishvili L, López T II, Arguello JM, Sáez D, Calvo E (2022) Prognostic Factors and midterm clinical outcome of transtibial pullout and partial meniscectomy for medial meniscus posterior root tears in middle-aged patients. Indian J Orthop 56:1457–1463
Dzidzishvili L, Lopez T II, Saez D, Arguello JM, Calvo E (2021) A comparison of the transtibial pullout technique and all-inside meniscal repair in medial meniscus posterior root tear: prognostic factors and midterm clinical outcomes. J Orthop 26:130–134
Englund M, Roos EM, Lohmander LS (2003) Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum 48:2178–2187
Eseonu KC, Neale J, Lyons A, Kluzek S (2022) Are outcomes of acute meniscus root tear repair better than debridement or nonoperative management? A systematic review. Am J Sports Med 50:3130–3139
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Joint Surg Br 30B:664–670
Faucett SC, Geisler BP, Chahla J, Krych AJ, Kurzweil PR, Garner AM et al (2019) Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med 47:762–769
Fillingham YA, Riboh JC, Erickson BJ, Bach BR Jr, Yanke AB (2017) Inside-out versus all-inside repair of isolated meniscal tears: an updated systematic review. Am J Sports Med 45:234–242
Grant JA, Wilde J, Miller BS, Bedi A (2012) Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med 40:459–468
Greis PE, Bardana DD, Holmstrom MC, Burks RT (2002) Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg 10:168–176
Henning CE, Clark JR, Lynch MA, Stallbaumer R, Yearout KM, Vequist SW (1988) Arthroscopic meniscus repair with a posterior incision. Instr Course Lect 37:209–221
Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2021) Cochrane handbook for systematic reviews of interventions version 6.2. Cochrane. Available from www.training.cochrane.org/handbook. Accessed Feb 2022
Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R et al (2007) Reliability and validity of the international knee documentation committee (IKDC) subjective knee form. Joint Bone Spine 74:594–599
Hoshino T, Nakagawa Y, Inomata K, Ohara T, Katagiri H, Otabe K et al (2022) Effects of different surgical procedures for meniscus injury on two-year clinical and radiological outcomes after anterior cruciate ligament reconstructions. -TMDU MAKS study. J Orthop Sci 27:199–206
Howick J CI, Glasziou P, Greenhalgh T, Carl Heneghan, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford CEBM levels of evidence. Oxford centre for evidence-based medicine. Available at https://www.cebm.net/index.aspx?o=5653. Accessed Jan 2020
Hutchinson ID, Moran CJ, Potter HG, Warren RF, Rodeo SA (2014) Restoration of the meniscus: form and function. Am J Sports Med 42:987–998
Johnson A, Huang YC, Mao CF, Chen CK, Thomas S, Kuo HP et al (2022) Protective effect of ethanolic extract of Echinacea purpurea contained nanoparticles on meniscal/ligamentous injury induced osteoarthritis in obese male rats. Sci Rep 12:5354
Jones KJ, Kelley BV, Arshi A, McAllister DR, Fabricant PD (2019) Comparative effectiveness of cartilage repair with respect to the minimal clinically important difference. Am J Sports Med 47:3284–3293
Kaiser JT, Meeker ZD, Horner NS, Sivasundaram L, Wagner KR, Mazra AF et al (2022) Meniscal ramp lesions-Skillful neglect or routine repair? J Orthop 32:31–35
Karia M, Ghaly Y, Al-Hadithy N, Mordecai S, Gupte C (2019) Current concepts in the techniques, indications and outcomes of meniscal repairs. Eur J Orthop Surg Traumatol 29:509–520
Katakura M, Horie M, Watanabe T, Katagiri H, Otabe K, Ohara T et al (2019) Effect of meniscus repair on pivot-shift during anterior cruciate ligament reconstruction: objective evaluation using triaxial accelerometer. Knee 26:124–131
Keyhani S, Movahedinia M, LaPrade RF, Qoreishy M, Vosoughi F (2023) Long-term clinical results of using a posteromedial all-inside and anteromedial inside-out approach to repair unstable or irreducible bucket-handle medial meniscal tears. J Orthop Traumatol 24:12
Kim CW, Lee CR, Gwak HC, Kim JH, Park DH, Kwon YU et al (2019) Clinical and radiologic outcomes of patients with lax healing after medial meniscal root repair: comparison with subtotal meniscectomy. Arthroscopy 35:3079–3086
Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG et al (2011) Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy 27:346–354
Korthaus A, Ballhause TM, Kolb JP, Krause M, Frosch KH, Hartel MJ (2020) Extended approach to the lateral tibial plateau with central meniscal subluxation in fracture repair: feasibility and first clinical and radiographic results. Eur J Trauma Emerg Surg 46:1221–1226
Krych AJ, Bernard CD, Kennedy NI, Tagliero AJ, Camp CL, Levy BA et al (2020) Medial versus lateral meniscus root tears: is there a difference in injury presentation, treatment decisions, and surgical repair outcomes? Arthroscopy 36:1135–1141
Lee WQ, Gan JZ, Lie DTT (2019) Save the meniscus-clinical outcomes of meniscectomy versus meniscal repair. J Orthop Surg (Hong Kong) 27:2309499019849813
Lutz C, Dalmay F, Ehkirch FP, Cucurulo T, Laporte C, Le Henaff G et al (2015) Meniscectomy versus meniscal repair: 10 years radiological and clinical results in vertical lesions in stable knee. Orthop Traumatol Surg Res 101:S327-331
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154
Maffulli N, Longo UG, Campi S, Denaro V (2010) Meniscal tears. Open Access J Sports Med 1:45–54
McCarty EC, Marx RG, DeHaven KE (2002) Meniscus repair: considerations in treatment and update of clinical results. Clin Orthop Relat Res 402:122–134
McDermott ID, Amis AA (2006) The consequences of meniscectomy. J Bone Joint Surg Br 88:1549–1556
Mehl J, Otto A, Baldino JB, Achtnich A, Akoto R, Imhoff AB et al (2019) The ACL-deficient knee and the prevalence of meniscus and cartilage lesions: a systematic review and meta-analysis (CRD42017076897). Arch Orthop Trauma Surg 139:819–841
Migliorini F, Asparago G, Oliva F, Bell A, Hildebrand F, Maffulli N (2023) Greater rate of return to play and re-injury following all-inside meniscal repair compared to the inside-out technique: a systematic review. Arch Orthop Trauma Surg 143:6273–6282
Migliorini F, Cuozzo F, Cipollaro L, Oliva F, Hildebrand F, Maffulli N (2022) Platelet-rich plasma (PRP) augmentation does not result in more favourable outcomes in arthroscopic meniscal repair: a meta-analysis. J Orthop Traumatol 23:8
Migliorini F, Oliva F, Eschweiler J, Cuozzo F, Hildebrand F, Maffulli N (2023) No evidence in support of arthroscopic partial meniscectomy in adults with degenerative and nonobstructive meniscal symptoms: a level I evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc 31:1733–1743
Migliorini F, Oliva F, Eschweiler J, Cuozzo F, Hildebrand F, Maffulli N (2022) No evidence in support of arthroscopic partial meniscectomy in adults with degenerative and nonobstructive meniscal symptoms: a level I evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07040-0
Migliorini F, Pilone M, Bell A, Celik M, Konrads C, Maffulli N (2023) Outside-in repair technique is effective in traumatic tears of the meniscus in active adults: a systematic review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-023-07475-z
Migliorini F, Vecchio G, Giorgino R, Eschweiler J, Hildebrand F, Maffulli N (2023) Micro RNA in meniscal ailments: current concepts. Br Med Bull 145:141–150
Mordecai SC, Al-Hadithy N, Ware HE, Gupte CM (2014) Treatment of meniscal tears: an evidence based approach. World J Orthop 5:233–241
Morgan CD, Casscells SW (1986) Arthroscopic meniscus repair: a safe approach to the posterior horns. Arthroscopy 2:3–12
Mostafaee N, Negahban H, Shaterzadeh Yazdi MJ, Goharpey S, Mehravar M, Pirayeh N (2020) Responsiveness of a persian version of knee injury and osteoarthritis outcome score and tegner activity scale in athletes with anterior cruciate ligament reconstruction following physiotherapy treatment. Physiother Theory Pract 36:1019–1026
Nepple JJ, Dunn WR, Wright RW (2012) Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am 94:2222–2227
Nesbitt DQ, Burruel DE, Henderson BS, Lujan TJ (2023) Finite element modeling of meniscal tears using continuum damage mechanics and digital image correlation. Sci Rep 13:4039
Nguyen JC, De Smet AA, Graf BK, Rosas HG (2014) MR imaging-based diagnosis and classification of meniscal tears. Radiographics 34:981–999
Ozeki N, Seil R, Krych AJ, Koga H (2021) Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS 6:35–45
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Paxton ES, Stock MV, Brophy RH (2011) Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy 27:1275–1288
Persson F, Turkiewicz A, Bergkvist D, Neuman P, Englund M (2018) The risk of symptomatic knee osteoarthritis after arthroscopic meniscus repair vs partial meniscectomy vs the general population. Osteoarthritis Cartilage 26:195–201
Petersen W, Forkel P, Feucht MJ, Zantop T, Imhoff AB, Brucker PU (2014) Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg 134:237–255
Petersen W, Zantop T (2006) Arthroscopic meniscal suture. Oper Orthop Traumatol 18:393–410
Petersson IF, Boegard T, Saxne T, Silman AJ, Svensson B (1997) Radiographic osteoarthritis of the knee classified by the Ahlback and Kellgren and Lawrence systems for the tibiofemoral joint in people aged 35–54 years with chronic knee pain. Ann Rheum Dis 56:493–496
Pihl K, Englund M, Christensen R, Lohmander LS, Jorgensen U, Viberg B et al (2021) Less improvement following meniscal repair compared with arthroscopic partial meniscectomy: a prospective cohort study of patient-reported outcomes in 150 young adults at 1- and 5-years’ follow-up. Acta Orthop 92:589–596
Rockborn P, Messner K (2000) Long-term results of meniscus repair and meniscectomy: a 13-year functional and radiographic follow-up study. Knee Surg Sports Traumatol Arthrosc 8:2–10
Rubman MH, Noyes FR, Barber-Westin SD (1998) Arthroscopic repair of meniscal tears that extend into the avascular zone. A review of 198 single and complex tears. Am J Sports Med 26:87–95
Rupp S, Seil R, Kohn D (2001) Ergebnisse nach Meniskusnaht. Arthroskopie 14:267–275
Saengpetch N, Noowan S, Boonrod A, Jaruwanneechai K, Sumanont S, Vijittrakarnrung C (2023) Comparison of medial tibiofemoral joint mechanics between all-suture anchors and transtibial pullout technique for posterior medial meniscal root tears. J Orthop Surg Res 18:591
Salata MJ, Gibbs AE, Sekiya JK (2010) A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med 38:1907–1916
Shelbourne KD, Carr DR (2003) Meniscal repair compared with meniscectomy for bucket-handle medial meniscal tears in anterior cruciate ligament-reconstructed knees. Am J Sports Med 31:718–723
Shelbourne KD, Dersam MD (2004) Comparison of partial meniscectomy versus meniscus repair for bucket-handle lateral meniscus tears in anterior cruciate ligament reconstructed knees. Arthroscopy 20:581–585
Shrestha R, Khadka SK, Basi A, Malla M, Thapa S, Tripathi A et al (2022) Meniscal tear at knee: repair or resect? An early experience from a university hospital in Nepal. Kathmandu Univ Med J (KUMJ) 20:47–50
Sochacki KR, Varshneya K, Calcei JG, Safran MR, Abrams GD, Donahue J et al (2020) Comparing meniscectomy and meniscal repair: a matched cohort analysis utilizing a national insurance database. Am J Sports Med 48:2353–2359
Sommerlath KG (1991) Results of meniscal repair and partial meniscectomy in stable knees. Int Orthop 15:347–350
Starke C, Kopf S, Petersen W, Becker R (2009) Meniscal repair. Arthroscopy 25:1033–1044
Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jager A (2010) Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med 38:1542–1548
Su J, Wan H, Pang Y, Lu Y, Liang J, Yan Z et al (2022) Trans-posterior cruciate ligament all-inside root repair versus partial meniscectomy for medial meniscus posterior root tears: comparison of semiquantitative and quantitative mri outcomes in cartilage degeneration and osteoarthritic progression. Cartilage 13:19476035221114240
Thorlund JB, Juhl CB, Roos EM, Lohmander LS (2015) Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. Br J Sports Med 49:1229–1235
Tsutsumi M, Nimura A, Tharnmanularp S, Kudo S, Akita K (2023) Posteromedial capsular anatomy of the tibia for consideration of the medial meniscal support structure using a multidimensional analysis. Sci Rep 13:12030
Turman KA, Diduch DR, Miller MD (2009) All-inside meniscal repair. Sports Health 1:438–444
Ventura M, Seabra P, Oliveira J, Sousa P, Quesado M, Sousa H et al (2023) Meniscal injuries in patients aged 40 years or older: a comparative study between meniscal repair and partial meniscectomy. Cureus 15:e33270
Warren RF, Levy IM (1983) Meniscal lesions associated with anterior cruciate ligament injury. Clin Orthop Relat Res 172:32–37
Wasserburger JN, Shultz CL, Hankins DA, Korcek L, Martin DF, Amendola A et al (2021) Long-term national trends of arthroscopic meniscal repair and debridement. Am J Sports Med 49:1530–1537
Xu C, Zhao J (2015) A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc 23:164–170
Zhang Z, Shang XK, Mao BN, Li J, Chen G (2019) Torn discoid lateral meniscus is associated with increased medial meniscal extrusion and worse articular cartilage status in older patients. Knee Surg Sports Traumatol Arthrosc 27:2624–2631
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
FM was involved in literature search, data extraction, risk of bias assessment, conception and design, drafting, and final approval; NM performed supervision, revision, and final approval; CRW was responsible for writing, and final approval; LS did literature search, data extraction, risk of bias assessment, and final approval; AB performed supervision, and final approval; GV was involved in drafting, and final approval. All the authors have agreed to the final version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have any competing interests for this article.
Ethical approval
This study complies with ethical standards.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Registration and protocol
The present review was not registered.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Migliorini, F., Schäfer, L., Bell, A. et al. Meniscectomy is associated with a higher rate of osteoarthritis compared to meniscal repair following acute tears: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 31, 5485–5495 (2023). https://doi.org/10.1007/s00167-023-07600-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07600-y