Abstract
Purpose
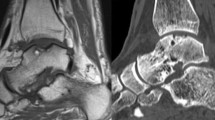
The purpose of this study was to retrospectively evaluate the clinical, arthroscopic and radiological outcomes of autologous osteoperiosteal transplantation for massive cystic osteochondral defects of the talus.
Methods
Cases of autologous osteoperiosteal transplantation for medial massive cystic defects of the talus between 2014 and 2018 were reviewed. The visual analogue scale (VAS), American Orthopaedic Foot and Ankle Society (AOFAS) score, Foot and Ankle Outcome Score (FAOS), and Ankle Activity Scale (AAS) were assessed preoperatively and postoperatively. The Magnetic Resonance Observation of Cartilage Tissue (MOCART) system and the International Cartilage Repair Society (ICRS) score were evaluated after surgery. The ability to return to daily activity and sport, as well as complications, were recorded.
Results
Twenty-one patients were available for follow-up, with a mean follow-up of 60.1 ± 11.7 months. All subscales of preoperative FAOS had significant (P < 0.001) improvement at the final follow-up. The mean AOFAS and VAS scores significantly (P < 0.001) improved from 52.4 ± 12.4 preoperatively to 90.9 ± 5.2 at the last follow-up and from 7.9 ± 0.8 to 1.5 ± 0.9, respectively. The mean AAS decreased from 6.0 ± 1.4 preinjury to 1.4 ± 0.9 postinjury and then increased to 4.6 ± 1.4 at the final follow-up (P < 0.001). All 21 patients resumed daily activities after a mean of 3.1 ± 1.0 months. Fifteen patients (71.4%) returned to sports after a mean of 12.9 ± 4.1 months. All patients underwent follow-up MRI with a mean MOCART score of 68.6 ± 5.9. Eleven patients underwent second-look arthroscopy, and the average ICRS was 9.4 ± 0.8. No donor site morbidity was found in any patient during the follow-up.
Conclusion
Autologous osteoperiosteal transplantation provided favourable clinical, arthroscopic and radiographic outcomes in patients with massive cystic osteochondral defects of the talus during a minimum 3-year follow-up.
Level of evidence
IV.

Similar content being viewed by others
Data availability
The data are available on request.
Abbreviations
- VAS:
-
Visual analogue scale
- AOFAS:
-
American orthopaedic foot and ankle society score
- FAOS:
-
Foot and ankle outcome score
- AAS:
-
Ankle activity scale
- MOCART:
-
Magnetic resonance observation of the cartilage tissue system
- ICRS:
-
International cartilage repair society score
- OLTs:
-
Osteochondral lesions of the talus
- AOT:
-
Autologous osteochondral transplantation
- BMI:
-
Body mass index
- PACS:
-
Picture archiving and communication system
- ROM:
-
Range of motion
References
Ahmad J, Jones K (2016) Comparison of osteochondral autografts and allografts for treatment of recurrent or large talar osteochondral lesions. Foot Ankle Int 37:40–50
Bai L, Guan S, Liu S, You T, Xie X, Chen P et al (2020) Clinical outcomes of osteochondral lesions of the talus with large subchondral cysts treated with osteotomy and autologous chondral grafts: minimum 2-year follow-up and second-look evaluation. Orthop J Sports Med 8:2325967120937798
Becher C, Malahias MA, Ali MM, Maffulli N, Thermann H (2019) Arthroscopic microfracture vs. arthroscopic autologous matrix-induced chondrogenesis for the treatment of articular cartilage defects of the talus. Knee Surg Sports Traumatol Arthrosc 27:2731–2736
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A(Suppl 2):58–69
Bruns J, Habermann C, Werner M (2021) Osteochondral lesions of the talus: a review on talus osteochondral injuries Including Osteochondritis Dissecans. Cartilage 13:1947603520985182
Carlsson AM (1983) Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 16:87–101
Chen W, Tang K, Yuan C, Zhou Y, Tao X (2015) Intermediate results of large cystic medial osteochondral lesions of the talus treated with osteoperiosteal cylinder autografts from the medial tibia. Arthroscopy 31:1557–1564
Chu C-H, Chen I-H, Yang K-C, Wang C-C (2021) Midterm Results of fresh-frozen osteochondral allografting for osteochondral lesions of the talus. Foot Ankle Int 42:8–16
Debnath S, Yallowitz AR, McCormick J, Lalani S, Zhang T, Xu R et al (2018) Discovery of a periosteal stem cell mediating intramembranous bone formation. Nature 562:133–139
Deng E, Gao L, Shi W, Xie X, Jiang Y, Yuan H et al (2020) Both magnetic resonance imaging and computed tomography are reliable and valid in evaluating cystic osteochondral lesions of the talus. Orthop J Sports Med 8:2325967120946697
El-Rashidy H, Villacis D, Omar I, Kelikian AS (2011) Fresh osteochondral allograft for the treatment of cartilage defects of the talus: a retrospective review. J Bone Joint Surg Am 93:1634–1640
Gross AE, Agnidis Z, Hutchison CR (2001) Osteochondral defects of the talus treated with fresh osteochondral allograft transplantation. Foot Ankle Int 22:385–391
Halasi T, Kynsburg A, Tállay A, Berkes I (2004) Development of a new activity score for the evaluation of ankle instability. Am J Sports Med 32:899–908
Hu Y, Guo Q, Jiao C, Mei Y, Jiang D, Wang J et al (2013) Treatment of large cystic medial osteochondral lesions of the talus with autologous osteoperiosteal cylinder grafts. Arthroscopy 29:1372–1379
Kadakia AR, Espinosa N (2013) Why allograft reconstruction for osteochondral lesion of the talus? The osteochondral autograft transfer system seemed to work quite well. Foot Ankle Clin 18:89–112
Kerkhoffs GMMJ, Altink JN, Stufkens SAS, Dahmen J (2021) Talar OsteoPeriostic grafting from the Iliac Crest (TOPIC) for large medial talar osteochondral defects: Operative technique (Talar OsteoPeriostic grafting from the Iliac Crest (TOPIC) for large medial talar osteochondral defects: operative technique). Oper Orthop Traumatol 33:160–169
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349–353
Looze CA, Capo J, Ryan MK, Begly JP, Chapman C, Swanson D et al (2017) Evaluation and management of osteochondral lesions of the talus. Cartilage 8:19–30
Marlovits S, Singer P, Zeller P, Mandl I, Haller J, Trattnig S (2006) Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol 57:16–23
McCollum GA, Myerson MS, Jonck J (2013) Managing the cystic osteochondral defect: allograft or autograft. Foot Ankle Clin 18:113–133
Mercer NP, Samsonov AP, Dankert JF, Kennedy JG (2022) Outcomes of autologous osteochondral transplantation with and without extracellular matrix cartilage allograft augmentation for osteochondral lesions of the talus. Am J Sports Med 50:162–169
Raikin SM (2004) Stage VI: massive osteochondral defects of the talus. Foot Ankle Clin 9:737–744
Raikin SM (2009) Fresh osteochondral allografts for large-volume cystic osteochondral defects of the talus. J Bone Joint Surg Am 91:2818–2826
Rikken QGH, Dahmen J, Reilingh ML, van Bergen CJA, Stufkens SAS, Kerkhoffs GMMJ (2021) Outcomes of bone marrow stimulation for secondary osteochondral lesions of the talus equal outcomes for primary lesions. Cartilage 13:1429S-1437S
Rikken QG, Kerkhoffs GM (2021) Osteochondral lesions of the talus. Foot Ankle Clin 26:121–136
Roos EM, Brandsson S, Karlsson J (2001) Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int 22:788–794
Shi W, Yang S, Xiong S, Xu M, Pi Y, Chen L et al (2022) Comparison of autologous osteoperiosteal and osteochondral transplantation for the treatment of large, medial cystic osteochondral lesions of the talus. Am J Sports Med 50:769–777
Shim DW, Park KH, Lee JW, Yang Y-J, Shin J, Han SH (2021) Primary autologous osteochondral transfer shows superior long-term outcome and survival rate compared with bone marrow stimulation for large cystic osteochondral lesion of talus. Arthroscopy 37:989–997
Shimozono Y, Hurley ET, Nguyen JT, Deyer TW, Kennedy JG (2018) Allograft compared with autograft in osteochondral transplantation for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am 100:1838–1844
Shimozono Y, Hurley ET, Myerson CL, Kennedy JG (2018) Good clinical and functional outcomes at mid-term following autologous osteochondral transplantation for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc 26:3055–3062
Slabaugh MA (2019) CORR insights®: knee-to-talus donor-site morbidity following autologous osteochondral transplantation: a meta-analysis with best-case and worst-case analysis. Clin Orthop Relat Res 477:1932–1933
Smith GD, Taylor J, Almqvist KF, Erggelet C, Knutsen G, Garcia Portabella M et al (2005) Arthroscopic assessment of cartilage repair: a validation study of 2 scoring systems. Arthroscopy 21:1462–1467
Sung MS, Jeong CH, Lim YS, Yoo WJ, Chung SK, Jung NY (2011) Periosteal autograft for articular cartilage defects in dogs: MR imaging and ultrasonography of the repair process. Acta Radiol 52:181–190
Weigelt L, Hartmann R, Pfirrmann C, Espinosa N, Wirth SH (2019) Autologous matrix-induced chondrogenesis for osteochondral lesions of the talus: a clinical and radiological 2- to 8-year follow-up study. Am J Sports Med 47:1679–1686
Winkler PW, Geyer S, Walzl D, Woertler K, Paul J, Siebenlist S et al (2022) Favorable long-term clinical and radiologic outcomes with high survivorship after autologous osteochondral transplantation of the talus. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07237-3
Acknowledgements
The authors would like to thank Wenqiang Yan and Fengyi Hu for writing assistance and language help with the manuscript.
Funding
This work was supported by grants from Beijing Municipal Science & Technology Commission (No. Z161100000116072), Beijing Nova Program (No. Z201100006820011) from the Beijing Municipal Science & Technology Commission and the National Natural Science Foundation of China (No. 81902208).
Author information
Authors and Affiliations
Contributions
SY and LJ both contributed to the literature search, data collection and analysis, statistics analysis and manuscript preparation. LC, YP, DJ, CJ and YH contributed to the surgical data provision and manuscript editing. FZ and XX contributed to the conceptualization and manuscript review. WS contributed to the data collection and analysis, literature search and manuscript review. QG contributed to the substantial conceptualization, surgical data provision, supervision and final approval of the draft version. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Board of Research Ethics of Peking University Third Hospital Medical Science Research Ethics Committee (IRB00006761-M2021296).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, S., Jing, L., Chen, L. et al. Favourable clinical, arthroscopic and radiographic outcomes after autologous osteoperiosteal transplantation for massive medial cystic osteochondral defects of the talus. Knee Surg Sports Traumatol Arthrosc 31, 3509–3516 (2023). https://doi.org/10.1007/s00167-023-07397-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07397-w