Abstract
Purpose
It is well-known that revision rates after primary knee arthroplasty vary widely. However, it is uncertain whether hospital revision rates are reliable indicators of general surgical quality as defined by patients. The SPARK study compared primary knee arthroplasty surgery at three high-volume hospitals whose revision rates differed for unknown reasons.
Methods
This prospective observational study included primary knee arthroplasty patients (total, medial/lateral unicompartmental and patellofemoral) in two low-revision hospitals (Aarhus University Hospital and Aalborg University Hospital Farsø) and one high-revision hospital (Copenhagen University Hospital Herlev-Gentofte). Patients were followed from preoperatively (2016–17) to 1-year postoperatively with patient-reported outcome measures including Oxford Knee Score (OKS), EQ-5D-5L and Copenhagen Knee ROM (range of motion) Scale. The surgical outcomes were compared across hospitals for patients with comparable grades of radiographic knee osteoarthritis and preoperative OKS. Statistical comparisons (parametric and non-parametric) included all three hospitals.
Results
97% of the 1452 patients who provided baseline data (89% of those included and 56% of those operated) responded postoperatively (90% at 1 year). Hospitals’ utilization of unicompartmental knee arthroplasties differed (Aarhus 49%, Aalborg 14%, and Copenhagen 22%, p < 0.001). 28 patients had revision surgery during the first year (hospital independent, p = 0.1) and were subsequently excluded. 1-year OKS (39 ± 7) was independent of hospital (p = 0.1), even when adjusted for age, sex, Body Mass Index, baseline OKS and osteoarthritis grading. 15% of patients improved less than Minimal Important Change (8 OKS) (Aarhus 19%, Aalborg 13% and Copenhagen 14%, p = 0.051 unadjusted). Patients with comparable preoperative OKS or osteoarthritis grading had similar 1-year results across hospitals (OKS and willingness to repeat surgery, p ≥ 0.087) except for the 64 patients with Kellgren–Lawrence grade-4 (Aarhus 4–6 OKS points lower). 86% of patients were satisfied, and 92% were “willing to repeat surgery”, independent of hospital (p ≥ 0.1). Hospital revision rates differences diminished during the study period.
Conclusions
Patients in hospitals with a history of differing revision rates had comparable patient-reported outcomes 1 year after primary knee arthroplasty, supporting that surgical quality should not be evaluated by revision rates alone. Future studies should explore if revision rate variations may depend as much on revision thresholds and indications as on outcomes of primary surgery.
Level of evidence
Level II (Prospective cohort study).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When hospitals differ in cumulative revision rates (CRR) following primary knee arthroplasty (KA), it leads to assumptions of differences in the quality of surgery. This is the case for variation both among and within countries [22]. However, with pain relief and regaining knee function being the primary goals of KA surgery, CRRs may not be the most important measure of treatment quality in the vast majority of patients, i.e., those, who are never revised and whose spectrum of postoperative results are not reflected in the statistics [8]. In 2015, Danish KA surgeons recognized the need for a comprehensive comparison of the primary KA surgery performed in the three (of five) administrative regions with the greatest differences in 1-, 2-, 5- and 10-year CRRs. The goal was to determine whether CRR variations were a reflection of overall differences in the quality of primary KA surgery, defined as patients’ subjective improvement after surgery [26]. By posing this question, the focus was shifted from registry-based quality to quality based on patient assessment, patient-reported outcome measures (PROMs) and range of motion.
Each region was represented by its largest KA hospital in a prospective observational cohort study, SPARK (“Variation in patient Satisfaction, Patient-reported outcome measures, radiographic signs of Arthritis, and Revision rates in Knee arthroplasty patients in three Danish regions”). The baseline publication [16] from the SPARK study compared the three hospitals’ patient selection at primary surgery by analyzing preoperative data from 1452 patients who underwent primary KA in routine clinical settings. It was reported that patient demographics, anxiety and depression symptoms, KA incidence, implant selection and radiographic classification of knee osteoarthritis varied somewhat between hospitals, but preoperative PROMs did not. The majority of hospital differences at baseline were in opposition to well-known revision risk factors. For example, one low-revision hospital (Aarhus) used more unicompartmental implants (49%) than the others [Aalborg 14% (low-CRR) and Copenhagen 22% (high-CRR)] (Table 1). Overall, the study was unable to identify differences in baseline characteristics that could adequately explain the persistent hospital differences in CRRs [16]. The present follow-up study compares the postoperative outcomes of primary KA in the SPARK cohort and determines if patients with a certain level of symptoms or radiological knee osteoarthritis (OA) can expect similar outcomes at the three hospitals.
Aside from differences in CRR between regions (e.g., 1.0, 2.2 and 5% per 2 years in 2015) and undocumented claims of cultural differences between east (Capital, high-revision) and west (low-revision), no previous data had led to hypotheses of quality differences across the country. Therefore, all data were analyzed under the assumption (null hypothesis) that there was no difference in hospital outcomes.
Materials and methods
The study was ethically approved by The National Committee of Health Research Ethics (Protocol no. 16038343, 2 September 2016). All patients provided written consent to participate in the study. The study was reported in accordance with the STROBE guidelines (STrengthening the Reporting of OBservational studies in Epidemiology). Register data were retrieved from the Danish Knee Arthroplasty Register and the Danish National Patient Register [24].
Patient inclusion
The prospective observational cohort study, SPARK, was conducted in three high-volume hospitals with 2-year CRRs that were representative of their region during the preceding 3 years: Aarhus University Hospital (1.9%) in Central Denmark Region (2.5%), Aalborg University Hospital Farsø (1.6%) in North Denmark Region (1.5%) and Copenhagen University Hospital Herlev-Gentofte (5.6%) in the Capital Region (4.7%) [16]. From 1 Sep 2016 to 31 Dec 2017, surgeons and employed medical students invited patients scheduled for KA (total (TKA), medial or lateral unicompartmental (MUKA/LUKA), or patellofemoral (PFA) knee arthroplasty) to participate in the study. Knee tumors, severe developmental lower limb deformities, haemophilia, dementia and severe language barriers were exclusion criteria, and this follow-up study only enrolled the 1452 patients who had provided PROM-data before surgery [16]. Questionnaires were sent by emails with unique links before surgery and 6 weeks, and 3, 6 and 12 months postoperatively. Patients who could only respond via traditional mail were only allowed inclusion in the final 6 months of the inclusion period. Some patients participated with both knees at separate occasions, and many more had bilateral knee trouble, thus the emails specifically addressed “right” or “left knee” and current follow-up time. If necessary, two reminders were sent, and at 1 year, a printed questionnaire with a postage-paid envelope was sent to non-responders. Surgeons continuously delivered surgical information as part of their routines and any missing or erroneous information was meticulously corrected using medical records.
Participants who underwent revision during the first year were not the main focus of the study. However, their PROMs were collected and reported until the day of revision. For example, a patient who was revised after 8 months could contribute to PROM analyses at 6 months, but not at 1 year. All subsequent revisions were attributed to the primary KA hospital regardless of which hospital (public or private) performed the revision. Minor surgery, such as wound debridement or manipulation under anesthesia did not result in participation cessation.
Radiographic classification of knee osteoarthritis
Blinded posteroanterior weight-bearing radiographs were used to evaluate the radiographic severity of knee osteoarthritis [23]. To facilitate fair comparisons, LUKA and PFA patients and radiographs with predominantly lateral joint space narrowing were excluded. Two radiologists graded knee OA according to Kellgren–Lawrence (K–L) classification (0–4, 4 most severe) and Ahlbäck score (0–5, 5 most severe) [16, 1, 12]. Moreover, 13 experienced KA surgeons performed thousands of “head-to-head” comparisons of the radiographs based on heuristics, i.e., “rules of thumb” and clinical experience and without the use of traditional classification systems, resulting in a complete OA severity ranking of all radiographs (further details in preceding publications [16, 18]).
Patient-reported outcome measures (PROMs)
The primary outcome, Oxford Knee Score (OKS, 0–48, 48 best), was reported as absolute score, change from baseline, and as proportions of patients achieving the Minimal Important Change (MIC) of 8 points indicating an important improvement for the average patient at 1 year [2, 6, 10, 11, 17, 25]. Copenhagen Knee ROM Scale (CKRS) assessed patient-reported passive range of motion (ROM), i.e., flexion (0–6, 6 max) and extension (0–5, 5 max) as well as estimated proportions of patients with flexion or extension deficits [14]. Every PROM set began with the generic EQ-5D-5L and EQ-VAS and a “global knee anchor” question asking, “How is your knee?” (VAS, 0–100, 100 best), and patients reported how often they used any type of analgesics for knee pain [30].
Additional questions and PROMs were added at varying time points. At baseline, height, weight, smoking, alcohol and level of urbanization data were reported [13, 29]. The Forgotten Joint Score (FJS) [3] and UCLA Activity Scale (UCLA) [15] were added from 3 months postoperatively, and UCLA was also used at baseline. At 6 months, patients answered whether they had received physiotherapeutic assistance in rehabilitation after hospital discharge. From 3 months on, patient satisfaction was measured by asking, “How satisfied are you with the overall experience of the operation and its result?” (five Likert boxes, one neutral). As the answers could be influenced by experiences related to hospital service, kindness of caretakers, etc. [5], also “willingness to repeat surgery” was reported at 1 year: “Suppose you could turn back time, would you still choose to have a knee replacement now that you know the outcome?” (five Likert boxes, one neutral).
Implants, perioperative care, and follow-up routines
The SPARK study did not interfere with local hospital routines concerning, e.g., analgesics use, aftercare, or selection of KA implants. Each hospital used a unique selection of cemented, uncemented and hybrid implants that were on the market for at least 10 years and had proven good survival in registries [24]. The predominant systems were NexGen™ (Zimmer Biomet), PFC™ Sigma (DePuy Synthes), Triathlon™ (Stryker), Oxford™ Mobile Bearing and ZUK™ (Zimmer Biomet) and Avon™ (Stryker).
In all three hospitals, tranexamic acid, glucocorticoids, local anesthetics and prophylactic antibiotics (dicloxacillin in Copenhagen, cefuroxime in Aarhus and Aalborg) were administered intraoperatively. Paracetamol, non-steroid anti-inflammatory drugs (NSAID) and opioids were the oral analgesics of choice for up to 4 weeks postoperatively. In 2017, the average length of stay for TKA patients in Aarhus, Aalborg and Copenhagen was 2.4, 1.4 and 2.2 nights, respectively, and for MUKA patients it was 0.6, 1.3 and 0.7 nights [27].
The routine preoperative multidisciplinary patient seminar included preparation training with physiotherapists (crutch walking, stair climbing, etc.). Postoperatively, Aalborg and Copenhagen patients were trained by a physiotherapist, and Copenhagen patients were routinely offered free of charge supervised physiotherapy upon discharge. Aarhus and Aalborg patients were screened 2–6 weeks after discharge to identify those in need of physiotherapy and only those whose progress was unsatisfactory after 6–8 weeks or who had abnormal findings on 1-year radiographs were referred to the surgeon for a follow-up appointment. In contrast, all Copenhagen patients saw their surgeon and had radiographs taken after 3 months.
Statistics
Based on pragmatic considerations and feasibility, the study aimed for a sample size of 1080 patients (75% inclusion rate and 80% response rate among 1800 patients) [16]. All significance tests comprised all three hospitals unless otherwise specified. In regression analyses, Aarhus was selected as the reference hospital, because it was situated between the other two hospitals in terms of geography, urbanization level, and revision rates. All observations were treated as independent data [21]. P values were two-sided with alpha level 0.05. Standard deviations were displayed as “(± SD)”. Tabular data were analyzed by Chi-square test (with Monte-Carlo correction for expected cell counts < 5), and Clopper–Pearson confidence intervals (95% CI) were provided when relevant. Non-parametric (ranked) methods (Kruskal–Wallis or Wilcoxon/Mann–Whitney U test) were used for ordinal measures (UCLA, global knee anchor, patient satisfaction, willingness to repeat, use of analgesics and radiographic classifications, while parametric methods (one-way analysis of variance (ANOVA) or t test) were applied to OKS, FJS, EQ-5D and CKRS [17]. Multiple linear regression analyses (dependent variable OKS) were conducted with both Ahlbäck and K–L, but since the overall result was not changed with classification method, only Ahlbäck-based confidence intervals (CIs) were reported. Since 1-year change scores for revised patients were unavailable, the analysis of change in OKS was repeated using imputed results (clearly specified). Analyses were carried out in R (RStudio) in Mar 2019 [20]. Data collection and Case Report Forms (CRF) were handled by Procordo Software Aps, Copenhagen.
Results
Patient inclusion
Baseline data were available for 1452 patients (68.0 ± 9 years, 45% males, 89% response rate) (Table 1). The 41 patients who participated by mail were 8 years older and more likely to be female (71%) than those who participated online. According to the post-hoc inclusion analysis, 56% of patients (62% in Aarhus and Copenhagen, 38% in Aalborg) provided baseline data for the SPARK study in 2017 [16]. Participants were younger than non-participants (67.7 ± 9 vs. 68.8 ± 11 years, p = 0.02) and more likely to be male (42 vs. 38%, p = 0.016). Implant types were equally distributed among participants and non-participants within each hospital (p ≥ 0.2) [16].
1414 patients (97%) responded postoperatively at least once, and 1307 (90%) responded at 1 year (Table 2). The response rate was comparable among hospitals (p = 0.4). In the first year, three patients left the study, seven died, and nine were lost to follow up due to errors, such as incorrect laterality or change of email address. Revision surgery was performed on 28 patients (1.9%) during the first postoperative year; 2 (0.6%) in Aarhus, 4 (2.0%) in Aalborg and 22 (2.4%) in Copenhagen (p = 0.1). Last available postoperative OKS, revision time and indication were listed for each patient (Table 3). Deep infection caused 13 revisions (1 (0.3%) in Aarhus, 1 (0.5%) in Aalborg and 11 (1.2%) in Copenhagen, p = 0.4).
Radiographic classification of knee osteoarthritis
Blinded K–L and Ahlbäck classifications of OA severity were made for 1051 radiographs (86% available of 1228, after exclusions) and radiographs were ranked from no. 1 to 1051 (no. 1 most severe) based on surgeons’ 17,767 direct comparisons [16, 18].
Patient-reported outcome measures (PROMs)
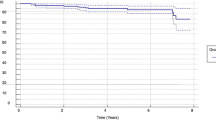
OKS at 1 year did not differ significantly among the three hospitals (39 ± 7, p = 0.1) (Fig. 1a, Table 4), nor when adjusted for age and sex, or when further adjusted for baseline OKS and EQ-VAS and variables that differed among hospitals preoperatively, i.e., BMI, anxiety and depression symptoms, and radiographic classification (Ahlbäck or K–L). OKS change at 1 year was lower in Aarhus (+ 1.6 in Aalborg, CI 0.07–3, and + 1.3 in Copenhagen, CI 0.2–2, respectively) (Fig. 1b, Table 4). This conclusion was partially modified by adjusting for age, sex and baseline OKS (+ 1.0 in Aalborg, CI -0.3–2, + 1.1 in Copenhagen, CI 0.2–2), and when additional adjustments were made for BMI, EQ-VAS, anxiety and depression and radiographic classification, there were no significant differences between hospitals (Aalborg CI -0.4–3, Copenhagen CI -0.1–2, p > 0.2).
At 1 year, 19% of patients in Aarhus, 13% in Aalborg, and 14% in Copenhagen did not attain the MIC of 8 OKS points (p = 0.051). To fairly account for the distribution of revised patients at 1 year, a new analysis was conducted in which all 28 revision patients, that were excluded from the latter analysis, were now assigned an imputed (hypothetic) change score below MIC. The new proportions of patients not attaining MIC in the three hospitals were now 20%, 15% and 16%, respectively (p = 0.2). Comparing the “last available” postoperative OKS change score of 1414 patients with at least one postoperative response (including 17 revision patients), hospitals did not differ significantly (21, 16 and 16%, respectively, p = 0.07).
When studied over time, OKS was higher at 6 weeks in Copenhagen (27.7 ± 7) than in Aarhus (25.6 ± 8) and Aalborg (26.1 ± 7) (p = 0.001, unadjusted) (Fig. 2a). This hospital difference was nuanced when MUKA and TKA patients were studied separately (Fig. 2b), and other PROMs did not vary over time between hospitals (Table 5 depicts the complete sample). Through the entire study period, OKS differed between TKA and MUKA patients, e.g., 1-year OKS was 38.7 and 40.3, respectively (CI 0.6–3).
Patient satisfaction and willingness to repeat surgery were no different between hospitals at 1 year (Table 4). Aalborg patients gained more in general health (EQ-VAS change, p < 0.001). Aarhus patients had better knee extension at 1 year, but when adjustments for baseline motion were made, 1-year extension (and flexion) were independent of hospital. In contrast, MUKA was associated with a greater increase in 1-year flexion (+ 0.34 CKRS flexion points, p < 0.001) after baseline adjustments when compared to TKA, but not to increased extension (p = 0.3) (Fig. 3a, b).
a, b Patient-reported a flexion and b extension after primary knee arthroplasty in the total sample, grouped by implant type (MUKA or TKA only), assessed with Copenhagen Knee ROM Scale. Whiskers denote mean ± 2 × std. error of the mean. Based on validation studies, flexion “4” corresponds to mean 101°, “5” to 121°, and 6 to 131°. In extension, “3” refers to mean 7°, “4” to 5°, and “5” to 1°
Hospital variation in results for comparable patients
When all patients were grouped by preoperative Ahlbäck or K–L classification, neither “willingness to repeat surgery”, 1-year OKS or “last postoperative OKS” varied significantly between hospitals (p = 0.09–1) (Fig. 4). An exception, however, was the “K–L 4” group of 64 patients, where the 17 Aarhus patients had 4–6 points lower 1-year OKS (CI 0.04–11) and 4–6 points lower “last postoperative OKS” (CI 0.03–10). With the frequent use of MUKA in Aarhus, it should be emphasized that only two “K-L 4” patients in Aarhus had MUKA and their 1-year OKS were 37 and 40, respectively. When patients were grouped by OKS at baseline (0–20, 21–30 and 30–48), none of the three aforementioned outcomes varied among hospitals (P = 0.2–0.5) (total sample displayed in Fig. 5). For patients with equivalent OKS results at 1 year (grouped by 10-point intervals), willingness to repeat surgery was independent of hospital (p = 0.2–0.8).
Revision rate development
During the study period, the Danish Knee Arthroplasty Register observed a reduction in 2-year CRR variation between hospitals and regions (Table 6) [28].
Discussion
Patients who underwent primary KA surgery across three Danish high-volume centres with a history of varied CRRs had comparable postoperative results when measured with PROMs, patient-reported knee ROM, patient satisfaction and willingness to repeat surgery. Across the three hospitals, patients with comparable preoperative radiographic knee OA or symptoms (OKS) had similar postoperative OKS results and were equally willing to repeat surgery, suggesting an overall homogeneity in the quality of treatment. This contradicts the conclusion that could be drawn from implant survival statistics alone, where high hospital CRRs are generally seen as indicative of inferior surgical outcomes. The CRRs provided by national KA registries are efficient means to detect poor performance of implants, techniques, hospitals or even surgeons, but they offer little information about treatment results in the far majority of patients; those who are not revised [8, 19, 22]. Outcome of surgery is not a yes-or-no question, but rather a wide spectrum ranging from a satisfied patient with a perfectly functioning prosthesis to an ill, infected patient in definite need of revision surgery. To quantify and eventually improve surgical quality, outcome evaluation should reflect this fact.
Strengths and limitations
An observational cohort study was considered the most suitable design to explore the clinical reality behind the wide variations in Danish regional KA revision rates. With this design, however, no conclusions can be made regarding casual relationships. The three hospitals were selected to represent their respective regions; nonetheless, the results may not necessarily reflect the regional context. Despite the intention to invite virtually all primary KA patients, the average rate of participation was roughly 56%. Participants closely matched the demography and implant distribution of the total surgical population, but socioeconomic information was missing, general health data adhered from patient reports alone (EQ-5D-5L, smoking, alcohol consumption, height and weight), and patients who were unable to respond electronically were only allowed to participate in one-third of the study period [16, 7, 9]. In Aalborg, the larger gain in EQ variables was unexplained, but inclusion bias cannot be ruled out, given that only 38% participated here.
The study was strengthened by high response rates; 89% replied prior to surgery, and 97% of those participants responded after surgery (90% at 1 year).
The three hospitals differed in implant selection, introducing an important confounder which was inseparable from the hospital factor. In the total sample, there were variations in outcomes between MUKA and TKA patients, but although Aarhus used unicompartmental implants twice as frequently as the other two hospitals, implant-related differences were not readily apparent in the overall comparisons [13]. As an exception, Aarhus showed a tendency to have superior 1-year ROM. After adjusting for baseline flexion, the greater 1-year flexion gain in MUKA patients overall was + 0.3 CKRS points compared to TKA patients, which corresponds to about 5°, yet, the clinical relevance of differences in patient-reported ROM were not quantified as part of the CKRS scale validation [14].
In one low-revision hospital (Aarhus), there was a tendency of lower OKS change scores and fewer patients reaching MIC. Note, that the study cannot answer whether particular patients with poor progress would have benefited from revision surgery. The slightly higher OKS (+ 1.9) in Copenhagen patients at 6 weeks postoperatively may indicate a faster recovery that could be related to more frequent use of physiotherapy in rehabilitation. No differences were observed in other parameters, such as ROM, and when data were stratified by implant type, a different pattern was observed (Fig. 2b), suggesting that the finding may represent a sporadic and clinically insignificant variation [4].
Even though the SPARK study was motivated by regional differences in revision rates, revision surgery was not the main objective of the study, and the relatively few SPARK participants who underwent revision surgery during the first year were not expected to be representative of recent years’ practice. Yet, the contributions of the 28 patients who underwent revision were not disregarded, and efforts were made to compensate for the absence of 1-year PROMs in this group by use of transparent imputations.
The historical hospital differences in CRR were not confirmed in this cohort. This was anticipated given the sample size, but it is noteworthy that during the study period, variations in CRR did decrease at both the hospital and regional levels in Denmark [28]. This may represent a random variation or a general tendency. It cannot be ruled out that awareness of the ongoing SPARK study may have altered revision thresholds and patterns. As surgeon staffs and procedures have remained largely the same between past years and the study period, it seems unlikely that the quality of primary KA has changed at uneven pace in the three hospitals.
Having conducted this necessary comparison of primary KA results across Danish hospitals and regions, the next logical step in the search for explanations for revision rate variations would be a nationwide investigation of both revision thresholds and the benefit to patients from revision surgery. Such studies followed by discussions about revision indications and techniques might serve the patients with poor results as much as the ongoing attempts to refine primary knee replacement surgery.
Conclusions
Patient-reported results 1 year after primary knee arthroplasty were comparable across three high-volume centres whose revision rates had varied for a decade. It follows, that hospital variance in revision rates does not necessarily reflect differences in the overall quality of primary surgery. Further studies focusing specifically on revision procedures should determine whether patients across regions and hospitals are offered revision surgery on the same clinical grounds.
Data availability
Raw data is available upon request.
References
Ahlbäck S, Rydberg J (1980) Röntgenologisk klassifikation och undersökningsteknik vid gonartros. Lakartidningen 77(2091–2093):2096
Beard DJ, Harris K, Dawson J, Doll H, Murray DW, Carr AJ, Price AJ (2015) Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 68:73–79
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27:430-436.e1
Bravi M, Longo UG, Laurito A, Greco A, Marino M, Maselli M, Sterzi S, Santacaterina F (2022) Supervised versus unsupervised rehabilitation following total knee arthroplasty: A systematic review and meta-analysis. Knee 40:71–89
Clement ND, Macdonald D, Burnett R, Simpson A, Howie CR (2017) A patient’s perception of their hospital stay influences the functional outcome and satisfaction of total knee arthroplasty. Arch Orthop Trauma Surg 137:693–700
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69
Dunbar MJ, Robertsson O, Ryd L (2004) What’s all that noise? The effect of co-morbidity on health outcome questionnaire results after knee arthroplasty. Acta Orthop Scand 75:119–126
Goodfellow JW, O’Connor JJ, Murray DW (2010) A critique of revision rate as an outcome measure: re-interpretation of knee joint registry data. J Bone Joint Surg Br 92:1628–1631
Harcourt WG, White SH, Jones P (2001) Specificity of the Oxford knee status questionnaire. The effect of disease of the hip or lumbar spine on patients’ perception of knee disability. J Bone Joint Surg Br 83:345–347
Harris K, Dawson J, Gibbons E, Lim CR, Beard DJ, Fitzpatrick R, Price AJ (2016) Systematic review of measurement properties of patient-reported outcome measures used in patients undergoing hip and knee arthroplasty. Patient Relat Outcome Meas 7:101–108
Ingelsrud LH, Roos EM, Terluin B, Gromov K, Husted H, Troelsen A (2018) Minimal important change values for the Oxford Knee Score and the Forgotten Joint Score at 1 year after total knee replacement. Acta Orthop 89:541–547
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Khatib Y, Badge H, Xuan W, Naylor JM, Harris IA (2020) Patient satisfaction and perception of success after total knee arthroplasty are more strongly associated with patient factors and complications than surgical or anaesthetic factors. Knee Surg Sports Traumatol Arthrosc 28:3156–3163
Mørup-Petersen A, Holm PM, Holm CE, Klausen TW, Skou ST, Krogsgaard MR, Laursen MB, Odgaard A (2018) Knee osteoarthritis patients can provide useful estimates of passive knee range of motion: development and validation of the Copenhagen Knee ROM Scale. J Arthroplasty 33:2875–2883.e3
Mørup-Petersen A, Skou ST, Holm CE, Holm PM, Varnum C, Krogsgaard MR, Laursen M, Odgaard A (2021) Measurement properties of UCLA Activity Scale for hip and knee arthroplasty patients and translation and cultural adaptation into Danish. Acta Orthop 92:681–688
Mørup-Petersen A, Krogsgaard MR, Laursen M, Madsen F, Mongelard KBG, Rømer L, Winther-Jensen M, Odgaard A (2023) Hospital variation in revision rates after primary knee arthroplasty was not explained by patient selection: baseline data from 1452 patients in the Danish prospective multicenter cohort study, SPARK. Knee Surg Sports Traumatol Arthrosc
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg Br 89:1010–1014
Pedersen MM, Mongelard KBG, Mørup-Petersen A, Kristensen KB, Odgaard A (2021) Clinicians’ heuristic assessments of radiographs compared with Kellgren-Lawrence and Ahlbäck ordinal grading: an exploratory study of knee radiographs using paired comparisons. BMJ Open 11(3):04793
Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, Carr A, Beard D (2018) Knee replacement. Lancet 392:1672–1682
RCoreTeam RStudio version 1.1.463. https://www.R-project.org/. R: A Language and Environment for Statistical Computing.
Robertsson O, Ranstam J (2003) No bias of ignored bilaterality when analysing the revision risk of knee prostheses: Analysis of a population based sample of 44,590 patients with 55,298 knee prostheses from the national Swedish Knee Arthroplasty Register. BMC Musculoskelet Disord 4:1
Robertsson O, Ranstam J, Lidgren L (2006) Variation in outcome and ranking of hospitals: an analysis from the Swedish knee arthroplasty register. Acta Orthop 77:487–493
Shohat N, Heller S, Sudya D, Small I, Khawalde K, Khatib M, Yassin M (2022) Mild radiographic osteoarthritis is associated with increased pain and dissatisfaction following total knee arthroplasty when compared with severe osteoarthritis: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 30:965–981
Sundhedsdatastyrelsen (2019) The Danish National Health Register. (Landspatientregistret) https://www.esundhed.dk/Registre/Landspatientsregisteret/Operationer.
Terluin B, Eekhout I, Terwee CB, De Vet HCW (2015) Minimal important change (MIC) based on a predictive modeling approach was more precise than MIC based on ROC analysis. J Clin Epidemiol 68:1388–1396
The Danish Knee Arthoplasty Register. Annual Report 2016.
The Danish Knee Arthoplasty Register. Annual Report 2018.
The Danish Knee Arthoplasty Register. Annual Report 2021.
Wall CJ, Vertullo CJ, Kondalsamy-Chennakesavan S, Lorimer MF, de Steiger RN (2022) A prospective, longitudinal study of the influence of obesity on total knee arthroplasty revision rate: results from the australian orthopaedic association national joint replacement registry. J Bone Joint Surg Am 104:1386–1392
Acknowledgements
Authors thank the following for valuable contributions to the study: Kristian Mongelard, Lone Rømer, Birthe Schøning, Heidi Ladefoged Poulsen, Camilla Grube, Naima Elsayed, Ulla Hornum, Gitte Broholm, Patricia Svare, Tina Isaksen, Gitte Raae Høybye, Anette Enemark-Larsen, Svend Erik Østgaard, Lasse Enkebølle Rasmussen, Thomas Bjerno, Lars Peter Møller, Snorre Stephensen, Thomas Lind, Henrik Schrøder, Søren Rytter, Claus Fink Jepsen, Andreas Kappel, Procordo ApS, medical students, Department of Orthopaedic Surgery, Herlev-Gentofte Hospital, and all patients for their time and efforts put in this study.
Funding
Open access funding provided by Royal Danish Library. The work was supported by The Health Research Fund of the Capital Region of Denmark (July 2015 Grant) and the Fund of the Kjaersgaard Family, Sunds (J.no. 6041401). The funding sources did not play any role in the collection, analysis or interpretation of data.
Author information
Authors and Affiliations
Contributions
AO initiated the study, and FM, MK, ML, AO and AM planned it. FM, ML and AO facilitated patient inclusion. MW participated in planning and interpretation of analyses. AM was in charge and took part in all aspects of the project and performed data collection (supported by AO) as well as statistical analyses. All authors contributed to discussions of findings and critically revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors have reported no conflicts of interests.
Ethical approval
The National Committee of Health Research Ethics approved the ethical aspects (Protocol no. 16038343, 2 September 2016) and data storage was approved by the Danish Data Protection Agency (Jr. no. 2012–58-0004, HGH-2016–087, I-Suite no. 04819). Permissions to use restricted questionnaires were obtained through each license provider.
Informed consent
All patients gave written consent to participate and for authors to access hospital charts.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mørup-Petersen, A., Krogsgaard, M.R., Laursen, M. et al. Patients in high- and low-revision hospitals have similar outcomes after primary knee arthroplasty: 1-year postoperative results from the Danish prospective multicenter cohort study, SPARK. Knee Surg Sports Traumatol Arthrosc 31, 3487–3499 (2023). https://doi.org/10.1007/s00167-023-07390-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07390-3