Abstract
Purpose
The purpose of this study was to determine the results of arthroscopic rotator cuff repair (ARCR) in terms of return to work (RTW).
Methods
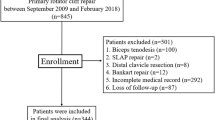
Inclusion criteria were working patients who underwent ARCR for rotator cuff rupture at the study site between 2008 and 2020 and minimum 12 months of follow-up. Patients were stratified based on the physical demand of their work according to the Canadian Classification and Dictionary of Occupations. The primary outcomes were time to RTW, level of employment (LoE), change of tasks, and work loss. Secondary outcomes included the return to sports activities, EQ-VAS, EQ-5D-5L, DASH, and Oxford Shoulder Score.
Results
Three-hundred and eighty-three patients were enrolled; at the follow-up evaluation, fifty-three patients (13.8%) lost their job, with a percentage of 34.4% (eleven patients) in the heavy-work category, and five patients (1.3%) chose early retirement. Other twenty-six patients (6.8%) had to lower their level of employment, and twenty patients (5.2%) changing their tasks, with 279 patients (72.9%) returning to their previous work activity. RTW was obtained at a mean time of 4.7 ± 4.6 months, ranging from 3.8 ± 3.1 months in the sedentary work vs 5.8 ± 2.8 months in the very heavy-work category (p = 0.015). The mean EQ-VAS score was 77.3 ± 18 points, the mean Oxford Shoulder Score was 43.4 ± 7.2 points, and the mean DASH score was 9.9 ± 14.5 points; 75.3% returned to their previous level of sport activity.
Conclusions
The success of ARCR in terms of RTW is not always complete and varies significantly based on the physical demand of the patient’s job. Patients with physically demanding work have a significantly higher time to RTW, reduction of the LoE, and job loss rate, thus affecting the possibility to have a satisfactory return to their previous life. The findings are of clinical relevance since they can help the surgeons to give their patients reliable expectations and to correctly plan the post-operative management.
Level of evidence
IV.


Similar content being viewed by others
References
Aagaard KE, Randeblad P, Abu-Zidan FM, Lunsjö K (2020) Return to work after early repair of acute traumatic rotator cuff tears. Eur J Trauma Emerg Surg 46:817–823
Altintas B, Anderson N, Dornan GJ, Boykin RE, Logan C, Millett PJ (2020) Return to sport after arthroscopic rotator cuff repair: is there a difference between the recreational and the competitive athlete? Am J Sports Med 48:252–261
Audigé L, Bucher HCC, Aghlmandi S, Stojanov T, Schwappach D, Hunziker S et al (2021) Swiss-wide multicentre evaluation and prediction of core outcomes in arthroscopic rotator cuff repair: protocol for the ARCR_Pred cohort study. BMJ Open 11:e045702
Carr AJ, Cooper CD, Campbell MK, Rees JR, Moser J, Beard DJ et al (2015) Clinical effectiveness and cost-effectiveness of open and arthroscopic rotator cuff repair [the UK rotator cuff surgery (UKUFF) randomised trial]. Health Technol Assess 19:1–218
Chen M, Xu W, Dong Q, Huang Q, Xie Z, Mao Y (2013) Outcomes of single-row versus double-row arthroscopic rotator cuff repair: a systematic review and meta-analysis of current evidence. Arthroscopy 29:1437–1449
Cho C-H, Bae K-C, Kim D-H (2022) Incidence and risk factors for early postoperative stiffness after arthroscopic rotator cuff repair in patients without preoperative stiffness. Sci Rep 12:3132
Cho CH, Ye HU, Jung JW, Lee YK (2015) Gender affects early postoperative outcomes of rotator cuff repair. Clin Orthop Surg 7:234–240
Choi S, Kim MK, Kim GM, Roh YH, Hwang IK, Kang H (2014) Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elbow Surg 23:1675–1681
Collin P, Abdullah A, Kherad O, Gain S, Denard PJ, Lädermann A (2015) Prospective evaluation of clinical and radiologic factors predicting return to activity within 6 months after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 24:439–445
Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL (2012) National trends in rotator cuff repair. J Bone Joint Surg Am 94:227–233
Dawson J, Fitzpatrick R, Carr A (1996) Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 78:593–600
Ensor KL, Kwon YW, Dibeneditto MR, Zuckerman JD, Rokito AS (2013) The rising incidence of rotator cuff repairs. J Shoulder Elbow Surg 22:1628–1632
EuroQol, (1990) A new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Fermont AJ, Wolterbeek N, Wessel RN, Baeyens JP, de Bie RA (2014) Prognostic factors for successful recovery after arthroscopic rotator cuff repair: a systematic literature review. J Orthop Sports Phys Ther 44:153–163
Green CK, Scanaliato JP, Dunn JC, Rosner RS, Parnes N (2022) Rates of return to manual labor after arthroscopic rotator cuff repair. Am J Sports Med 50:2227–2233
Gulotta LV, Nho SJ, Dodson CC, Adler RS, Altchek DW, MacGillivray JD (2011) Prospective evaluation of arthroscopic rotator cuff repairs at 5 years: part II–prognostic factors for clinical and radiographic outcomes. J Shoulder Elbow Surg 20:941–946
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The upper extremity collaborative group (UECG). Am J Ind Med 29:602–608
Imai T, Gotoh M, Hagie K, Fukuda K, Ogino M, Madokoro K et al (2019) Factors affecting return to work in patients undergoing arthroscopic rotator cuff repair. Prog Rehabil Med 4:20190006
Kendrick D, Vinogradova Y, Coupland C, Christie N, Lyons RA, Towner EL et al (2012) Getting back to work after injury: the UK burden of Injury multicentre longitudinal study. BMC Public Health. https://doi.org/10.1186/1471-2458-12-584
Ludwig K, Graf von der Schulenburg JM, Greiner W (2018) German value set for the EQ-5D-5L. Pharmacoeconomics 36:663–674
Minagawa H, Yamamoto N, Abe H, Fukuda M, Seki N, Kikuchi K et al (2013) Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: from mass-screening in one village. J Orthop 10:8–12
Namdari S, Donegan RP, Chamberlain AM, Galatz LM, Yamaguchi K, Keener JD (2014) Factors affecting outcome after structural failure of repaired rotator cuff tears. J Bone Joint Surg Am 96:99–105
National Occupational A, Classification S (1985) CCDO guide : Canadian classification and dictionary of occupations. Employment and Immigration Canada, Ottawa (ISBN 0708-6091)
Neyton L, Godenèche A, Nové-Josserand L, Carrillon Y, Cléchet J, Hardy MB (2013) Arthroscopic suture-bridge repair for small to medium size supraspinatus tear: healing rate and retear pattern. Arthroscopy 29:10–17
Nové-Josserand L, Liotard JP, Godeneche A, Neyton L, Borel F, Rey B et al (2011) Occupational outcome after surgery in patients with a rotator cuff tear due to a work-related injury or occupational disease. A series of 262 cases. Orthop Traumatol Surg Res 97:361–366
Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS (2009) Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy 25:30–39
Randelli P, Spennacchio P, Ragone V, Arrigoni P, Casella A, Cabitza P (2012) Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg 96:9–16
Romeo AA, Hang DW, Bach BR Jr, Shott S (1999) Repair of full thickness rotator cuff tears. Gender, age, and other factors affecting outcome. Clin Orthop Relat Surg 367:243–255
Sabo MT, LeBlanc J, Hildebrand KA (2021) Patient gender and rotator cuff surgery: are there differences in outcome? BMC Musculoskelet Disord 22:838
Shields E, Thirukumaran C, Noyes K, Voloshin I (2017) A review of a workers’ compensation database 2003 to 2013: patient factors influencing return to work and cumulative financial claims after rotator cuff repair in geriatric workers’ compensation cases. Geriatr Orthop Surg Rehabil 8:208–214
Spennacchio P, Banfi G, Cucchi D, D’Ambrosi R, Cabitza P, Randelli P (2015) Long-term outcome after arthroscopic rotator cuff treatment. Knee Surg Sports Traumatol Arthrosc 23:523–529
van der Meijden OA, Westgard P, Chandler Z, Gaskill TR, Kokmeyer D, Millett PJ (2012) Rehabilitation after arthroscopic rotator cuff repair: current concepts review and evidence-based guidelines. Int J Sports Phys Ther 7:197–218
Wieser K, Bouaicha S, Grubhofer F (2019) Rotatorenmanschettenruptur: Wann ist die konservative und wann die operative Therapie indiziert? Praxis 108:257–268
Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H et al (2010) Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 19:116–120
Acknowledgements
The authors thank Elettra Pignotti, PhD, for her work in statistical analysis.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members. Christian Candrian has received institutional support outside the present work from Medacta International SA, Johnson & Johnson, Lima Corporate, Zimmer Biomet, and Oped AG.
Ethical approval
The local Ethical Committee of Canton Ticino approved the current study; the assigned number is Study 2021–00486/CE 3836.
Informed consent
In accordance with the Swiss Law, every patient involved in the study signed an informed consent form, approved by the local Ethical Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feltri, P., Monteleone, A.S., Marbach, F. et al. Arthroscopic rotator cuff repair: patients with physically demanding work have significantly worse time to return to work, level of employment, and job loss. Knee Surg Sports Traumatol Arthrosc 31, 153–160 (2023). https://doi.org/10.1007/s00167-022-07172-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07172-3