Abstract
Purpose
To evaluate the rate of return to pre-injury type of sports (RTS type) in patients after revision anterior cruciate ligament reconstruction (ACLR) with lateral extra-articular tenodesis (LET) compared to patients after revision ACLR without LET.
Methods
Seventy-eight patients who underwent revision ACLR with an autologous ipsilateral bone-patellar tendon-bone autograft with and without LET were included at least one year after surgery (mean follow-up: 43.9, SD: 29.2 months). All patients filled in a questionnaire about RTS type, the Knee injury and Osteoarthritis Outcome Score (KOOS), the International Knee Documentation Committee subjective form (IKDCsubjective), and the Tegner activity score.
Results
The RTS type for revision ACLR with LET was 22 of 42 (52%), whereas 11 of 36 (31%) of the patients who underwent revision ACLR without LET returned to the pre-injury type of sport (p = 0.05). No significant differences were found in KOOS subscores, IKDCsubjective, and Tegner activity scores.
Conclusion
An additional LET increases the rate of RTS type after revision ACLR.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Return to sports rate after revision anterior cruciate ligament (ACL) reconstruction (ACLR) is low; about half of the patients after revision ACLR are reported to return to their pre-injury type of sports (RTS type) [11, 22]. One of the reasons for the low RTS type might be the presence of residual rotational laxity after ACLR. Because injury to structures in the anterolateral corner (ALC) of the knee is reported to result in a decrease in rotational stability [15], an increasing interest in several extra-articular surgical procedures to stabilize the ALC has been seen in the past years [1, 4], and it has been reported that residual rotational laxity after ACLR decreased when this was combined with ALC reconstruction [2, 7, 13]. Moreover, reduced failure rate, increased subjective outcome scores, anterior tibial translation, and tibial internal rotation have been reported after ACLR combined with ALC reconstruction [2, 3, 12, 16, 17]. Indicators for this procedure seem to be young age (which might be a proxy for activity level [24]), participation in pivoting sports, and chronic ACL injury [18].
One of these extra-articular ALC reconstruction techniques is a lateral extra-articular tenodesis with the iliotibial band (LET) [14]. However, evidence of whether revision ACLR with additional LET increases RTS compared to revision ACLR without LET is lacking. It is expected that patients after an ACLR with high rotational stability of the knee are more likely to RTS type compared to those with low rotational stability. Due to the expected lower rotational laxity after a LET, the RTS type might be higher after ACLR with LET than without LET.
The present study aimed to evaluate the RTS type in patients after revision ACLR combined with LET compared to RTS type in patients after revision ACLR without LET. Moreover, functional outcome scores were evaluated after ACLR with and without LET. It is hypothesized that patients who underwent a combined revision ACLR with LET show higher RTS type and better functional outcome scores than patients who underwent revision ACLR without LET.
Materials and methods
A retrospective cohort study was conducted at the Centre for Orthopaedic Surgery and Sports Medicine OCON in Hengelo, The Netherlands. The institutional review board (IRB) of OCON Centre for Orthopaedic Surgery and Sports Medicine approved this study (IRB nr: 2020101).
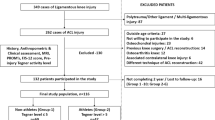
Seventy-eight patients were included for analyses (mean follow-up: 43.9, SD: 29.2, range follow-up 12–192 months; Table 1). Patients who underwent revision ACLR with an autologous ipsilateral bone-patellar tendon-bone (BPTB) between February 2012 and February 2020 and with a minimum follow-up of 1 year were eligible to participate in this study. Exclusion criteria were a history of contralateral ACL injury and re-rupture of the revision ACLR. After inclusion, patients were distributed into two groups: (1) patients who underwent revision ACLR combined with LET (ACLR_LET group), and (2) patients who underwent revision ACLR without LET (ACLR group).
The primary outcome measure was the RTS type (returned/not returned). Secondary outcome measures were: the Dutch versions of the Knee injury and Osteoarthritis Outcome Score (KOOS) [6], the International Knee Documentation Committee subjective form (IKDCsubjective) [8], and the Tegner activity score [20].
Procedure
Together with an explanation of the study, an online questionnaire including homemade open questions about the RTS type [11] (Table 2), the KOOS, IKDCsubjective, and Tegner activity score was sent to patients by e-mail. By submitting the questionnaire, the patients gave their informed consent. After the patients had filled in the questionnaire, the researcher extracted baseline characteristics from the patient’s file and information about the presence or absence of concomitant cartilaginous or meniscal injuries and the graft used for primary ACLR from the patients’ operative form.
Surgical technique
One experienced orthopaedic surgeon (RAGH) performed all surgeries. One-stage or two-stage ACL revision surgery was performed. All ACL revisions were performed using a bone-patellar tendon-bone (BPTB) autograft, which was harvested from the ipsilateral leg. The ACL graft was fixed with interference screws at 20 degrees of knee flexion. LET was performed with a modified deep Lemaire technique as previously described [10, 14] and was fixated with an interference screw (RCI; Smith and Nephew) [9].
Statistical analysis
The data were processed and statistical testing was performed using SPSS version 26 (IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). A Chi-square test was used to compare the distribution of RTS type (returned/not returned) between groups. As the criteria for an independent sample t-test were not met (kurtosis > 1.96), Mann–Whitney U tests were used to compare the KOOS subscales, IKDCsubjective, and Tegner activity score between groups. Moreover, statistical tests were performed to check for differences in baseline characteristics between groups. An alpha level of p ≤ 0.05 was considered statistically significant.
A post-hoc power calculation using proportions of 0.524 and 0.306, an alfa of 0.05, and group sizes of 36 and 42, revealed a power of 50% for analysis regarding RTS type calculated using G*Power 3.1.
Results
Primary outcome: RTS type
A significant RTS type was found between the ACLR_LET (52.4% RTS) and ACLR group (30.6% RTS; X(1) = 3.78, p = 0.05). The level of return to sports is presented in Table 3.
Secondary outcomes: KOOS , IKDC subjective , KOOS, and Tegner activity score
No significant differences were found between the ACLR_LET and ACLR groups in KOOS subscores, IKDCsubjective scale, and Tegner activity score (Table 4).
Discussion
The most important finding of the present study is that more patients returned to their pre-injury type of sports after revision ACLR combined with an additional LET than patients who underwent revision ACLR without additional LET.
One possible explanation that patients with an additional LET are more likely to return to their pre-injury type of sports may be that the laxity of the knee is reduced after this procedure [17]. After ACLR without LET, rotational laxity is reported to be higher than after ACLR with LET [21]. One cadaver and two experimental studies using a hamstring tendon for primary ACLR combined with an extra-articular lateral reconstruction procedure indeed showed that the internal rotational laxity of the knee was lower compared to ACLR without extra-articular lateral reconstruction [7, 17]. Lower rotational laxity will increase the stability of the knee and may increase the trust in the knee and, therefore, may increase RTS probabilities. Moreover, in cadavers, untreated ALC injuries, together with untreated meniscal tears and collateral ligament tears, could lead to an overload of the ACL (graft) and consequently higher changes to graft failure [23]. Indeed, previous studies showed that after (primary) ACLR with extra-articular lateral reconstruction, the failure rate is considerably decreased, suggesting higher stability of the knee [2, 5, 19].
In line with the current study, Lee et al. [13] also found a higher return to sports level after revision ACLR combined with an extra-articular lateral reconstruction procedure using allograft tendons for ACLR compared to ACLR without extra-articular lateral reconstruction. In contrast with the current study, they also found higher IKDC and Tegner activity score after the combined procedure. A higher IKDC and Tegner activity score and higher KOOSsymptom and KOOSsport scores were also found in other studies [2, 7]. No significant differences was found between groups in the IKDC score, KOOS subscores, or Tegner activity score. The differences in findings may be because of differences in graft choice: Lee et al. [13] used allografts, Alm et al. [2] used hamstring, BPTB and quadriceps autografts, whereas in the present study only BPTB autografts were used. Patients who are operated using specific types of grafts, such as allografts and hamstring tendons, for ACLR might benefit more from an extra-articular lateral reconstruction procedure. The absence of significant differences between groups in IKDC, Tegner activity score, and KOOS scores in the current study might also be due to the low number of patients in the current study (power < 13%).
Besides the retrospective nature of the present study, there are some other limitations. No objective instrumented assessments such as passive rotational knee laxity were used to measure knee function. Another limitation is the significant difference in time between participation and surgery between the ACLR_LET (30.7 months) and ACL group (62.4 months). This significant difference is due to the transition of surgical technique from revision ACLR without to revision ACLR with LET. This may have influenced the RTS type between the two groups. However, a subgroup analysis where the groups had equal time between surgery and participation could not be performed as the number of participants would have been too small. Moreover, no subgroup analysis with a follow-up of 2 years was performed. This is because the power is too small for this analysis and approximately the same percentage of the patients included in our study with a follow-up of 1 year returned to sports (42%) compared to the patients with a follow-up of two years (45.6%). In addition, the sample size of this study was low and, therefore, our results should be interpreted as an indication and not as definite.
The clinical relevance of the present study is that it provides evidence for using an additional LET in combination with a revision ACLR with BPTP as RTS is higher after ACLR with LET than ACLR without LET.
Conclusion
A combined LET with revision ACLR in patients after failure of a primary ACLR increases the rate of return to the pre-injury type of sports compared to revision ACLR without LET. Therefore, an additional LET combined with a revision ACLR is beneficial for those patients and should be considered by orthopaedic surgeons.
References
Ahn JH, Koh IJ, McGarry MH, Patel NA, Lin CC, Lee TQ, Kim S (2020) Knee laxity in anterolateral complex injuries versus lateral meniscus posterior horn injuries in anterior cruciate ligament deficient knees: a cadaveric study. Knee 27(2):363–374
Alm L, Drenck TC, Frosch KH, Akoto R (2020) Lateral extra-articular tenodesis in patients with revision anterior cruciate ligament (ACL) reconstruction and high-grade anterior knee instability. Knee 27(5):1451–1457
Aryana IGNW, Subawa IW, Dusak IWS, Dharmayuda CGO, Nugraha HK, Deslivia MF (2022) Functional outcome of lateral extraarticular tenodesis (LET) procedure in addition to anterior cruciate ligament reconstruction: a metaanalysis. Rev Bras Ortop 57(1):033–040
Castelli A, Zanon G, Jannelli E, Ivone A, Ferranti Calderoni E, Combi A, Mosconi M, Benazzo F (2020) The role of the anterolateral ligament in knee’s biomechanics: a case–control retrospective study. Eur J Orthop Surg Traumatol 30(4):653–658
Getgood AMJ, Bryant DM, Litchfield R, Heard M, Mccormack RG, Rezansoff A, Peterson D, Bardana D, Macdonald PB, Verdonk PCM, Spalding T, Group S (2020) Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction 2-year outcomes from the STABILITY study randomized clinical trial. Am J Sports Med 48(2):285–297
de Groot IB, Favejee MM, Reijman M, Verhaar JAN, Terwee CB (2008) The Dutch version of the knee injury and osteoarthritis outcome score: a validation study. Health Qual Life Outcomes. https://doi.org/10.1186/1477-7525-6-16
Hamido F, Habiba AA, Marwan Y, Soliman ASI, Elkhadrawe TA, Morsi MG, Shoaeb W, Nagi A (2020) Anterolateral ligament reconstruction improves the clinical and functional outcomes of anterior cruciate ligament reconstruction in athletes. Knee Surg Sports Traumatol Arthrosc 29(4):1173–1180
Haverkamp D, Sierevelt IN, Breugem SJM, Lohuis K, Blankevoort L, Van Dijk CN (2006) Translation and validation of the Dutch version of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med 34(10):1680–1684
Inderhaug E, Stephen JM, Williams A, Amis AA (2017) Anterolateral tenodesis or anterolateral ligament complex reconstruction: effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med 45(13):3089–3097
Inderhaug E, Stephen JM, Williams A, Orth F, Amis AA (2017) Biomechanical comparison of anterolateral procedures combined with anterior cruciate ligament reconstruction. Am J Sports Med 45(2):347–354
Keizer MNJ, Hoogeslag RAG, van Raay JJAM, Otten E, Brouwer RW (2018) Superior return to sports rate after patellar tendon autograft over patellar tendon allograft in revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 26(2):574–581
Laboudie P, Douiri A, Bouguennec N, Biset A, Graveleau N (2022) Combined ACL and ALL reconstruction reduces the rate of reoperation for graft failure or secondary meniscal lesions in young athletes. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-06956-x
Lee DW, Kim JG, Cho SI, Kim DH (2019) Clinical outcomes of isolated revision anterior cruciate ligament reconstruction or in combination with anatomic anterolateral ligament reconstruction. Am J Sports Med 47(2):324–333
Lemaire M (1967) Ruptures anciennes du ligament croisé antérieur du genou. J Chir 93(3):311–320
Madhan AS, Patel NM (2020) The anterolateral ligament of the knee. JBJS Rev 8(6):e0136
Perelli S, Morales-Avalos R, Formagnana M, Rojas-Castillo G, Serrancolí G, Monllau JC (2022) Lateral extraarticular tenodesis improves stability in non-anatomic ACL reconstructed knees: in vivo kinematic analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06854-8
Rhatomy S, Ariyanto MW, Fiolin J, Dilogo IH (2022) Comparison of clinical outcomes between isolated ACL reconstruction and combined ACL with anterolateral ligament reconstruction: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-021-03194-8
Saithna A, Thaunat M, RomainDelaloye J, Ouanezar H, Marie Fayard J, Sonnery-Cottet B (2018) Combined ACL and anterolateral ligament reconstruction. JBJS Essent Surg Tech. 8(1):e2
Sonnery-Cottet B, Haidar I, Rayes J, Fradin T, Ngbilo C, Dutra Vieira T, Freychet B, Ouanezar H, Saithna A (2021) A long-term graft rupture rates after combined ACL and anterolateral ligament reconstruction versus isolated ACL reconstruction a matched-pair analysis from the SANTI Study Group. Am J Sports Med 49(11):2889–2897
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Ventura A, Legnani C, Boisio F, Borgo E, Peretti GM (2021) The association of extra-articular tenodesis restores rotational stability more effectively compared to contralateral hamstring tendon autografts ACL reconstruction alone in patients undergoing ACL revision surgery. Orthop Traumatol Surg Res 107(2):102739
Della Villa F, Andriolo L, Ricci M, Filardo G, Gamberini J, Caminati D, Della Villa S, Zaffagnini S (2020) Compliance in post-operative rehabilitation is a key factor for return to sport after revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 28(2):463–469
Van Der Wal WA, Meijer T, Hoogeslag RAG, Laprade RF (2021) Systematic review meniscal tears, posterolateral and posteromedial corner injuries, increased coronal plane, and increased sagittal plane tibial slope all influence anterior cruciate ligamenterelated knee kinematics and increase forces on the native and reconstructed anterior cruciate ligament: a systematic review of cadaveric studies. Arthroscopy 38(5):1664-1688.e1
Webster KE (2021) Editorial commentary: anterior cruciate ligament suture repair could have high failure rates in active athletes of all ages. Arthroscopy 37(4):1202–1203
Acknowledgements
The authors thank Rianne Huis in ‘t Veld, Astrid de Vries and Leid de Vries-Gerritsen, who assisted in the selection of participants.
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Contributions
All auteurs contributed to the design of the study, interpretation of the results and approved the final manuscript. MNJK: did the data analysis and wrote the first draft of the manuscript. FdG, RAGH and RWB: revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Medical Ethical Committee approved the study design, procedure and protocol. The Medical Ethical Committee of OCON Centre for Orthopaedic Surgery and Sports Medicine approved this study (IRB nr: OCON2020101).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Keizer, M.N.J., Brouwer, R.W., de Graaff, F. et al. Higher return to pre-injury type of sports after revision anterior ligament reconstruction with lateral extra-articular tenodesis compared to without lateral extra-articular tenodesis. Knee Surg Sports Traumatol Arthrosc 31, 1699–1703 (2023). https://doi.org/10.1007/s00167-022-07018-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07018-y