Abstract
Purpose
To update previously published outcomes (at 2–8 years) of second revision anterior cruciate ligament reconstruction (ACLR) combined with tibial deflexion osteotomy (TDO), after an interval of 5 more years (at 7–15 years), and monitor evolution of clinical scores and progression of osteoarthritis.
Methods
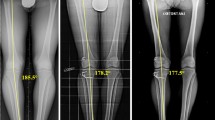
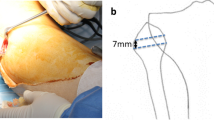
The initial retrospective consecutive series included nine patients that underwent one-stage second revision ACLR with TDO, all of whom were contacted for second follow-up at minimum 7 years. An independent observer collected IKDC-SKF, the Lysholm score, and assessed radiographs for signs of osteoarthritis.
Results
Of the nine original patients, seven were assessed at the clinic, one could only be assessed by telephone, and one was lost to follow-up. At final follow-up of 9.9 ± 3.0 years, the eight patients assessed maintained or improved clinical scores, compared to the previous follow-up at 4.0 ± 2.9 years. The mean Lysholm score improved from 73.8 ± 5.8 (65–82) to 84.5 ± 11.9 (59–95), and IKDC improved from 71.6 ± 6.2 (62–79) to 82.9 ± 12.1 (61–98). Of the three patients that had signs of arthritis at the previous follow-up, the stage of osteoarthritis increased in one (from grade 2 to grade 3), remained unchanged in one, and could not be assessed in one.
Conclusion
At 7–15 years following second revision ACLR with TDO, patients maintained or improved clinical scores compared to the previous follow-up at 2–8 years, without retears or reoperations. Although eight of the nine knees had meniscectomies or meniscal sutures, osteoarthritis progressed in only one of the six knees that had signs of arthritis at the previous follow-up. These results confirm that TDO can protect the ACL graft from retear, with minimal progression of osteoarthritis and/or risks of meniscal tears, suggesting that correction of excessive tibial slope should be considered when performing ACLR, whether a revision or primary procedure.

Similar content being viewed by others
References
Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P (2004) Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg 124(9):575–584
Akoto R, Alm L, Drenck TC, Frings J, Krause M et al (2020) Slope-correction osteotomy with lateral extra-articular tenodesis and revision anterior cruciate ligament reconstruction Is highly effective in treating high-grade anterior knee laxity. Am J Sports Med 48(14):3478–3485
Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L et al (2014) Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med 42(5):1049–1057
Bernhardson AS, Aman ZS, Dornan GJ, Kemler BR, Storaci HW et al (2019) Tibial slope and Its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med 47(2):296–302
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR et al (2006) The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22(8):894–899
Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS et al (2015) Lateral tibial posterior slope is Increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med 43(10):2510–2514
Dejour D, Khun A, Dejour H (1998) Osteotomie tibiale de déflexion et laxité chronique antérieure à propos de 22 cas. Rev Chir Orthop 84:28–29
Dejour D, Saffarini M, Demey G, Baverel L (2015) Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc 23(10):2846–2852
Dejour D, Vanconcelos W, Bonin N, Saggin PR (2013) Comparative study between mono-bundle bone-patellar tendon-bone, double-bundle hamstring and mono-bundle bone-patellar tendon-bone combined with a modified Lemaire extra-articular procedure in anterior cruciate ligament reconstruction. Int Orthop 37(2):193–199
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76(5):745–749
Dini F, Tecame A, Ampollini A, Adravanti P (2019) Multiple ACL revision: failure analysis and clinical outcomes. J Knee Surg 34(8):801–809
Engler ID, Salzler MJ, Wall AJ, Johnson WR, Makani A et al (2020) Patient-reported outcomes after multiple-revision ACL reconstruction: good but not great. Arthrosc Sports Med Rehabil 2(5):e539–e546
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32(2):376–382
Grassi A, Ardern CL, Marcheggiani Muccioli GM, Neri MP, Marcacci M et al (2016) Does revision ACL reconstruction measure up to primary surgery? A meta-analysis comparing patient-reported and clinician-reported outcomes, and radiographic results. Br J Sports Med 50(12):716–724
Grassi A, Kim C, Marcheggiani Muccioli GM, Zaffagnini S, Amendola A (2017) What Is the mid-term failure rate of revision ACL reconstruction? A systematic review. Clin Orthop Relat Res 475(10):2484–2499
Griffith TB, Allen BJ, Levy BA, Stuart MJ, Dahm DL (2013) Outcomes of repeat revision anterior cruciate ligament reconstruction. Am J Sports Med 41(6):1296–1301
Hamrin Senorski E, Svantesson E, Baldari A, Ayeni OR, Engebretsen L et al (2019) Factors that affect patient reported outcome after anterior cruciate ligament reconstruction—a systematic review of the Scandinavian knee ligament registers. Br J Sports Med 53(7):410–417
Horvath A, Senorski EH, Westin O, Karlsson J, Samuelsson K et al (2019) Outcome after anterior cruciate ligament revision. Curr Rev Musculoskelet Med 12(3):397–405
Imhoff FB, Mehl J, Comer BJ, Obopilwe E, Cote MP et al (2019) Slope-reducing tibial osteotomy decreases ACL-graft forces and anterior tibial translation under axial load. Knee Surg Sports Traumatol Arthrosc 27(10):3381–3389
Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC (2010) Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med 38(3):455–463
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Lefevre N, Klouche S, Mirouse G, Herman S, Gerometta A et al (2017) Return to sport after primary and revision anterior cruciate ligament reconstruction: a prospective comparative study of 552 patients from the FAST cohort. Am J Sports Med 45(1):34–41
Napier RJ, Garcia E, Devitt BM, Feller JA, Webster KE (2019) Increased radiographic posterior tibial slope Is associated with subsequent injury following revision anterior cruciate ligament reconstruction. Orthop J Sports Med 7(11):2325967119879373
Ogura T, Ackermann J, Barbieri Mestriner A, Merkely G, Gomoll AH (2020) Minimal clinically important differences and substantial clinical benefit in patient-reported outcome measures after autologous chondrocyte implantation. Cartilage 11(4):412–422
Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J et al (2018) 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med 46(3):531–543
Shelburne KB, Kim HJ, Sterett WI, Pandy MG (2011) Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res 29(2):223–231
Sonnery-Cottet B, Mogos S, Thaunat M, Archbold P, Fayard JM et al (2014) Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med 42(8):1873–1880
Winkler PW, Godshaw BM, Karlsson J, Getgood AMJ, Musahl V (2021) Posterior tibial slope: the fingerprint of the tibial bone. Knee Surg Sports Traumatol Arthrosc 29:1687–1689
Winkler PW, Wagala NN, Hughes JD, Lesniak BP, Musahl V (2021) A high tibial slope, allograft use, and poor patient-reported outcome scores are associated with multiple ACL graft failures. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06460-8
Funding
The authors are grateful to “GCS Ramsay Santé pour l’Enseignement et la Recherche” for funding the statistical analysis and manuscript preparation for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
AR has nothing to declare. FVR has nothing to declare. GD has nothing to declare. MS has nothing to declare. Dr. Dejour reports personal fees from SBM, outside the submitted work.
Ethical approval
All patients had provided written informed consent for the use of their data and images for research and publishing purposes and the institutional review board approved the study in advance (GCS Ramsay Santé pour l'Enseignement et la Recherche, COS-RGDS-2021-03-008-DEJOUR-D).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rozinthe, A., van Rooij, F., Demey, G. et al. Tibial slope correction combined with second revision ACLR grants good clinical outcomes and prevents graft rupture at 7–15-year follow-up. Knee Surg Sports Traumatol Arthrosc 30, 2336–2341 (2022). https://doi.org/10.1007/s00167-021-06750-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06750-1