Abstract
Purpose
To evaluate the influence of time from injury and meniscus tears on the side-to-side difference in anterior tibial translation (SSD-ATT) as measured on lateral monopodal weightbearing radiographs in both primary and secondary ACL deficiencies.
Methods
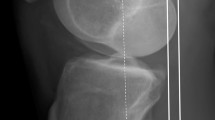
Data from 69 patients (43 males/26 females, median age 27—percentile 25–75: 20–37), were retrospectively extracted from their medical records. All had a primary or secondary ACL deficiency as confirmed by MRI and clinical examination, with a bilateral weightbearing radiograph of the knees at 15°–20° flexion available. Meniscal status was assessed on MRI images by a radiologist and an independent orthopaedic surgeon. ATT and posterior tibial slope (PTS) were measured on the lateral monopodal weightbearing radiographs for both the affected and the contralateral healthy side. A paired t-test was used to compare affected/healthy knees. Independent t-tests were used to compare primary/secondary ACL deficiencies, time from injury (TFI) (≤ 4 years/ > 4 years) and meniscal versus no meniscal tear.
Results
ATT of the affected side was significantly greater than the contralateral side (6.2 ± 4.4 mm vs 3.5 ± 2.8 mm; p < 0.01). There was moderate correlation between ATT and PTS in both the affected and healthy knees (r = 0.43, p < 0.01 and r = 0.41, p < 0.01). SSD-ATT was greater in secondary ACL deficiencies (4.7 ± 3.8 vs 1.9 ± 3.2 mm; p < 0.01), patients with a TFI greater than 4 years (4.2 ± 3.8 vs 2.0 ± 3.0 mm; p < 0.01) and with at least one meniscal tear (3.9 ± 3.8 vs 0.7 ± 2.2 mm; p < 0.01). Linear regression showed that, in primary ACL deficiencies, SSD-ATT was expected to increase (+ 2.7 mm) only if both a meniscal tear and a TFI > 4 years were present. In secondary ACL deficiencies, SSD-ATT was mainly influenced by the presence of meniscal tears regardless of the TFI.
Conclusion
SSD-ATT was significantly greater in secondary ACL deficiencies, patients with a TFI greater than 4 years and with at least one meniscal tear. These results confirm that SSD-ATT is a time- and meniscal-dependent parameter, supporting the concept of gradual sagittal decompensation in ACL-deficient knees, and point out the importance of the menisci as secondary restraints of the anterior knee laxity. Monopodal weightbearing radiographs may offer an easy and objective method for the follow-up of ACL-injured patients to identify early signs of soft tissue decompensation under loading conditions.
Level of evidence
Level III.



Similar content being viewed by others
References
Almekinders LC, Chiavetta JB (2001) Tibial subluxation in anterior cruciate ligament-deficient knees: implications for tibial tunnel placement. Arthroscopy 17(9):960–962
Asmakutlu O, Alis D, Topel C, Bankaoglu M (2021) Patients with ACL graft deficiency showed a higher frequency of knee osteoarthritis compared with patients with intact ACL graft in the medium term. Skeletal Radiol 50:137–148
Barcellona MG, Morrissey MC, Milligan P, Amis AA (2014) The effect of thigh muscle activity on anterior knee laxity in the uninjured and anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc 22:2821–2829
Chavez A, Jimenez AE, Riepen D, Schell B, Khazzam M, Coyner KJ (2020) Anterior cruciate ligament tears: the impact of increased time from injury to surgery on intra-articular lesions. Orthop J Sports Med 8:2325967120967120
Cook RD, Weisberg S (1982) Residuals and influence in regression. Chapman and Hall, New York
Crues JV, Mink J, Levy TL, Lotysch M, Stoller DW (1987) Meniscal tears of the knee: accuracy of MR imaging. Radiology 164:445–448
Dejour D, Pungitore M, Valluy J, Nover L, Saffarini M, Demey G (2019) Preoperative laxity in ACL-deficient knees increases with posterior tibial slope and medial meniscal tears. Knee Surg Sports Traumatol Arthrosc 27:564–572
Dejour D, Pungitore M, Valluy J, Nover L, Saffarini M, Demey G (2019) Tibial slope and medial meniscectomy significantly influence short-term knee laxity following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27(11):3481–3489
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Jt Surg Br 76:745–749
Dejour H, Walch G, Deschamps G, Chambat P (2014) Arthrosis of the knee in chronic anterior laxity. Orthop Traumatol Surg Res 100:49–58
Grassi A, Dal Fabbro G, Di Paolo S, Stefanelli F, Macchiarola L, Lucidi GA, Zaffagnini S (2019) Medial and lateral meniscus have a different role in kinematics of the ACL-deficient knee: a systematic review. J ISAKOS 4(5):233–241
Grassi A, Di Paolo S, Lucidi GA, Macchiarola L, Raggi F, Zaffagnini S (2019) The contribution of partial meniscectomy to preoperative laxity and laxity after anatomic single-bundle anterior cruciate ligament reconstruction. In vivo kinematics with navigation. Am J Sports Med 47:3203–3211
Grassi A, Macchiarola L, Urrizola Barrientos F, Zicaro JP, Costa Paz M, Adravanti P, Dini F, Zaffagnini S (2019) Steep posterior tibial slope, anterior tibial subluxation, deep posterior lateral femoral condyle, and meniscal deficiency are common findings in multiple anterior cruciate ligament failures: an MRI case–control study. Am J Sports Med 47:285–295
Hardy A, Klouche S, Szarzynski P, Charpentier E, Beranger JS, Bauer T, Rousselin B, Judet O, Hardy P (2019) A threshold value of 3.5 mm of passive anterior tibial subluxation on MRI is highly specific for complete ACL tears. Knee Surg Sports Traumatol Arthrosc 27:885–892
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163
Kvist J (2005) Sagittal tibial translation during exercises in the anterior cruciate ligament-deficient knee. Scand J Med Sci Sports 15:148–158
Kvist J, Gillquist J (2001) Anterior positioning of tibia during motion after anterior cruciate ligament injury. Med Sci Sports Exerc 33:1063–1072
Kvist J, Gillquist J (2001) Sagittal plane knee translation and electromyographic activity during closed and open kinetic chain exercises in anterior cruciate ligament-deficient patients and control subjects. Am J Sports Med 29:72–82
Li G, Rudy TW, Allen C, Sakane M, Woo SL (1998) Effect of combined axial compressive and anterior tibial loads on in situ forces in the anterior cruciate ligament: a porcine study. J Orthop Res 16:122–127
Lian J, Novaretti JV, Sheean AJ, Patel NK, Whaley S, Popchak A, Musahl V (2019) Static lateral tibial plateau subluxation predicts high-grade rotatory knee laxity in anterior cruciate ligament-deficient knees. Am J Sports Med 47:277–284
Marom N, Kleeblad LJ, Ling D, Nwachukwu BU, Marx RG, Potter HG, Pearle AD (2020) Pre-operative static anterior tibial translation assessed on MRI does not influence return to sport or satisfaction after anterior cruciate ligament reconstruction. HSSJ 16(suppl 2):475–481
McDonald LS, van der List JP, Jones KJ, Zuiderbaan HA, Nguyen JT, Potter HG, Pearle AD (2017) Passive anterior tibial subluxation in the setting of anterior cruciate ligament injuries: a comparative analysis of ligament-deficient states. Am J Sports Med 45:1537–1546
Mehl J, Otto A, Baldino JB, Achtnich A, Akoto R, Imhoff AB, Scheffler S, Petersen W (2019) The ACL-deficient knee and the prevalence of meniscus and cartilage lesions: a systematic review and meta-analysis (CRD42017076897). Arch Orthop Trauma Surg 139:819–841
Mishima S, Takahashi S, Kondo S, Ishiguro N (2005) Anterior tibial subluxation in anterior cruciate ligament-deficient knees: quantification using magnetic resonance imaging. Arthrosc J 21:1193–1196
Mitchell BC, Siow MY, Bastrom T, Bomar JD, Pennock AT, Parvaresh K, Edmonds EW (2021) Coronal lateral collateral ligament sign: a novel magnetic resonance imaging sign for identifying anterior cruciate ligament-deficient knees in adolescents and summarizing the extent of anterior tibial translation and femorotibial internal rotation. Am J Sports Med 49(4):928–934
Myers RH (1990) Classical and modern regression with applications. PWS-Kent Publishing Company, Boston
Nishida K, Matsushita T, Araki D, Sasaki H, Tanaka T, Hoshino Y, Kanzaki N, Matsumoto T, Nagamune K, Niikura T, Kurosaka M, Kuroda R (2019) Analysis of anterior tibial subluxation to the femur at maximum extension in anterior cruciate ligament-deficient knees. J Orthop Surg (Hong Kong) 27:2309499019833606
Sigonney G, Klouche S, Chevance V, Bauer T, Rousselin B, Judet O, Hardy P (2020) Risk factors for passive anterior tibial subluxation on MRI in complete ACL tear. Orthop Traumatol Surg Res 106:465–468
Snoj Ž, Zupanc O, Stražar K, Salapura V (2017) A descriptive study of potential effect of anterior tibial translation, femoral tunnel and anterior cruciate ligament graft inclination on clinical outcome and degenerative changes. Int Orthop 41:789–796
Song G-Y, Zhang H, Zhang J, Liu X, Xue Z, Qian Y, Feng H (2018) Greater static anterior tibial subluxation of the lateral compartment after an acute anterior cruciate ligament injury is associated with an increased posterior tibial slope. Am J Sports Med 46:1617–1623
Tanaka MJ, Jones KJ, Gargiulo AM, Delos D, Wickiewicz TL, Potter HG, Pearle AD (2013) Passive anterior tibial subluxation in anterior cruciate ligament-deficient knees. Am J Sports Med 41:2347–2352
Tanaka Y, Kita K, Takao R, Amano H, Uchida R, Shiozaki Y, Yonetani Y, Kinugasa K, Mae T, Horibe S (2018) Chronicity of anterior cruciate ligament deficiency, part 2: radiographic predictors of early graft failure. Orthop J Sports Med 6:2325967117751915
Tanaka Y, Kita K, Takao R, Amano H, Uchida R, Shiozaki Y, Yonetani Y, Kinugasa K, Mae T, Horibe S (2018) Chronicity of anterior cruciate ligament deficiency, part 1: effects on the tibiofemoral relationship before and immediately after anatomic ACL reconstruction with autologous hamstring grafts. Orthop J Sports Med 6:2325967117750813
Tashiro Y, Mori T, Kawano T, Oniduka T, Arner JW, Fu FH, Iwamoto Y (2020) Meniscal ramp lesions should be considered in anterior cruciate ligament-injured knees, especially with larger instability or longer delay before surgery. Knee Surg Sports Traumatol Arthrosc 28:3569–3575
Torzilli PA, Deng X, Warren RF (1994) The effect of joint-compressive load and quadriceps muscle force on knee motion in the intact and anterior cruciate ligament-sectioned knee. Am J Sports Med 22:105–112
Uffmann W, ElAttrache N, Nelson T, Eberlein SA, Wang J, Howard DR, Metzger MF (2021) Posterior lateral meniscal root tears increase strain on the reconstructed anterior cruciate ligament: a cadaveric study. Arthrosc Sports Med Rehabil 3(2):505–513
Vahey TN, Hunt JE, Shelbourne KD (1993) Anterior translocation of the tibia at MR imaging: a secondary sign of anterior cruciate ligament tear. Radiology 187:817–819
Wang CK, Lin LC, Sun YN, Lai CS, Chen CH, Kao CY (2021) Computer-assisted system in stress radiography for anterior cruciate ligament injury with correspondent evaluation of relevant diagnostic factors. Diagn (Basel, Switz) 11(3):419
Acknowledgements
The authors would first like to thank the Department of Radiology from the Clinique d'Eich (Centre Hospitalier de Luxembourg) for their help in the standardization and execution of monopodal radiographs.
Funding
No funding was received for the present work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedure performed in this study were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Macchiarola, L., Jacquet, C., Dor, J. et al. Side-to-side anterior tibial translation on monopodal weightbearing radiographs as a sign of knee decompensation in ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc 30, 1691–1699 (2022). https://doi.org/10.1007/s00167-021-06719-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06719-0