Abstract
Purpose
The COVID-19 pandemic has disrupted the health care system around the entire globe. A consensus is needed about resuming total hip and knee procedures. The European Hip Society (EHS) and the European Knee Association (EKA) formed a panel of experts that have produced a consensus statement on how the safe re-introduction of elective hip and knee arthroplasty should be undertaken.
Methods
A prospective online survey was done among members of EHS and EKA. The survey consisted of 27 questions. It includes basic information on demographics and details the participant’s agreement with each recommendation. The participant could choose among three options (agree, disagree, abstain). Recommendations focussed on pre-operative, peri-operative, and post-operative handling of patients and precautions.
Results
A total of 681 arthroplasty surgeons participated in the survey, with 479 fully completing the survey. The participants were from 44 countries and 6 continents. Apart from adhering to National and Local Guidelines, the recommendations concerned how to make elective arthroplasty safe for patients and staff.
Conclusion
The survey has shown good-to-excellent agreement of the participants with regards to the statements made in the recommendations for the safe return to elective arthroplasty following the first wave of the COVID-19 pandemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent months, the SARS-CoV-2 pandemic (COVID-19) has evolved rapidly in Europe, disrupting the personal, social, economic and professional lives of health professionals on a large scale. The overall goal of most governments in Europe has been to flatten the curve of infected SARS-CoV-2 patients and prevent a collapse of national health systems. The April 2020 SARS-CoV-2 survey completed by EHS and EKA members in Europe has confirmed the impact of SARS-CoV-2: this pandemic has resulted in a tremendous reduction in primary hip and knee arthroplasty procedures as shown in the survey. A broad consensus is needed about the factors that need to be in place before restarting such procedures.
Delaying hip and knee arthroplasty in patients with severe osteoarthritis (OA) may lead to increased opioid use. It is associated with lower clinical results and increased readmission rates after the index procedure. Moreover, when access to hip and knee arthroplasty is limited, as it is now in the wake of the COVID-19 sanitary measures, the direct and indirect costs for our health care and social systems are enormous. Many patients suffering from OA have to prolong their absence from work, request temporary unemployment benefits, and burden the public welfare system.
We are now entering a new phase in most European countries, where we can consider restarting elective hip and knee arthroplasty in a “post-pandemic” period. To date, the scientific basis for the existing guidelines is not robust; there is much room for an exchange of ideas between surgeons. The current concern is to map out the optimal trajectory for starting up elective hip and knee arthroplasties. As a result, the European Hip Society (EHS) and the European Knee Association (EKA) formed a panel of experts that have produced a consensus on how the safe re-introduction of elective arthroplasty should be undertaken. They have provided recommendations based on the available evidence [1]. This survey aimed to validate the recommendations by involving arthroplasty surgeons from a wide geographical area to promote then the recommendations for a safe return to elective joint arthroplasty across Europe and elsewhere.
Materials and method
A prospective online survey was done online using SurveyMonkey (Portland, USA: https://www.surveymonkey.com) among members of European Hip Society (EHS) and European Knee Associates (EKA). A link to the survey was sent by email to all members of the EHS and the EKA and affiliated arthroplasty surgeons. The online survey was launched on 23rd May 2020 and concluded on 6th June 2020.
The survey consisted of 27 questions. It includes basic information on demographics and details the participant’s agreement with each recommendation. The participant could choose among three options (agree, disagree, abstain). The recommendations focus on three time periods; pre-operative, per-operative, and post-operative (Table 1).
This survey did not require formal ethical approval with a practice dedicated to adult reconstruction.
Results
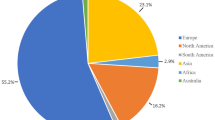
A total of 681 arthroplasty surgeons participated in the survey, with 479 fully completing the survey. The geographical spread of this survey included surgeons from 44 different countries in 6 continents (Fig. 1). The EHS and EKA had a 22.1% and 20.9% response rate, respectively. The mean time in practice for all participants was 20 years (min 1 year–max 46 years).
The detailed results are shown in Table 2.
Discussion
The survey has shown good-to-excellent agreement by the participants to the Statements made in the Recommendations for the safe return to elective arthroplasty following the COVID-19 pandemic. Although the response rate from both the EHS and EKA membership was low, at around 20%, it is notable that the mean time in elective arthroplasty of the participants was 20 years. This means that very experienced surgeons gave their opinions. Coupled with the global coverage of the survey, the mean time in elective arthroplasty is a proper validation for the recommendations.
Conclusion
The survey has shown good-to-excellent agreement of the participants with regards to the statements made in the recommendations for the safe return to elective arthroplasty following the first wave of the COVID-19 pandemic.
References
Kort NP, Gómez Barrena E, Bédar M, Donell S, Epinette JA, Gomberg B et al (2020) Resuming elective hip and knee arthroplasty in the setting of the SARS-CoV-2 pandemic: the European Hip Society and European Knee Associates recommendations. Knee Surg Sports Traumatol Arthrosc
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
NC has provided consultancy services to Stryker Netherlands (amsterdam), Zimmer-Biomet (Warsaw Indiana) and BodyCad. (Naples USA) No other conflicts of interest have been recorded.
Funding
No funding has been provided for this study.
Ethical approval
This survey did not require formal ethical approval with a practice dedicated to adult reconstruction.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kort, N.P., Barrena, E.G., Bédard, M. et al. Recommendations for resuming elective hip and knee arthroplasty in the setting of the SARS-CoV-2 pandemic: the European Hip Society and European Knee Associates Survey of Members. Knee Surg Sports Traumatol Arthrosc 28, 2723–2729 (2020). https://doi.org/10.1007/s00167-020-06212-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06212-0