Abstract
Purpose
To determine whether articular cartilage damage noted at the time of primary anterior cruciate ligament reconstruction (ACLR) affects the likelihood of achieving ≥ 90% symmetry for isokinetic extension strength at 6 months after surgery or risk of recurrent ACL injury.
Methods
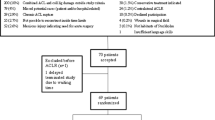
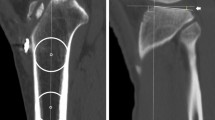
Five hundred and eight patients underwent primary ACLR and diagnostic arthroscopy. All identified cartilage lesions were graded using the Outerbridge system. All patients underwent isokinetic strength testing. The association between cartilage Outerbridge grade and a ≥ 90% Limb Symmetry Index (LSI) and recurrent ACL injury risk at mean 38.7 month follow-up (SD 31.8) was evaluated via multivariate regression analysis.
Results
Grade 2 or higher damage was present in 394 (77.5%) of patients, grade 3 or higher in 143 (28.1%) and grade 4 in 83 (16.4%) at time of ACLR. Ipsilateral ACLR graft rupture occurred in 31 (6.1%) of patients. Contralateral ACL injury occurred in 19 (3.7%). Patients with grade 2 or higher damage were significantly less likely to meet an LSI goal of ≥ 90% for fast (300°/s) isokinetic extension. There was no association with slow isokinetic extension. Cartilage lesion severity at or beyond grade 2 had a similar effect on isokinetic testing results regardless of compartment involvement or performance of microfracture. Patients with grade 2–4 cartilage damage were less likely to sustain a second ipsilateral ACL injury or a contralateral native ACL injury.
Conclusions
Cartilage damage seen at time of ACL reconstruction is common and associated with lower likelihood of achieving ≥ 90% symmetry for isokinetic extension strength at 6 months after surgery. However, lower recurrent ACL injury rates are seen in patients with concurrent cartilage damage. These data may inform future clinical decisions regarding operative managment of recurrent ACL injuries.
Level of evidence
III.

Similar content being viewed by others
References
Anandacoomarasamy A, Smith G, Leibman S, Caterson I, Giuffre B, Fransen M et al (2009) Cartilage defects are associated with physical disability in obese adults. Rheumatology (Oxford) 48:1290–1293
Cinque ME, Chahla J, Mitchell JJ, Moatshe G, Pogorzelski J, Murphy CP et al (2018) Influence of meniscal and chondral lesions on patient-reported outcomes after primary anterior cruciate ligament reconstruction at 2-year follow-up. Orthop J Sports Med 6:2325967117754189
Ebert JR, Smith A, Edwards PK, Ackland TR (2014) The progression of isokinetic knee strength after matrix-induced autologous chondrocyte implantation: implications for rehabilitation and return to activity. J Sport Rehabil 23:244–258
Eitzen I, Grindem H, Nilstad A, Moksnes H, Risberg MA (2016) Quantifying quadriceps muscle strength in patients with ACL injury, focal cartilage lesions, and degenerative meniscus tears: differences and clinical implications. Orthop J Sports Med 4:2325967116667717
Filardo G, de Caro F, Andriolo L, Kon E, Zaffagnini S, Marcacci M (2017) Do cartilage lesions affect the clinical outcome of anterior cruciate ligament reconstruction? A systematic review. Knee Surg Sports Traumatol Arthrosc 25:3061–3075
Greig M, Naylor J (2017) The efficacy of angle-matched isokinetic knee flexor and extensor strength parameters in predicting agility test performance. Int J Sports Phys Ther 12:728–736
Hamrin Senorski E, Svantesson E, Baldari A, Ayeni OR, Engebretsen L, Franceschi F et al (2018) Factors that affect patient reported outcome after anterior cruciate ligament reconstruction—a systematic review of the scandinavian knee ligament registers. Br J Sports Med 53:410–417
Heir S, Nerhus TK, Røtterud JH, Løken S, Ekeland A, Engebretsen L et al (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38:231–237
Hirschmüller A, Andres T, Schoch W, Baur H, Konstantinidis L, Südkamp NP et al (2017) Quadriceps strength in patients with isolated cartilage defects of the knee: results of isokinetic strength measurements and their correlation with clinical and functional results. Orthop J Sports Med 5:2325967117703726
Kreuz PC, Müller S, Freymann U, Erggelet C, Niemeyer P, Kaps C et al (2011) Repair of focal cartilage defects with scaffold-assisted autologous chondrocyte grafts: clinical and biomechanical results 48 months after transplantation. Am J Sports Med 39:1697–1705
LaBella CR, Hennrikus W, Hewett TE (2014) Council on Sports Medicine and Fitness, and Section on Orthopaedics. Anterior cruciate ligament injuries: diagnosis, treatment, and prevention. Pediatrics 133:e1437–e1450
Løken S, Ludvigsen TC, Høysveen T, Holm I, Engebretsen L, Reinholt FP (2009) Autologous chondrocyte implantation to repair knee cartilage injury: ultrastructural evaluation at 2 years and long-term follow-up including muscle strength measurements. Knee Surg Sports Traumatol Arthrosc 17:1278–1288
Maldonado G, Greenland S (1993) Simulation study of confounder-selection strategies. Am J Epidemiol 138:923–936
Mickey RM, Greenland S (1989) The impact of confounder selection criteria on effect estimation. Am J Epidemiol 129:125–137
Outerbridge R (1961) The etiology of chondromalacia patellae. J Bone Jt Surg Br 43-B:752–757
Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE (2012) Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med 22:116–121
Røtterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Arøen A (2013) Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: a nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med 41:535–543
Shelbourne KD, Jari S, Gray T (2003) Outcome of untreated traumatic articular cartilage defects of the knee: a natural history study. J Bone Jt Surg Am 85-A(Suppl 2):8–16
Snaebjörnsson T, Hamrin Senorski E, Sundemo D, Svantesson E, Westin O, Musahl V et al (2017) Adolescents and female patients are at increased risk for contralateral anterior cruciate ligament reconstruction: a cohort study from the Swedish National Knee Ligament Register based on 17,682 patients. Knee Surg Sports Traumatol Arthrosc 25:3938–3944
Thrush C, Porter TJ, Devitt BM (2018) No evidence for the most appropriate postoperative rehabilitation protocol following anterior cruciate ligament reconstruction with concomitant articular cartilage lesions: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:1065–1073
Webster KE, Feller JA, Leigh WB, Richmond AK (2014) Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 42:641–647
Wondrasch B, Arøen A, Røtterud JH, Høysveen T, Bølstad K, Risberg MA (2013) The feasibility of a 3-month active rehabilitation program for patients with knee full-thickness articular cartilage lesions: the Oslo Cartilage Active Rehabilitation and Education Study. J Orthop Sports Phys Ther 43:310–324
Wright RW, Haas AK, Anderson J, Calabrese G, Cavanaugh J, Hewett TE et al (2015) Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health 7:239–243
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors received no funding for this study and report no conflicts of interest.
Ethical approval
This project was approved by the Biomedical Institutional Research Board of The Ohio State University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Everhart, J.S., DiBartola, A.C., Swank, K. et al. Cartilage damage at the time of anterior cruciate ligament reconstruction is associated with weaker quadriceps function and lower risk of future ACL injury. Knee Surg Sports Traumatol Arthrosc 28, 576–583 (2020). https://doi.org/10.1007/s00167-019-05739-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05739-1