Abstract
Purpose
To investigate, whether cartilage repair surgery for focal osteochondral defects at the knee results in less degenerative changes over 6 years in a MR imaging follow-up than morphologically initially identical defects in non-operated control subjects from the osteoarthritis initiative (OAI).
Methods
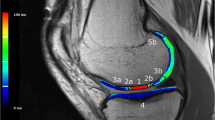
A total of 32 individuals received baseline and follow-up MRI. In n = 16 patients with cartilage repair [osteochondral autograft transfer system (OATS), n = 12; spongiosa-augmented matrix-associated autologous chondrocyte implantation (MACI), n = 4] MRI was performed preoperatively and after 5.7 ± 2.3 year follow-up. Baseline MRIs of non-operated subjects from the OAI were screened for initially identical cartilage defects (n = 16). Morphological knee abnormalities were assessed using WORMS, AMADEUS and MOCART scores. A sagittal 2D MSME sequence was implemented for quantitative cartilage T2 relaxation time measurements in all (0, 2, 4, 6 and 8-years) follow-ups from the OAI and in the postoperative MRI protocol.
Results
For both groups, focal osteochondral defects were located at the femoral condyle in 8/16 cases (5 medial, 3 lateral) and at the patella in 8/16 cases. At baseline, the mean cartilage defect size ± SD was 1.4 ± 1.3 cm2 for the control group and 1.3 ± 1.2 cm2 for the cartilage repair group (n.s.). WORMS scores were not significantly different between the cartilage repair group and the control group at baseline [mean difference ± SEM (95%CI); 0.5 ± 2.5 (− 4.7, 5.7), n.s.]. During identical follow-up times, the progression of total WORMS scores [19.9 ± 2.3 (15.0, 24.9), P < 0.001] and of cartilage defects scores in the affected (P < 0.001) and in the opposing (P = 0.029) compartment was significantly more severe in non-operated individuals (P < 0.05). In non-operated subjects, T2 values increased continuously from baseline to the 8-year follow-up (P = 0.001).
Conclusions
Patients with cartilage repair showed less progression of degenerative MRI changes at 6-year follow-up than a control cohort from the OAI with initially identical osteochondral defects. Patients with focal cartilage defects may profit from cartilage repair surgery since it may prevent progression of early osteoarthritis at the knee joint.
Level of evidence
Prognostic study, Level II.





Similar content being viewed by others
References
Agneskirchner JD, Brucker P, Burkart A, Imhoff AB (2002) Large osteochondral defects of the femoral condyle: press-fit transplantation of the posterior femoral condyle (MEGA-OATS). Knee Surg Sports Traumatol Arthrosc 10:160–168
Baum T, Joseph GB, Karampinos DC, Jungmann PM, Link TM, Bauer JS (2013) Cartilage and meniscal T2 relaxation time as non-invasive biomarker for knee osteoarthritis and cartilage repair procedures. Osteoarthr Cartil 21:1474–1484
Benthien JP, Schwaninger M, Behrens P (2011) We do not have evidence based methods for the treatment of cartilage defects in the knee. Knee Surg Sports Traumatol Arthrosc 19:543–552
Bentley G, Biant LC, Vijayan S, Macmull S, Skinner JA, Carrington RW (2012) Minimum ten-year results of a prospective randomised study of autologous chondrocyte implantation versus mosaicplasty for symptomatic articular cartilage lesions of the knee. J Bone Jt Surg Br 94:504–509
Brittberg M, Recker D, Ilgenfritz J, Saris DBF, Group SES (2018) Matrix-applied characterized autologous cultured chondrocytes versus microfracture: five-year follow-up of a prospective randomized trial. Am J Sports Med 46:1343–1351
Burstein D, Gray M (2003) New MRI techniques for imaging cartilage. J Bone Jt Surg Am 85-A(Suppl) 2:70–77
Cicuttini F, Ding C, Wluka A, Davis S, Ebeling PR, Jones G (2005) Association of cartilage defects with loss of knee cartilage in healthy, middle-age adults: a prospective study. Arthritis Rheum 52:2033–2039
Conaghan PG, Tennant A, Peterfy CG, Woodworth T, Stevens R, Guermazi A et al (2006) Examining a whole-organ magnetic resonance imaging scoring system for osteoarthritis of the knee using Rasch analysis. Osteoarthr Cartil 14(Suppl A):A116–121
Crawford DC, DeBerardino TM, Williams RJ 3rd (2012) NeoCart, an autologous cartilage tissue implant, compared with microfracture for treatment of distal femoral cartilage lesions: an FDA phase-II prospective, randomized clinical trial after two years. J Bone Jt Surg Am 94:979–989
Crema MD, Roemer FW, Marra MD, Burstein D, Gold GE, Eckstein F et al (2011) Articular cartilage in the knee: current MR imaging techniques and applications in clinical practice and research. Radiographics 31:37–61
Dardzinski BJ, Mosher TJ, Li S, Van Slyke MA, Smith MB (1997) Spatial variation of T2 in human articular cartilage. Radiology 205:546–550
de Windt TS, Welsch GH, Brittberg M, Vonk LA, Marlovits S, Trattnig S et al (2013) Is magnetic resonance imaging reliable in predicting clinical outcome after articular cartilage repair of the knee? A systematic review and meta-analysis. Am J Sports Med 41:1695–1702
Dell’accio F, Vincent TL (2010) Joint surface defects: clinical course and cellular response in spontaneous and experimental lesions. Eur Cell Mater 20:210–217
DiBartola AC, Everhart JS, Magnussen RA, Carey JL, Brophy RH, Schmitt LC et al (2016) Correlation between histological outcome and surgical cartilage repair technique in the knee: a meta-analysis. Knee 23:344–349
Domayer SE, Welsch GH, Dorotka R, Mamisch TC, Marlovits S, Szomolanyi P et al (2008) MRI monitoring of cartilage repair in the knee: a review. Semin Musculoskelet Radiol 12:302–317
Dozin B, Malpeli M, Cancedda R, Bruzzi P, Calcagno S, Molfetta L et al (2005) Comparative evaluation of autologous chondrocyte implantation and mosaicplasty: a multicentered randomized clinical trial. Clin J Sport Med 15:220–226
Ebert JR, Robertson WB, Woodhouse J, Fallon M, Zheng MH, Ackland T et al (2011) Clinical and magnetic resonance imaging-based outcomes to 5 years after matrix-induced autologous chondrocyte implantation to address articular cartilage defects in the knee. Am J Sports Med 39:753–763
Eckstein F, Kunz M, Hudelmaier M, Jackson R, Yu J, Eaton CB et al (2007) Impact of coil design on the contrast-to-noise ratio, precision, and consistency of quantitative cartilage morphometry at 3 T: a pilot study for the osteoarthritis initiative. Magn Reson Med 57:448–454
Gersing AS, Feuerriegel G, Holwein C, Suchowierski J, Karampinos DC, Haller B et al (2018) T2-relaxation time of cartilage repair tissue is associated with bone remodeling after spongiosa-augmented matrix-associated autologous chondrocyte implantation. Osteoarthr Cartil. https://doi.org/10.1016/j.joca.2018.08.023
Gomoll AH, Gillogly SD, Cole BJ, Farr J, Arnold R, Hussey K et al (2014) Autologous chondrocyte implantation in the patella: a multicenter experience. Am J Sports Med 42:1074–1081
Hafezi-Nejad N, Zikria B, Eng J, Carrino JA, Demehri S (2015) Predictive value of semi-quantitative MRI-based scoring systems for future knee replacement: data from the osteoarthritis initiative. Skelet Radiol 44:1655–1662
Harmelink KEM, Zeegers A, Hullegie W, Hoogeboom TJ, Nijhuis-van der Sanden MWG, Staal JB (2017) Are there prognostic factors for one-year outcome after total knee arthroplasty? A systematic review. J Arthroplast 32:3840–3853 e3841
Horas U, Pelinkovic D, Herr G, Aigner T, Schnettler R (2003) Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. A prospective, comparative trial. J Bone Jt Surg Am 85-A:185–192
Hovis KK, Stehling C, Souza RB, Haughom BD, Baum T, Nevitt M et al (2011) Physical activity is associated with magnetic resonance imaging-based knee cartilage T2 measurements in asymptomatic subjects with and those without osteoarthritis risk factors. Arthritis Rheum 63:2248–2256
Hustedt JW, Goltzer O, Bohl DD, Fraser JF, Lara NJ, Spangehl MJ (2017) Calculating the cost and risk of comorbidities in total joint arthroplasty in the United States. J Arthroplast 32:355–361 e351
Jungmann PM, Baum T, Bauer JS, Karampinos DC, Erdle B, Link TM et al (2014) Cartilage repair surgery: outcome evaluation by using noninvasive cartilage biomarkers based on quantitative MRI techniques? Biomed Res Int 2014:840170
Jungmann PM, Baum T, Nevitt MC, Nardo L, Gersing AS, Lane NE et al (2016) Degeneration in ACL injured knees with and without reconstruction in relation to muscle size and fat content-data from the osteoarthritis initiative. PLoS One 11:e0166865
Jungmann PM, Brucker PU, Baum T, Link TM, Foerschner F, Minzlaff P et al (2015) Bilateral cartilage T2 mapping 9 years after Mega-OATS implantation at the knee: a quantitative 3T MRI study. Osteoarthr Cartil 23:2119–2128
Jungmann PM, Kraus MS, Nardo L, Liebl H, Alizai H, Joseph GB et al (2013) T(2) relaxation time measurements are limited in monitoring progression, once advanced cartilage defects at the knee occur: longitudinal data from the osteoarthritis initiative. J Magn Reson Imaging 38:1415–1424
Jungmann PM, Nevitt MC, Baum T, Liebl H, Nardo L, Liu F et al (2015) Relationship of unilateral total hip arthroplasty (THA) to contralateral and ipsilateral knee joint degeneration—a longitudinal 3T MRI study from the osteoarthritis initiative (OAI). Osteoarthr Cartil 23:1144–1153
Jungmann PM, Welsch GH, Brittberg M, Trattnig S, Braun S, Imhoff AB et al (2017) Magnetic resonance imaging score and classification system (AMADEUS) for assessment of preoperative cartilage defect severity. Cartilage 8:272–282
Lahner M, Ull C, Hagen M, von Schulze Pellengahr C, Daniilidis K, von Engelhardt LV et al (2018) Cartilage surgery in overweight patients: clinical and MRI results after the autologous matrix-induced chondrogenesis procedure. Biomed Res Int 2018:6363245
Lansdown DA, Wang K, Cotter E, Davey A, Cole BJ (2018) Relationship between quantitative MRI biomarkers and patient-reported outcome measures after cartilage repair surgery: a systematic review. Orthop J Sports Med 6:2325967118765448
Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA (2017) Knee osteoarthritis: a primer. Perm J 21
Liebl H, Joseph G, Nevitt MC, Singh N, Heilmeier U, Subburaj K et al (2015) Early T2 changes predict onset of radiographic knee osteoarthritis: data from the osteoarthritis initiative. Ann Rheum Dis 74:1353–1359
Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N et al (2003) Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology 226:373–381
Maier CF, Tan SG, Hariharan H, Potter HG (2003) T2 quantitation of articular cartilage at 1.5 T. J Magn Reson Imaging 17:358–364
McCarthy HS, McCall IW, Williams JM, Mennan C, Dugard MN, Richardson JB et al (2018) Magnetic resonance imaging parameters at 1 year correlate with clinical outcomes up to 17 years after autologous chondrocyte implantation. Orthop J Sports Med 6:2325967118788280
Minzlaff P, Feucht MJ, Saier T, Schuster T, Braun S, Imhoff AB et al (2013) Osteochondral autologous transfer combined with valgus high tibial osteotomy: long-term results and survivorship analysis. Am J Sports Med 41:2325–2332
Mosher TJ, Zhang Z, Reddy R, Boudhar S, Milestone BN, Morrison WB et al (2011) Knee articular cartilage damage in osteoarthritis: analysis of MR image biomarker reproducibility in ACRIN-PA 4001 multicenter trial. Radiology 258:832–842
Niemeyer P, Albrecht D, Andereya S, Angele P, Ateschrang A, Aurich M et al (2016) Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: a guideline by the working group “clinical tissue regeneration” of the German Society of Orthopaedics and Trauma (DGOU). Knee 23:426–435
Niemeyer P, Andereya S, Angele P, Ateschrang A, Aurich M, Baumann M et al (2013) Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: a guideline by the working group “tissue regeneration” of the German Society of Orthopaedic Surgery and Traumatology (DGOU). Z Orthop Unfall 151:38–47
Niemeyer P, Steinwachs M, Erggelet C, Kreuz PC, Kraft N, Kostler W et al (2008) Autologous chondrocyte implantation for the treatment of retropatellar cartilage defects: clinical results referred to defect localisation. Arch Orthop Trauma Surg 128:1223–1231
Ochs BG, Muller-Horvat C, Albrecht D, Schewe B, Weise K, Aicher WK et al (2011) Remodeling of articular cartilage and subchondral bone after bone grafting and matrix-associated autologous chondrocyte implantation for osteochondritis dissecans of the knee. Am J Sports Med 39:764–773
Oei EHG, Wick MC, Muller-Lutz A, Schleich C, Miese FR (2018) Cartilage imaging: techniques and developments. Semin Musculoskelet Radiol 22:245–260
Ossendorff R, Franke K, Erdle B, Uhl M, Sudkamp NP, Salzmann GM (2018) Clinical and radiographical ten years long-term outcome of microfracture vs. autologous chondrocyte implantation: a matched-pair analysis. Int Orthop. https://doi.org/10.1007/s00264-018-4025-5
Pan J, Pialat JB, Joseph T, Kuo D, Joseph GB, Nevitt MC et al (2011) Knee cartilage T2 characteristics and evolution in relation to morphologic abnormalities detected at 3-T MR imaging: a longitudinal study of the normal control cohort from the osteoarthritis initiative. Radiology 261:507–515
Peterfy CG, Schneider E, Nevitt M (2008) The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthr Cartil 16:1433–1441
Riboh JC, Cvetanovich GL, Cole BJ, Yanke AB (2017) Comparative efficacy of cartilage repair procedures in the knee: a network meta-analysis. Knee Surg Sports Traumatol Arthrosc 25:3786–3799
Roos EM, Engelhart L, Ranstam J, Anderson AF, Irrgang JJ, Marx RG et al (2011) ICRS recommendation document: patient-reported outcome instruments for use in patients with articular cartilage defects. Cartilage 2:122–136
Salzmann GM, Niemeyer P, Steinwachs M, Kreuz PC, Sudkamp NP, Mayr HO (2011) Cartilage repair approach and treatment characteristics across the knee joint: a European survey. Arch Orthop Trauma Surg 131:283–291
Salzmann GM, Paul J, Bauer JS, Woertler K, Sauerschnig M, Landwehr S et al (2009) T2 assessment and clinical outcome following autologous matrix-assisted chondrocyte and osteochondral autograft transplantation. Osteoarthr Cartil 17:1576–1582
Smith HE, Mosher TJ, Dardzinski BJ, Collins BG, Collins CM, Yang QX et al (2001) Spatial variation in cartilage T2 of the knee. J Magn Reson Imaging 14:50–55
Stehling C, Liebl H, Krug R, Lane NE, Nevitt MC, Lynch J et al (2010) Patellar cartilage: T2 values and morphologic abnormalities at 3.0-T MR imaging in relation to physical activity in asymptomatic subjects from the osteoarthritis initiative. Radiology 254:509–520
Vanlauwe J, Saris DB, Victor J, Almqvist KF, Bellemans J, Luyten FP et al (2011) Five-year outcome of characterized chondrocyte implantation versus microfracture for symptomatic cartilage defects of the knee: early treatment matters. Am J Sports Med 39:2566–2574
Vijayan S, Bartlett W, Bentley G, Carrington RW, Skinner JA, Pollock RC et al (2012) Autologous chondrocyte implantation for osteochondral lesions in the knee using a bilayer collagen membrane and bone graft: a two- to eight-year follow-up study. J Bone Jt Surg Br 94:488–492
Funding
The study was funded by the B. Braun Stiftung (BBST-D-17-00070R1). The study was supported by the Osteoarthritis Initiative, a public–private partnership comprising 5 NIH contracts (National Institute of Arthritis and Musculoskeletal and Skin Diseases contracts N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, and N01-AR-2-2262), with research conducted by the Osteoarthritis Initiative Study Investigators. The study was also funded in part by the Intramural Research Program of the National Institute on Aging, NIH. Private funding partners include Merck Research, Novartis Pharmaceuticals, GlaxoSmithKline, and Pfizer; the private sector funding for the Osteoarthritis Initiative is managed by the Foundation for the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All authors (PMJ, ASG, FB, CH, SB, JN, JZ, FCH, ABI, EJR, TML) have made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data. All authors (PMJ, ASG, FB, CH, SB, JN, JZ, FCH, ABI, EJR, TML) have been involved in drafting the manuscript or revising it critically for important intellectual content. All authors (PMJ, ASG, FB, CH, SB, JN, JZ, FCH, ABI, EJR, TML) have given final approval of the version to be published. All authors (PMJ, ASG, FB, CH, SB, JN, JZ, FCH, ABI, EJR, TML) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest for any of the authors.
Ethical approval
The study was approved by the local Institutional Review Boards (Ethikkommission Technical University of Munich). The OAI study protocol, amendments, and informed consent documentation including analysis plans were reviewed and approved by the local institutional review boards. Data used in the preparation of this manuscript were obtained from the OAI database, which is available for public access at http://www.oai.ucsf.edu/. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Informed consent
All subjects gave written informed consent prior to participation in the study.
Rights and permissions
About this article
Cite this article
Jungmann, P.M., Gersing, A.S., Baumann, F. et al. Cartilage repair surgery prevents progression of knee degeneration. Knee Surg Sports Traumatol Arthrosc 27, 3001–3013 (2019). https://doi.org/10.1007/s00167-018-5321-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5321-8