Abstract
Purpose
Total knee arthroplasty is a successful procedure in treating subjects with end-stage knee osteoarthritis. The objective of this matched study was to evaluate subjective patient satisfaction and clinical and radiological outcomes in two groups of patients undergoing primary TKA using an identical third-generation design with different conformity in the polyethylene insert.
Methods
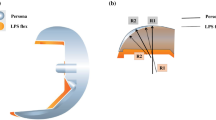
One hundred consecutive patients undergoing TKA because of knee osteoarthritis were randomized in two matched groups. Group A included 50 Posterior-Stabilized (PS) implants, while group B included 50 Medially Congruent (MC) implants. The surgical technique was identical: gap balancing in extension and measured resection in flexion; cruciate ligaments were always removed; the coronal alignment followed the mechanical axis and the tibial slope was set at 3° in the PS group and 5° in the MC. Oxford Knee Score (OKS) and Knee Society Score (KSS) were assessed preoperatively and at 2 year minimum follow-up. Two-sample T test statistical analysis was performed.
Results
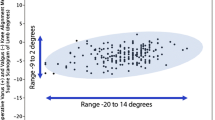
All patients were available at final follow-up: there were no preoperative statistical differences between the two groups in the average preoperative ROM (PS 112°, MC 108°; n.s.), average preoperative KSS (PS 64.4, MC 63.7; n.s.), average preoperative OKS (PS 19.6; MC 19.0; n.s.), and average BMI (PS 34.40, MC 34.60; n.s.). At final follow-up, there were no statistical differences between the two groups in the average OKS (PS 40,5; MC 41.1; n.s.) and in the average KSS (PS 161,5, MC 165,7; n.s.). We found a statistically but not clinically significant difference at final ROM: the average maximum active flexion was 120° in the PS group and 123° in the MC group (s.s.).
Conclusion
This study evaluated two biomechanically different polyethylene inserts in the same TKA design, showing that reducing the level of intra-articular conformity had minimal effects on PROMs and objective short-term clinical results but a potentially beneficial effect on ROM. This study suggests that, once a satisfactory intra-operative stability is obtained, the minimal level of constraint should be used.
Level of evidence
III.

Similar content being viewed by others
References
Chatterji U, Ashworth MJ, Lewis PL, Dobson PJ (2005) Effect of total knee arthroplasty on recreational and sporting activity. ANZ J Surg 75:405–408
Gibon GE, Goodman MJ, Goodman SB (2017) Patient satisfaction after total knee arthroplasty. Orthop Clin 48(4):421–431
Dennis DA, Komistek RD, Hoff WA et al (1996) In vivo knee kinematics derived using an inverse perspective technique. Clin Orthop Relat Res 331:107–117
Dennis D, Komistek R, Mahfouz M, Haas B, Stiehl J (2003) Conventry award paper: multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res 416:37–57
Dennis DA, Mahfouz MR, Komistek RD et al (2005) In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech 38(2):241–253
Ginsel BL, Banks S, Verdonschot N et al (2009) Improving maximum flexion with a posterior cruciate retaining total knee arthroplasty: a fluoroscopic study. Acta Orthop Belg 75:801–807
Grieco TF, Sharma A, Komistek RD, Cates HE (2016) Single versus multiple-radii cruciate-retaining total knee arthroplasty: an in-vivo mobile fluoroscopy study. J Arthroplasty 31:694–701
Hoffman AA, Tkach TK, Evanich CJ et al (2000) Posterior stabilization in total knee arthroplasty with use of an ultracongruent polyethylene insert. J Arthroplasty 15:576–583
Incavo SJ, Mullins ER, Coughlin KM, Banks S, Banks A, Beynnon BD (2004) Tibiofemoral kinematic analysis of kneeling after total knee arthroplasty. J Arthroplasty 19(7):906–910
Indelli PF, Marcucci M, Graceffa A, Charlton S, Latella L (2014) Primary posterior stabilized total knee arthroplasty: analysis of different instrumentation. J Orthop Surg Res 19(9):54–58
Indelli PF, Graceffa A, Payne B, Baldini A, Pipino G, Marcucci M (2015) Relationship between tibial baseplate design and rotational alignment landmarks in primary total knee arthroplasty. Arthritis 4:1–8
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–24
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15(8) 970–973
Iwaki H, Pinskerova V, Freeman MAR (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 82(8):1189–1195
Joglekar S, Gioe TJ, Yoon P, Schwartz MH (2012) Gait analysis comparison of cruciate retaining and substituting TKA following PCL sacrifice. Knee 19(4):279–285
Kleinbart FA, Bryk E, Evangelista J, Scott WN, Vigorita VJ (1996) Histologic comparison of posterior cruciate ligaments from arthritic and age-matched knee specimens. J Arthroplasty 11(6):726–731
Komistek RD, Dennis DA, Mahfouz M (2003) In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res 410:69–81
Leszko F, Hovinga KR, Lerner AL et al (2011) In vivo normal knee kinematics: is ethnicity or gender an influencing factor? Clin Orthop Relat Res 469(1):95–106
Li G, Zayontz S, DeFrate LE et al (2004) Kinematics of the knee at high flexion angles: an in vitro investigation. J Orthop Res 22(1):90–95
Lombardi AV Jr., Mallory TH, Waterman RA, Eberle RW (1995) Intercondylar distal femoral fracture. An unreported complication of posterior-stabilized total knee arthroplasty. J Arthroplasty 10(5):643–650
Lotke PA, Lonner JH (2009) Knee arthroplasty, 3rd edn. Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia
Lützner J, Firmbach FP, Lützner C et al (2015) Similar stability and range of motion between cruciate-retaining and cruciate-substituting ultracongruent insert total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(6):1638–1643
Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB (2005) Does total knee replacement restore normal knee function? Clin Orthop Relat Res 431:157–165
Parcells BW, Tria AJ Jr (2016) The cruciate ligaments in total knee arthroplasty. Am J Orthop (Belle Mead NJ) 45(4):153–160
Pope MH (2005) Giovanni Alfonso Borelli: the father of biomechanics. Spine 5(30):2350–2355
Rajgopal A, Aggarwal K, Khurana A, Rao A, Vasdev A, Pandit H (2017) Gait parameters and functional outcomes after total knee arthroplasty using persona knee system with cruciate retaining and ultracongruent knee inserts. J Arthroplasty 32(1):87–91
Sabatini L, Risitano S, Parisi G, Tosto F, Indelli PF, Atzori F, Massè A (2018) Medial pivot in total knee arthroplasty: literature review and our first experience. Clin Med Insights Arthritis Musculoskelet Disord. https://doi.org/10.1177/1179544117751431
Schulze A, Scharf HP (2013) Satisfaction after total knee arthroplasty. Comparison of 1990–1999 with 2000–2012. Orthopade 42(10):858–865
Steckelberg RC1, Funck N, Kim TE, Walters TL, Lochbaum GM, Memtsoudis SG, Giori NJ, Indelli PF, Mariano ER (2017) Adherence to a multimodal analgesic clinical pathway: a within-group comparison of staged bilateral knee arthroplasty patients. Reg Anesth Pain Med 42(3):368–371
Stiehl JB, Komistek RD, Dennis DA et al (1995) Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br 77(6):884–889
Scott G, Iman MA, Eifort A et al (2016) Can a total knee arthroplasty be both rotationally unconstrained and anteroposteriorly stabilized ? A pulsed fluoroscopic investigation. Bone Joint Res 5:80–86
Yoshiya S, Matsui N, Komistek RD et al (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty 20(6):777–783
Funding
The Authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Authors certify that they have non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
Each author confirms that this manuscript meets the highest ethical standards, including proper statistical investigations and thorough ethical reviews by the data owning organisations.
Rights and permissions
About this article
Cite this article
Indelli, P.F., Risitano, S., Hall, K.E. et al. Effect of polyethylene conformity on total knee arthroplasty early clinical outcomes. Knee Surg Sports Traumatol Arthrosc 27, 1028–1034 (2019). https://doi.org/10.1007/s00167-018-5170-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5170-5