Abstract
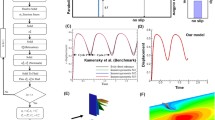
We present direct numerical simulations for the pathophysiology of hypertrophic cardiomyopathy of the left ventricle of the human heart. This cardiovascular disorder manifests itself through systolic anterior motion (SAM), a drift of the mitral leaflets towards the aortic subvalvular region, sometimes causing ventricular obstruction during systole. This pathology is induced by a combination of factors, including a thickening of the interventricular septum and an elongation of the mitral valve leaflets: we perform a full parametric study to assess their effect on the disease. From our results we observe that SAM occurs when elongated leaflets, hypertrophic ventricles and strong ejection fraction are present at the same time. In contrast, a physiological ventricle with elongated leaflets, an hypertrophic ventricle with physiological leaflets or diseased ventricle and leaflets with a weak ejection fraction do not produce SAM. After verifying that the numerical results are consistent and in agreement with the clinical data from the literature, we virtually test the two standard surgical procedures, leaflet plication and septal myectomy, adopted for the surgical treatment of SAM. For all the considered cases we obtain quantitative confirmation for the reliability of the intraventricular subvalvular pressure drop (or subvalvular pressure gradient for the medical community) as diagnostic indicator of the systolic anterior motion: when this quantity attains the value of 30 mmHg, SAM of the mitral leaflets is observed, while when this threshold is exceeded the SAM becomes obstructive. On the other hand, in all cases for which SAM is not observed the above pressure drop is always below the threshold.















Similar content being viewed by others
References
Boyang, S., et al.: Cardiac MRI based numerical modeling of left ventricular fluid dynamics with mitral valve incorporated. J. Biomech. 26, 225–230 (2016)
de Tullio, M.D., Pascazio, G.: A moving least-squares immersed boundary method for simulating the fluid–structure interaction of elastic bodies with arbitrary thickness. J. Comput. Phys. 235, 201–225 (2016)
Donato, M.D., et al.: Left ventricular geometry in normal and post-anterior myocardial infarction patients: sphericity index and ‘new’ conicity index comparisons. Eur. J. Cardiothorac. Surg. 29, 225–230 (2006)
Fadlun, E.A., Verzicco, R., Orlandi, P., Mohd-Yosuf, J.: Combined immersed-boundary finite-difference methods for three-dimensional complex flow simulations. J. Comput. Phys. 161, 35–60 (2000)
Feins, E.N., Yamauchi, H., Marx, G.R., Freudenthal, F.P., Liu, H., del Nido, P.J., Vasilyev, N.V.: Repair of posterior mitral valve prolapse with a novel leaflet plication clip in an animal model. J. Thorac. Cardiovasc. Surg. 147(2), 783–791 (2014)
Gregor, P., Curila, K.: Medical treatment of hypertrophic cardiomyopathy—What do we know about it today? Cor et Vasa 57, e219–e224 (2015)
Koester, M.: A review of sudden cardiac death in young athletes and strategies for preparticipation cardiovascular screening. J. Athlet. Train. 36(2), 197–204 (2001)
Maron, B.J., Gardin, J.M., Flack, J..M..e.a: Assessment of the prevalence of hypertrophic cardiomyopathy in a general population of young adults: echocardiographic analysis of 4111 subjects in the cardia study. Circulation 92, 785–944 (1995)
Maron, B.J., Ommen, S.R., Semsarian, C., Spirito, P., Olivotto, I., Maron, M.S.: Hypertrophic cardiomyopathy. Present and future, with translation into contemporary cardiovascular medicine. J. Am. Coll. Cardiol. 64, 83–99 (2014)
Meschini, V., de Tullio, M.D., Querzoli, G., Verzicco, R.: Flow structure in healthy and pathological left ventricles with natural and prosthetic mitral valves. J. Fluid Mech. 834, 271–307 (2018)
Meschini, V., de Tullio, M.D., Verzicco, R.: Effects of chordae tendineae on the flow in the left heart ventricle. Eur. Phys. J. E 41(2), 27 (2018)
Mittal, R., Seo, J.H., Vedula, V., Choi, Y.J., Liu, H., Huang, H.H., Jain, S., Younes, L., Abrahamd, T., George, R.T.: Computational modeling of cardiac hemodynamics: current status and future outlook. J. Comput. Phys. 305, 1065–1082 (2016)
Naidu, S.S.: Hypertrophic Cardiomyopathy. Springer, New York (2015)
Seo, J.H., et al.: Effect of the mitral valve on diastolic flow patterns. Phys. Fluids 26, 121901 (2016)
Sherrid, M., Balaram, S., Kim, B., Axel, L., Swistel, D.: The mitral valve in obstructive hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 67(15), 1846–1858 (2016)
Siginer, D.A., De Kee, D., Chhabra, R.P.: Advances in the Flow and Rheology of Non-Newtonian Fluids. Elsevier, Amsterdam (1999)
Spandan, V., Meschini, V., de Tullio, M.D., Querzoli, G., Lohse, D., Verzicco, R.: A parallel interaction potential approach for large scale simulations of deformable interfaces and membranes. J. Comput. Phys. 348, 567–590 (2017)
Stouffer, G., Runge, M., Patterson, C., Rossi, J.: Netter’s Cardiology. Theoretical Background and Biological/Biomedical Problems. Elsevier, New York (2018)
Suinesiaputra, A., et al.: Statistical shape modeling of the left ventricle: myocardial infarct classification challenge. J. Biomed. Health Inform. 22, 503–515 (2016)
Tanaka, M., Wada, S., Nakamura, M.: Computational Biomechanics, Theoretical Background and Biological/Biomedical Problems, vol. 3. Springer, New York (2012)
University, S.: https://web.stanford.edu
Van Gelder, A.: Approximate simulation of elastic membranes by triangulated spring meshes. J. Graph. Tools 3, 21–41 (1998)
Vanella, M., Balaras, E.: A moving-least-squares reconstruction for embedded-boundary formulations. J. Comput. Phys. 228(18), 6617–6628 (2009)
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Jeff D. Eldredge.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meschini, V., Mittal, R. & Verzicco, R. Systolic anterior motion in hypertrophic cardiomyopathy: a fluid–structure interaction computational model. Theor. Comput. Fluid Dyn. 35, 381–396 (2021). https://doi.org/10.1007/s00162-021-00564-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00162-021-00564-0