Abstract
Purpose
To study the incidence, predictors, and outcomes of diarrhea during the stay in the intensive care unit (ICU).
Methods
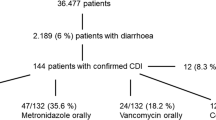
Prospective cohort of consecutive adults in the ICU for > 24 h during a 10-week period across 12 intensive care units (ICUs) internationally. The explored outcomes were: (1) incidence of diarrhea, (2) Clostridioides difficile-associated diarrhea (CDAD); (3) ICU and hospital length of stay (LOS) and mortality in patients with diarrhea. We fit generalized linear models to evaluate the predictors, management, morbidity and mortality associated with diarrhea.
Results
Among 1109 patients aged 61.4 (17.5) [mean (standard deviation)] years, 981(88.5%) were medical and 645 (58.2%) were mechanically ventilated. The incidence was 73.8% (818 patients, 73.8%, 95% confidence interval [CI] 71.1–76.6) using the definition of the World Health Organisation (WHO). Incidence varied across definitions (Bristol 53.5%, 95% CI 50.4–56.7; Bliss 37.7%, 95% CI 34.9–40.4). Of 99 patients with diarrhea undergoing CDAD testing, 23 tested positive (2.2% incidence, 95% CI 1.5–3.4). Independent predictors included enteral nutrition (RR 1.23, 95% CI 1.16–1.31, p < 0.001), antibiotic days (RR 1.02, 95% CI 1.02–1.03, p < 0.001), and suppositories (RR 1.14 95% CI 1.06–1.22, p < 0.001). Opiates decreased diarrhea risk (RR 0.76, 95% CI 0.68–0.86, p < 0.001). Diarrhea prompted management modifications (altered enteral nutrition or medications: RR 10.25, 95% CI 5.14–20.45, p < 0.001) or other consequences (fecal management device or CDAD testing: RR 6.16, 95% CI 3.4–11.17, p < 0.001). Diarrhea was associated with a longer time to discharge for ICU or hospital stay, but was not associated with hospital mortality.
Conclusion
Diarrhea is common, has several predictors, and prompts changes in patient care, is associated with longer time to discharge but not mortality.

Similar content being viewed by others
Data availability
Upon request.
Code availability
Not applicable.
References
Whelan K, Judd PA, Taylor MA (2004) Assessment of fecal output in patients receiving enteral tube feeding: validation of a novel chart. Eur J Clin Nutr 58:1030–1037
Ronan Thibault SG, Cler A, Delieuvin N, Heidegger CP, Pichard C (2013) Diarrhoea in the ICU: respective contribution of feeding and antibiotics. Crit Care 17:1–8
Reintam Blaser A, Malbrain ML, Starkopf J, Fruhwald S, Jakob SM, De Waele J, Braun JP, Poeze M, Spies C (2012) Gastrointestinal function in intensive care patients: terminology, definitions and management. Recommendations of the ESICM Working Group on Abdominal Problems. Intensive Care Med 38:384–394
Schiller LR, Pardi DS, Spiller R, Semrad CE, Surawicz CM, Giannella RA, Krejs GJ, Farthing MJ, Sellin JH (2014) Gastro 2013 APDW/WCOG Shanghai working party report: chronic diarrhea: definition, classification, diagnosis. J Gastroenterol Hepatol 29:6–25
Hay T, Bellomo R, Rechnitzer T, See E, Ali Abdelhamid Y, Deane AM (2019) Constipation, diarrhea, and prophylactic laxative bowel regimens in the critically ill: A systematic review and meta-analysis. J Crit Care. https://doi.org/10.1016/j.jcrc.2019.01.004
Organization WH (2005) The treatment of diarrhoea: a manual for physicians and other senior health workers: 1–43
Lewis SJ, Heaton KW (1997) Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol 32:920–924
Crobach MJ, Planche T, Eckert C, Barbut F, Terveer EM, Dekkers OM, Wilcox MH, Kuijper EJ (2016) European society of clinical microbiology and infectious diseases: update of the diagnostic guidance document for Clostridium difficile infection. Clin Microbiol Infect 22(Suppl 4):S63-81
Caroff DA, Edelstein PH, Hamilton K, Pegues DA, Program CDCPE (2014) The Bristol stool scale and its relationship to Clostridium difficile infection. J Clin Microbiol 52:3437–3439
Bliss D (2001) Reliability of a stool consistency classification system. Journal of WOCN 28:305–313
Zimmaro Bliss D, Dhamani KA, Savik K, Kirk K (2003) Tool to classify stool consistency: content validity and use by person of diverse cultures. Nurs Health Sci. https://doi.org/10.1046/j.1442-2018.2003.00145.x
Bishop S, Young H, Goldsmith D, Buldock D, Chin M, Bellomo R (2010) Bowel motions in critically ill patients:a pilot observational study. Criti Care Resuscit 12:182–185
Jack L, Coyer F, Courtney M, Venkatesh B (2010) Diarrhoea risk factors in enterally tube fed critically ill patients: a retrospective audit. Intensive Crit Care Nurs 26:327–334
Tirlapur N, Puthucheary ZA, Cooper JA, Sanders J, Coen PG, Moonesinghe SR, Wilson AP, Mythen MG, Montgomery HE (2016) Diarrhoea in the critically ill is common, associated with poor outcome, and rarely due to Clostridium difficile. Sci Rep 6:24691
Marcon AP, Amaral L, Carneiro V (2006) Nosocomial diarrhea in the intensive care unit. Braz J Infect Dis 10:384–389
Reintam A, Parm P, Redlich U, Tooding LM, Starkopf J, Kohler F, Spies C, Kern H (2006) Gastrointestinal failure in intensive care: a retrospective clinical study in three different intensive care units in Germany and Estonia. BMC Gastroenterol 6:19
Reintam A, Parm P, Kitus R, Kern H, Starkopf J (2009) Gastrointestinal symptoms in intensive care patients. Acta Anaesthesiol Scand 53:318–324
Taito S, Kawai Y, Liu K, Ariie T, Tsujimoto Y, Banno M, Kataoka Y (2019) Diarrhea and patient outcomes in the intensive care unit: systematic review and meta-analysis. J Crit Care 53:142–148
Dionne JC, Sullivan K, Mbuagbaw L, Takaoka A, Duan EH, Alhazzani W, Devlin JW, Duprey M, Moayyedi P, Armstrong D, Thabane L, Tsang JLY, Jaeschke R, Hamielec C, Karachi T, Cartin-Ceba R, Muscedere J, Alshahrani MSS, Cook DJ (2019) Diarrhoea: interventions, consequences and epidemiology in the intensive care unit (DICE-ICU): a protocol for a prospective multicentre cohort study. BMJ Open 9:e028237
Dionne JC, Sullivan K, Mbuagbaw L, Al-Hazzani W, Karachi T, Hamielec C, Tsang J, Takaoka A, Cook DJ (2016) Tu1068 diarrhea in the intensive care unit: epidemiology (The DICE Study). Gastroenterology. https://doi.org/10.1016/S0016-5085(16)32815-3
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2008) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61:344–349
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Cummings P (2009) Methods for estimating adjusted risk ratios. Stand Genomic Sci 9:175–196
StataCorp. (2019) Statistical Software: Release 16
Lindsay PJ, Rohailla S, Taggart LR, Lightfoot D, Havey T, Daneman N, Lowe C, Muller MP (2019) Antimicrobial stewardship and intensive care unit mortality: a systematic review. Clin Infect Dis 68:748–756
Pickens CI, Wunderink RG (2019) Principles and practice of antibiotic stewardship in the ICU. Chest 156:163–171
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, McCarthy MS, Davanos E, Rice TW, Cresci GA, Gervasio JM, Sacks GS, Roberts PR, Compher C, Society of Critical Care M, American Society for P, Enteral N (2016) Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: society of critical care medicine (SCCM) and american society for parenteral and enteral nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 40:159–211
Dionne JC, Campbell T, Janisse N, Zytaruk N, Saunders L, Heels-Ansdell D, Francois L, Johnstone J, Cook DJ (2020) Effect of fiber, osmolarity, and protein content of enteral nutrition on the development of diarrhea in critical illness. Gastroenterology. https://doi.org/10.1016/S0016-5085(20)33157-7
McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, Dubberke ER, Garey KW, Gould CV, Kelly C, Loo V, Shaklee Sammons J, Sandora TJ, Wilcox MH (2018) Clinical practice guidelines for clostridium difficile infection in adults and children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis 66:e1–e48
McDonald D, Ackermann G, Khailova L, Baird C, Heyland D, Kozar R, Lemieux M, Derenski K, King J, Vis-Kampen C, Knight R, Wischmeyer PE (2016) Extreme dysbiosis of the microbiome in critical illness. mSphere. https://doi.org/10.1128/mSphere.00199-16
Lankelma JM, van Vught LA, Belzer C, Schultz MJ, van der Poll T, de Vos WM, Wiersinga WJ (2017) Critically ill patients demonstrate large interpersonal variation in intestinal microbiota dysregulation: a pilot study. Intensive Care Med 43:59–68
Lamarche D, Johnstone J, Zytaruk N, Clarke F, Hand L, Loukov D, Szamosi JC, Rossi L, Schenck LP, Verschoor CP, McDonald E, Meade MO, Marshall JC, Bowdish DME, Karachi T, Heels-Ansdell D, Cook DJ, Surette MG, P Canadian Critical Care Trials G, Canadian Critical Care Translational Biology G (2018) Microbial dysbiosis and mortality during mechanical ventilation: a prospective observational study. Respir Res 19:245
Iapichino G, Callegari ML, Marzorati S, Cigada M, Corbella D, Ferrari S, Morelli L (2008) Impact of antibiotics on the gut microbiota of critically ill patients. J Med Microbiol 57:1007–1014
Iapichino G, Lankelma JM, Joost Wiersinga W (2017) Gut microbiota disruption in critically ill patients: discussion on “Critically ill patients demonstrate large interpersonal variation of intestinal microbiota dysregulation: a pilot study.” Intensive Care Med 43:718–719
Acknowledgements
We appreciate the data management assistance of Suzanne Duchesne and Nicole Zytaruk for this study. We also thank the research teams at each participating institution. A special tribute is dedicated to Wojciech Serednicki, co-author, who recently passed away.
DICE Investigators: Niagara Health System: J Tsang (Lead), Dimitra (Gina) Fleming, Susan O'Farrell, Brittany Young, Allison Brown, Helen Su, Robin Owen, Kathryn Lalonde, Kathleen Willis. Joseph Brant Hospital: P Lysecki (Lead), T Campbell. St. Joseph’s Healthcare Hamilton: D Cook (Lead), K Sullivan, A Takaoka. St. Joseph’s Hospital Toronto: R Cirone (Lead), K Kavikondala. Hamilton Health Sciences (General Site): C Hamielec (Lead), K Sullivan. Hamilton Health Sciences (Juravinski Site): T Karachi (Lead), K Sullivan. Northeastern University, Boston: J Devlin (Lead), M Duprey. Mayo Clinic, Phoenix: R Cartin-Ceba (Lead), H Raza, B Nokes. Kingston General Hospital: J Muscedere (Lead), M Hunt, I Georgescu. University of Dammam, A Alshahrani (Lead), LP Asonto. Brantford General Hospital, B Reeve (Lead), W Dechert. Jagellonian University Medical School, W Szczeklik (Lead), K Borowska.
Funding
Peer-review grants from the Hamilton Regional Medical Associates, Hamilton Health Sciences Department of Medicine, Physicians Services Incorporated of Ontario, and the Canadian Association of Gastroenterology. Career Awards were from Physicians Services Incorporated of Ontario (J Dionne) and the Canadian Institutes for Health Research (D Cook).
Author information
Authors and Affiliations
Consortia
Contributions
The authors' roles are as follows. Conception and design: JCD, DJC, LM, WA Acquisition, analysis and interpretation of the data: JCD, DJC, LM, WA, KS, JWD, MD, PM, DA, LT, JM, JT, RC, RJ, AT, CH, TK, RC-C, MA, BR, WS, KB, WS, PL, TC. Analysis of the data: JCD, LM, DC. Drafting the manuscript: JCD, DC, LM, LT, JWD, MSD, JM, JT, AT. Critiquing the manuscript: JWD, KS, MD, PM, DA, LT, JM, JT, RJ, AT, CH, TK, RC-C, MA, WA, BR, WS, KB, WS, PL, TC. Final approval: All authors provided final approval of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The DICE Investigators members are listed in acknowledgement section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dionne, J.C., Mbuagbaw, L., Devlin, J.W. et al. Diarrhea during critical illness: a multicenter cohort study. Intensive Care Med 48, 570–579 (2022). https://doi.org/10.1007/s00134-022-06663-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-022-06663-8