Abstract
Purpose
In adults requiring treatment in an intensive care unit, probiotic therapy using Lactobacillus plantarum 299v may reduce nosocomial infection. The aim of this study was to determine whether early and sustained L. plantarum 299v therapy administered to adult ICU patients increased days alive and at home.
Methods
A multicentre, parallel group, placebo-controlled, randomised clinical trial was conducted. Adult patients within 48 h of intensive care admission and expected to require intensive care beyond the day after recruitment were eligible to participate. L plantarum 299v or placebo were administered immediately after enrolment and continued for 60 days. The primary outcome was days alive and out of hospital to Day 60 (DAOH60). Secondary outcomes included nosocomial infections.
Results
The median [interquartile range (IQR)] number of DAOH60 in the probiotic (n = 110) and placebo group (n = 108) was 49.5 (IQR 37.0–53.0) and 49.0 (IQR 43.8–53.0) respectively, between-group difference of 0.0 [95% confidence interval (CI) − 6.10 to 7.1, P = 0.55]. Nosocomial infection occurred in 8 (7.3%) and 5 (4.6%) of the probiotic and placebo group participants, respectively, odds ratio 1.62 (95% CI 0.51–5.10), P = 0.57. There were no serious, or probiotic-associated adverse events.
Conclusion
Early and sustained untargeted administration of probiotic therapy with Lactobacillus plantarum 299v to adult patients admitted to the ICU is safe, but not associated with improved patient outcomes.
Similar content being viewed by others
Early and sustained probiotic administration to adult patients requiring treatment in the intensive care is safe but ineffective in improving outcomes or reducing nosocomial infection. Whether more targeted therapy is beneficial remains uncertain. |
Introduction
Critical illness requiring treatment in an intensive care unit (ICU) results in rapid and profound alterations to the gastrointestinal microflora [1, 2]. Microbiota depletion and diversity loss are associated with adverse outcomes including prolonged hospital stay, nosocomial infections and increased mortality [2,3,4]. The reintroduction of commensal bacteria using strain-specific oral probiotic therapy may mitigate these adverse effects [5, 6].
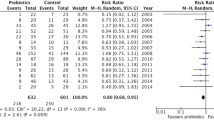
Lactobacillus (L.) plantarum 299 V is a human commensal that survives passage through the gastrointestinal tract, irrespective of gastric acidity [7]. It reduces gastrointestinal bacterial translocation, attenuates systemic inflammation in critically ill patients, and has in vitro antimicrobial activity against a wide range of potentially pathogenic species [8]. In a meta-analysis of 14 randomised trials involving adult critically ill patients, probiotic therapy decreased overall infections, a benefit most apparent in trials of L. plantarum [9]. Given that probiotics exhibit strain-specific effects, L. plantarum, as a single agent, is a strong candidate intervention to improve clinical outcomes. However, sufficient evidence to inform clinical practice is limited by trial quality and heterogeneity in the timing, dose and duration of therapy, resulting in conflicting guideline recommendations [10, 11].
The multicentre, randomised, restoration of gut microflora in critical illness trial (ROCIT) was designed to test the hypothesis that, compared with placebo, the early and sustained enteral administration of L. plantarum 299v probiotic therapy, in adult patients expected to require ongoing treatment in the ICU beyond the day after recruitment, would improve clinical outcomes including increased days alive and out of hospital to Day 60 (DAOH60).
Methods
Trial design
The investigator initiated ROCIT study was a parallel group, placebo-controlled, randomised clinical trial conducted in the ICUs of five hospitals in Perth, Western Australia (ANZCTR 12617000783325). The protocol was prospectively approved by the research ethics committee (HREC) of all participating institutions and reported prior to completion of the study (South Metropolitan Health Service Human Research Ethics Committee ref:RGS000004, St John of God Health Care Human Research Ethics Committee ref:1183) [12]. Initial HREC approval had included the provision to enrol participants who lacked capacity to provide informed consent, where prospective consent was able to be obtained from the person responsible. In June 2018, after 83 participants had been enrolled, the study management committee received an updated interpretation of local legislation from the lead HREC. This mandated that trial recruitment of the subsequent 138 participants was restricted to patients competent to provide consent prospectively. Approval to analyse and report the participants enrolled prior to this change was granted by the HREC.
Patients
Eligible patients were adults within 48 h of ICU admission and expected by the treating clinician to require ICU care beyond the calendar day after recruitment. Key exclusion criteria included immunosuppression, presence of a prosthetic heart valve or permanent pacemaker and admission to hospital from a high-level nursing or rehabilitation facility (Fig. 1). The complete exclusion criteria are provided in the Supplementary Appendix (eTable 1).
Randomisation and masking
Variable-block, 1:1 randomisation, stratified by site, was generated using a web-based interface [13]. Allocation concealment was maintained using an unblinded pharmacist to assign unique, sequential numbers to each bottle of study drug. The active study drug and the placebo were prepared by a certified facility in identically packaged capsules with 60 capsules per bottle (Metagenics Australia, 741 Nudgee Road, Northgate, Qld, 4013). All members of the treating team, the study participants, research staff and outcome adjudicators were blinded to the treatment allocation. Unblinding occurred after database lock and completion of the statistical analysis.
Study treatment
The study drug was administered once daily, beginning immediately after enrolment and continued for 60 days. Study participants who were discharged from hospital prior to Day 60 were advised to continue the treatment regime until the course was complete, then return a post-discharge treatment diary and the study drug bottle to the coordinating site. The active study drug contained 2 × 1010 colony-forming units (CFUs) of L. plantarum 299v per capsule, a dose comparable or greater than that used in other studies [9]. The placebo was of identical appearance but contained only microcrystalline cellulose. Independent testing of each study drug batch at the lead site confirmed bacterial absence in the placebo capsules and > 2 × 1010 CFUs of L. plantarum 299v in the probiotic capsules. Participants were requested to refrain from initiating any probiotic treatment during the 60 days of study participation. All other aspects of care were at the discretion of the patient and clinical teams.
Outcome measures
The primary outcome was DAOH60. This is a validated composite measure for which the components of death, index hospital length of stay and the occurrence and duration of hospital readmission, plausibly, may all be improved by probiotic therapy [14]. Days spent in a rehabilitation facility or high-level nursing facility to Day 60 were considered as days in hospital and participants who died prior to Day 60 were recorded as having zero DAOH60.
Incident nosocomial infections, a secondary outcome, were assessed independently by two blinded infectious diseases specialist clinicians. These included hospital-acquired pneumonia, ventilator-associated pneumonia, Clostridioides difficile-associated diarrhoea, surgical site infection, urinary tract infection, and blood stream infection as defined by Centre for Disease Control (CDC) criteria [15]. Antibiotic-free days were collected for all days in hospital, including any readmissions to Day 60. Quality of life was assessed using the five-level EQ-5D (EQ-5D-5L) questionnaire including the EQ-5D descriptive system with five domains (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) and the EQ visual analogue scale (EQ VAS) [16]. The number of missed study medication days was the sum of the missed days whilst hospitalised, plus, either the number of remaining capsules in returned bottles post-discharge or the number of omitted study diary days post-discharge, whichever was greater.
Statistical analysis
In the placebo group, a mean DAOH60 of 37 and standard deviation (SD) of nine was assumed, using previous estimates from the lead study site [12]. Based on a two-sided type I error rate of 0.05 and sample size inflation of 20% to account for rank-based testing, a further 5% each for withdrawn consent and loss to follow-up, a sample size of 220 participants was determined to have 80% power to detect a between-group difference in DAOH60 of 4 days. This difference was considered clinically meaningful to ICU consumers [12].
The primary analysis was performed on an intention-to-treat population, defined as all eligible, randomised patients. For non-parametric outcomes, significance was determined using the Wilcoxon rank-sum test, median difference was calculated using quantile regression, with the inversion method used to calculate a 95% confidence interval (CI). Fischer’s Exact test and Chi2 test were used to test association between categorical outcomes as appropriate. Analyses of pre-specified subgroups (sepsis defined according to sepsis-3 criteria [17], antibiotics at enrolment, ICU admission urgency and ICU admission type), and a post hoc septic shock subgroup, included an interaction term between assigned treatment and subgroup using a two-sided hypothesis test. The discrepancy in pre-specified subgroups reported in the trial registration and published protocol is provided in the Supplementary Appendix. A sensitivity analysis was conducted including all patients receiving study medication for ≥ 80% of days alive to Day 60. Each health state was converted into the corresponding utility index, indicating the preference of being in a health state, with utilities calculated using Australian value weights [18]. Adverse outcomes, based on clinician suspicion of an association with the intervention, were reported for all randomised patients. All serious adverse events, defined and reported according to the Note for Guidance on Clinical Safety Data Management: Definitions and Standards for Expedited Reporting (CPMP/ICH/377/95), were reported to the Data Safety Management Committee (Membership provided in the Supplementary Appendix). No interim analysis was planned or undertaken. A P value of less than 0.05 was deemed statistically significant. No correction was made for multiple comparisons. All data analyses were conducted using R version 3.5.1.
Results
Between July 2017 and December 2019, 221 patients were enrolled in the study (Fig. 1). Three patients were found to be ineligible, leaving an intention-to-treat population of 218. The primary outcome data were available for all participants. Baseline characteristics of the probiotic (n = 110) and placebo group (n = 108) participants were similar, although 81% of patients in the probiotic group compared with 62% in the placebo group received antibiotics at baseline (Table 1). The number of patients receiving study medication for ≥ 80% of days alive to Day 60 was 95 (86.4%), and 87 (80.6%) in the probiotic and placebo groups, respectively. Other measures of study treatment compliance are provided in the Supplementary Appendix (eTable 2).
Primary outcome
The median [interquartile range (IQR)] number of DAOH60 in the probiotic group was 49.5 (IQR 37–53) and 49 (IQR 43.8–53) in the placebo group, with a between-group absolute difference of 0.0 (95% CI − 6.1 to 7.1), P = 0.55. There were no significant between-group differences observed in the components of the primary outcome, or when analysis was limited to participants with ≥ 80% compliance (Table 2). There was no significant between-group difference for the four pre-specified subgroup pairs (Table 3).
Secondary outcomes
Nosocomial infection occurred in 8 (7.3%) and 5 (4.6%) of the probiotic and placebo group participants, respectively, odds ratio 1.62 (95% CI 0.51–5.1), P = 0.57. No participant had more than one nosocomial infection. Other clinical outcomes including ICU and hospital mortality were similar between groups (Table 2, eTable 4). Amongst survivors, overall quality of life at Day 60, as assessed by median EQ-5D-5L VAS scores was similar in the probiotic and placebo groups, 75 (IQR 60–85) and 76 (IQR 60–90), respectively, between-group difference − 1.0 (95% CI − 14.5 to 16.3), P = 0.39. The individual components scores are provided in the Supplementary Appendix (eTable 5).
A post hoc exploratory analysis suggested significant increase in DAOH60 and antibiotic-free days in the subgroup of 24 participants with septic shock at baseline (eTable 3).
Safety
There were no serious adverse events reported amongst the 221 randomised participants, including no cases of Lactobacillus infection. There were three adverse events reported in total, one in the probiotic group and two in the placebo group (eTable 6).
Discussion
In this multicentre, randomised, placebo-controlled clinical trial, the early and sustained administration of probiotic therapy with L. plantarum 299v to adult patients admitted to the ICU did not result in a significant difference in days alive and out of hospital to Day 60. Nosocomial infection and all other pre-specified secondary outcomes were also similar between groups. The administration of L. plantarum 299v was safe. There were no serious adverse events amongst participants, including no associated Lactobacilli infections, and few reported adverse events.
A systematic review of previous clinical trials suggested a lower incidence of nosocomial infection and improved clinical outcomes amongst critically ill patients receiving probiotic therapy [9]. However, the robust design of the placebo-controlled ROCIT study, powered to detect a meaningful difference in a patient-centred outcome, provides results that are consistent with the findings of other higher quality trials [9]. The ROCIT study extends these findings by evaluating the early administration of a high dose probiotic, sustained amongst survivors until ascertainment of the primary outcome at 60 days. In addition to a lack of benefit demonstrated amongst the entire cohort, subgroup analyses based on antibiotic administration at time of enrolment, presence or absence of sepsis, ICU admission urgency and type, also failed to demonstrate benefit. Similarly, an analysis of highly compliant participants, though a post-randomisation variable that could not be determined at baseline, did not suggest that the lack of benefit could be explained by insufficient probiotic exposure. Together, these findings suggest that the widespread, untargeted administration of L. plantarum 299v to patients admitted to the ICU, although safe, is ineffective.
In a large clinical trial conducted in infants in rural India, the administration of L. plantarum decreased the risk of a composite outcome including infection and death [19]. Whilst the microbiota of adults is complex and established, in infants it is newly developing. This may explain why an untargeted approach could be successful in infants but not adults. Untargeted enteral probiotic administration to critically ill patients receiving mechanical ventilation may be of specific benefit due to the risk of aspiration of gastric contents [20]. In addition, the expected mortality of the cohort in this study was relatively low, and mechanically ventilated patients may be expected to have a higher illness severity. Although the attributable mortality of ventilator-associated pneumonia is uncertain, further study of this cohort will provide important information of the role of untargeted probiotics in another high acuity cohort [21].
Alternatively, a more targeted approach, based on a specific gastrointestinal microbiome composition may identify a population of critically ill adults who would benefit from L. plantarum administration [22]. Preliminary studies have found an association between gastrointestinal microbiota composition and adverse outcomes from critical illness [23]. To date, however, there is limited evidence that this risk is modifiable [24]. This may be explained by the substantial variation in microbiota disturbance observed between and within individuals after a uniform exposure such as broad spectrum antibiotic [25]. The post hoc analysis suggesting benefit of L. plantarum 299v amongst patients with septic shock may be a chance finding and must be considered hypothesis generating, but may be due to consistent, severe dysbiosis in this subgroup. Irrespective, developing targeted interventions will require a mechanistic and individualised understanding of the effects probiotics exert on the gastrointestinal microbiota in critical illness. Developing tools to provide information on the composition of the gastrointestinal microbiota in a clinically relevant timeframe could assist with a goal of precision restoration of gut microbiota constituents and diversity.
There are several limitations to this study. Observed days alive and at home in the placebo group were higher than estimated in the sample size calculation so that the findings may be underpowered. However, on the basis of the minimal between-group differences in all outcome measures, a false-negative finding is considered unlikely. Although the trial was initially approved to include participants who lacked capacity to provide consent, the approval to enrol incapacitated patients was rescinded after approximately one third of the participants were enrolled, and enrolment then limited to participants with capacity to provide prospective consent. Incapacitated patients may differ in important characteristics, including illness severity, and overall mortality of 5% is low for an ICU cohort. However, outcomes were similar amongst planned and unplanned ICU admissions, suggesting that identifying a cohort based on higher acuity alone is unlikely to lead to different findings. Reliance on clinical suspicion of an adverse event may increase the chance of underreporting, although lack of any outcome difference suggests that any such effect resulted in minimal impact. Finally, whether L. plantarum 299v administration targeted to a subgroup of critically ill patients, or whether untargeted administration of an alternative probiotic is beneficial, remains uncertain.
Conclusion
The early and sustained administration of probiotic therapy with L. plantarum 299v to adult patients admitted to the ICU did not result in a significant difference in days alive and at home to Day 60.
Availability of data and material
Requests for data should be made to the corresponding author. Each request requires a research proposal including a clear research question and proposed analysis plan. Requests will be considered on an individual basis and are subject to review and approval by the ROCIT management committee and relevant human research ethics committees.
References
McDonald D, Ackermann G, Khailova L, Baird C, Heyland D, Kozar R, Lemieux M, Derenski K, King J, Vis-Kampen C, Knight R, Wischmeyer PE (2016) Extreme dysbiosis of the microbiome in critical illness. mSphere 1(4):e0019–16
Aardema H, Lisotto P, Kurilshikov A, Diepeveen JRJ, Friedrich AW, Sinha B, de Smet A, Harmsen HJM (2019) Marked changes in gut microbiota in cardio-surgical intensive care patients: a longitudinal cohort study. Front Cell Infect Microbiol 9:467
Freedberg DE, Zhou MJ, Cohen ME, Annavajhala MK, Khan S, Moscoso DI, Brooks C, Whittier S, Chong DH, Uhlemann AC, Abrams JA (2018) Pathogen colonization of the gastrointestinal microbiome at intensive care unit admission and risk for subsequent death or infection. Intensive Care Med 44:1203–1211
Xu R, Tan C, Zhu J, Zeng X, Gao X, Wu Q, Chen Q, Wang H, Zhou H, He Y, Pan S, Yin J (2019) Dysbiosis of the intestinal microbiota in neurocritically ill patients and the risk for death. Crit Care 23:195
Ho KM, Kalgudi S, Corbett JM, Litton E (2020) Gut microbiota in surgical and critically ill patients. Anaesth Intensive Care 48(3):179–195
McFarland LV, Evans CT, Goldstein EJC (2018) Strain-specificity and disease-specificity of probiotic efficacy: a systematic review and meta-analysis. Front Med (Lausanne) 5:124
Goossens D, Jonkers D, Russel M, Thijs A, van den Bogaard A, Stobberingh E, Stockbrugger R (2005) Survival of the probiotic, L. plantarum 299v and its effects on the faecal bacterial flora, with and without gastric acid inhibition. Dig Liver Dis 37:44–50
McNaught CE, Woodcock NP, Anderson ADG, MacFie J (2005) A prospective randomised trial of probiotics in critically ill patients. Clin Nutr 24:211–219
Manzanares W, Lemieux M, Langlois PL, Wischmeyer PE (2016) Probiotic and synbiotic therapy in critical illness: a systematic review and meta-analysis. Crit Care 20:262
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, McCarthy MS, Davanos E, Rice TW, Cresci GA, Gervasio JM, Sacks GS, Roberts PR, Compher C, Society of Critical Care M, American Society for P, Enteral N (2016) Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 40:159–211
Dhaliwal R, Cahill N, Lemieux M, Heyland DK (2014) The Canadian critical care nutrition guidelines in 2013: an update on current recommendations and implementation strategies. Nutr Clin Pract 29:29–43
Litton E, Anstey M, Broadhurst D, Chapman AR, Currie A, Ferrier J, Gummer J, Higgins A, Lim J, Manning L, Myers E, Orr K, Palermo AM, Paparini A, Pellicano S, Raby E, Rammohan A, Regli A, Richter B, Salman S, Strunk T, Waterson S, Wibrow B, Wood FM (2020) Study protocol for the safety and efficacy of probiotic therapy on days alive and out of hospital in adult ICU patients: the multicentre, randomised, placebo-controlled Restoration Of gut microflora in Critical Illness Trial (ROCIT). BMJ Open 10:e035930
Sealed Envelope LTD, 501 Clerkenwell workshops, 27-31 Clerkenwell Close, London EC1R 0AT, UK. sealedenvelope.com
Jerath A, Austin PC, Wijeysundera DN (2019) Days alive and out of hospital: validation of a patient-centered outcome for perioperative medicine. Anesthesiology 131:84–93
CDC (2019) National Healthcare Safety Network (NHSN) patient safety component manual. In: Chapter 17: CDC/NHSN surveillance definitions for specific types of infections
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20:1727–1736
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA J Am Med Assoc 315:801–810
Norman R, Cronin P, Viney R (2013) A pilot discrete choice experiment to explore preferences for EQ-5D-5L health states. Appl Health Econ Health Policy 11:287–298
Panigrahi P, Parida S, Nanda NC, Satpathy R, Pradhan L, Chandel DS, Baccaglini L, Mohapatra A, Mohapatra SS, Misra PR, Chaudhry R, Chen HH, Johnson JA, Morris JG, Paneth N, Gewolb IH (2017) A randomized synbiotic trial to prevent sepsis among infants in rural India. Nature 548:407–412
Cook DJ, Johnstone J, Marshall JC, Lauzier F, Thabane L, Mehta S, Dodek PM, McIntyre L, Pagliarello J, Henderson W, Taylor RW, Cartin-Ceba R, Golan E, Herridge M, Wood G, Ovakim D, Karachi T, Surette MG, Bowdish DM, Lamarche D, Verschoor CP, Duan EH, Heels-Ansdell D, Arabi Y, Meade M, Investigators P, the Canadian Critical Care Trials G (2016) Probiotics: prevention of severe pneumonia and endotracheal colonization trial-PROSPECT: a pilot trial. Trials 17:377
Bekaert M, Timsit JF, Vansteelandt S, Depuydt P, Vesin A, Garrouste-Orgeas M, Decruyenaere J, Clec’h C, Azoulay E, Benoit D, Outcomerea Study G (2011) Attributable mortality of ventilator-associated pneumonia: a reappraisal using causal analysis. Am J Respir Crit Care Med 184:1133–1139
Haak BW, Prescott HC, Wiersinga WJ (2018) Therapeutic potential of the gut microbiota in the prevention and treatment of sepsis. Front Immunol 9:2042
Lamarche D, Johnstone J, Zytaruk N, Clarke F, Hand L, Loukov D, Szamosi JC, Rossi L, Schenck LP, Verschoor CP, McDonald E, Meade MO, Marshall JC, Bowdish DME, Karachi T, Heels-Ansdell D, Cook DJ, Surette MG, Investigators P, Trials G, Canadian Critical Care Translational Biology G (2018) Microbial dysbiosis and mortality during mechanical ventilation: a prospective observational study. Respir Res 19:245
McFarland LV (2014) Use of probiotics to correct dysbiosis of normal microbiota following disease or disruptive events: a systematic review. BMJ Open 4:e005047
Dethlefsen L, Relman DA (2011) Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci USA 108(Suppl 1):4554–4561
Acknowledgements
The authors would like to thank the ROCIT participants and study sites, and would like to thank the consumers from the Consumer and Community Involvement Program (The University of Western Australia, MBDP M503, 35 Stirling Highway, Crawley, WA, 6009) for their contribution to the study design.
Funding
ROCIT is funded by grants from the Department of Health, Government of Western Australia Research Translation Projects, the St John of God Hospital Foundation, and the Fiona Wood Foundation. Study drug was supplied by Metagenics Australia (previously Health World), 741 Nudgee Road, Northgate, Queensland 4013, Australia. The funding bodies and Metagenics Australia have had no input into the design, conduct, analysis or reporting of the trial. The study sponsor is the Fiona Stanley Fremantle Hospital Group, South Metropolitan Health Service, Western Australia.
Author information
Authors and Affiliations
Contributions
EL: conceived the study, wrote the first draft of the protocol, chaired the study management committee, supervised the data analysis, wrote the first draft of the manuscript and takes overall responsibility for the study. MA, AC, AC, JG, JL, AP, AR, BR, SS, TS and BW: contributed to the study design, protocol development, data analysis and redrafting the study manuscript. DB contributed to the study design, protocol development, and redrafting of the study manuscript. JF, A-MP and SW: contributed to the study design, protocol development, data collection and redrafting the study manuscript. AH: contributed to the study design, protocol development, data analysis and redrafting the study manuscript and led the health economic aspects. LM: contributed to the study design, protocol development, data analysis and redrafting the study manuscript and co-led the infectious diseases blinded outcome evaluation. EM: contributed to the study design, data collection and redrafting the study manuscript. KO: contributed to the study design, protocol development, including randomisation sequence and redrafting the study manuscript. SP was the overall project manager and contributed to the study design, protocol development, data collection, analysis and redrafting the study manuscript. ER co-led the infectious diseases blinded outcome assessment and contributed to the study design, protocol development, data analysis and redrafting the study manuscript. AR: contributed to the study design, protocol development, data analysis and redrafting the study manuscript with specific input into health economics. DW: contributed to the study statistical design, protocol development, led the statistical data analysis and redrafting the study manuscript. FW: contributed to the study design, protocol development, data analysis and redrafting the study manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest.
Ethical approval
The protocol was prospectively approved by the human research ethics committee of all participating institutions and reported prior to completion of the study. This was the South Metropolitan Health Service Human Research Ethics Committee ref:RGS000004, and the St John of God Health Care Human Research Ethics Committee ref:1183.
Consent to participate
Consent to participate was provided prospectively from all participants or their legal surrogate.
Consent for publication
The signed consent forms for all participants included consent to publication of aggregate data. The authors all consent to publication of the manuscript.
Code availability
Requests for code should be made to the corresponding author and will be considered on an individual basis by the study management committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All authors in author group are members of ROCIT Investigators.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Litton, E., Anstey, M., Broadhurst, D. et al. Early and sustained Lactobacillus plantarum probiotic therapy in critical illness: the randomised, placebo-controlled, restoration of gut microflora in critical illness trial (ROCIT). Intensive Care Med 47, 307–315 (2021). https://doi.org/10.1007/s00134-020-06322-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-020-06322-w