Abstract
Introduction
In 1992, we published a report on the effect of positive end-expiratory pressure (PEEP) on right ventricular (RV) function in humans.
Results
We measured RV volumes and pressures and pericardial pressure (Ppc) as PEEP was increased from zero to 15 cm H20 in 12 patients after thoracotomy, using a pulmonary arterial catheter equipped with a rapid responding thermistor that allowed measurement of RV ejection fraction (RVef), while Ppc was measured via a pericardial balloon catheter. RV end-diastolic volume (EDV) was estimated as the ratio of stroke volume (SV) to RVef, whereas RV end-systolic volume (ESV) were estimated as RV EDV-SV. PEEP increased Ppc and Pra, but RVef unaltered. There was no relation between either RV filling pressure (Pra-Ppc) and EDV or the change in RV filling pressure and EDV, although EDV varied significantly with PEEP (p < 0.05). The relations between EDV and both SV and RVef were weak (r = 0.54 and 0.55, respectively). RVef varied inversely with ESV (r = −0.77), although it showed no relation to transmural peak pulmonary artery pressure (r = 0.28). However, both absolute and relative changes in EDV corresponded closely with respective ESV values (r = 0.94). We concluded that EDV varies independently of changes in filling pressure and that changes in ESV occur independently of changes in ejection pressure. These data can be explained by assuming that the RV shape changes can dissociate changes in RV EDV from changes in RV wall stress (preload). Thus, changes in RV EDV may or may not alter SV but should proportionately change ESV to a degree dependent on election pressure and contractility.
Conclusions
Subsequent studies confirmed our findings which can be summarized as 1) RV filling is independent of Pra; thus central venous pressure cannot be used to estimate RV preload; and 2) for cardiac output to increase by the Starling mechanism the RV must dilate increasing RV ESV. Since the pericardium limits absolute biventricular volume, there is a finite limit to which cardiac output can increase by the Starling mechanism defined not by left ventricular contractility but by RV function. And 3) if fluid loading causes Pra to increase without increasing cardiac output, then resuscitation should stop as the patient is going into acute cor pulmonale. These truths help bedside clinicians understand the echocardiographic and hemodynamic signatures of both RV failure and volume responsiveness.
Similar content being viewed by others
Summary of original study
In 1992 Jean-Louis Vincent, Jean Marie DeSmet, and I published a study in the American Review of Respiratory Disease (blue journal) entitled “Effect of positive end-expiratory pressure on right ventricular function in humans” [1]. In that study we asked the question: What is the effect of changing intrathoracic pressure and lung volume by increasing positive end-expiratory pressure (PEEP) on right ventricular (RV) function when one could simultaneously measure right atrial pressure, pericardial pressure (Ppc), and RV volume? The study was unique at the time because we were able to measure Ppc using a specially designed balloon catheter inserted during cardiac surgery and removed 12 h following surgery. Previous studies on the effect of PEEP on of RV function in critically ill patients did not measure the effect that PEEP has on intrathoracic pressure or Ppc [2, 3]. Since PEEP must increase intrathoracic pressure but to a variable degree depending on lung and chest wall mechanics, one would need to measure intrathoracic pressure to note how RV filling pressures were altered. Previous studies using pericardial catheters were done only during open-chest intraoperative settings with volume loading and then only examining the relation between changing right atrial pressure and Ppc [4]. Importantly, Ppc was measured with an air-filled flat balloon catheter (Holt catheter) [5]. We developed a special thin-walled air-filling balloon catheter that could be inserted into the pericardium during cardiac surgery and remain there postoperatively, being removed at the time the chest tubes were also removed. Thus, we could now measure the impact that PEEP would have on RV function when RV filling pressure, estimated as right atrial pressure minus Ppc, called transmural right atrial pressure, was directly measured. RV end-systolic pressure was presumed to approximate pulmonary artery systolic pressure and was measured by a pulmonary artery catheter. RV volumes were estimated by the pulmonary artery catheter ejection fraction technique. This technique analyzes the thermodilution decay profile as the ratios of sequential reciprocals of the residual thermal signal sensed in the pulmonary artery for each heartbeat. Following a right atrial cold saline bolus using a rapid response thermistor pulmonary artery catheter, the thermal signal decreases in a step fashion presuming full thermal mixing in the right ventricle prior to each ejection. Thus, the ratio of the initial thermal signal minus the residual thermal signal of the first beat to the same ratio of the second beat will equal the same ratio of the second to the third beats, third to the fourth, etc., and all will equal the residual thermal volume remaining in the right ventricle. One minus the residual thermal signal is the RV ejection fraction (RVef). Cardiac output is estimated by the Stewart–Hamilton equation independent of the RVef calculation and when divided by heart rate equals stroke volume (SV). Since RV end-diastolic volume (EDV) equals the ratio of SV to RVef, RV EDV is easily calculated. Similarly RV end-systolic volume (ESV) equals the difference between RV EDV and SV. Thus, with a single thermal ejection using a rapid response thermistor pulmonary artery catheter one can measure not only cardiac output but RV EDV, ESV, and RVef. Although echocardiographic analysis of RV function was available then, it cannot measure intracardiac pressures, thus is unable to assess parameters like RV diastolic compliance and end-systolic elastance [6].
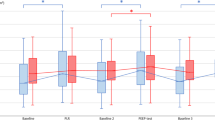
What we found was that as PEEP was progressively increased from 0 to 5 to 10 to 15 cmH2O, RV volumes decreased while cardiac output decreased slightly and both RVef and transmural pulmonary artery pressure (pulmonary artery pressure minus pericardial pressure) remained relatively unchanged and left atrial pressure increased. However, one of the first things we wished to define was RV diastolic compliance, which we reasoned to be reflected by the relation between RV EDV and RV filling pressure measured as transmural right atrial pressure. Surprisingly, there was no relation between RV EDV and transmural right atrial pressure (Fig. 1) or RV SV and transmural right atrial pressure. However, we noted that as RV ESV increased RVef decreased slightly but consistently for all subjects, such that the relation between RV EDV and ESV was highly linear with a slope equal to one minus RVef (Fig. 2). These data supported the hypothesis that the normal human right ventricle fills below its unstressed volume, an observation already made at that time by Tyberg et al. [4]. On the basis of these data we concluded that over the normal physiological range, changes in RV EDV occur below the right ventricle’s stressed volume level, such that these volume changes occurred without any change in wall stretch. Presumably, conformational changes in RV shape rather than myocardial fiber stretch allow these RV EDV changes to occur without measurable changes in RV distending pressure. If this were so, we reasoned that RV preload, which is RV wall stretch, would remain constant as RV EDV varied. In support of this hypothesis, we saw that there was a reverse linear relationship between RV EDV and RVef (Fig. 3). If, as with the left ventricle, increased RV filling increased RV wall stretch, then one would expect RV ejection fraction to either remain constant or increase by the Frank–Starling mechanism. However, since we saw the opposite, this supported the claim that under normal conditions the RV is functioning below its unstressed volume and thus RV preload is independent of RV EDV. Importantly, these findings agreed with those of previous studies by other groups who also found an inverse relation between RV EDV and RVef, but were at a loss to explain the mechanism behind these findings [7, 8]. And these findings confirmed both our earlier observation in patients being treated in an emergency department for acute circulatory shock, namely that the RV EDV to ESV ratio was highly linear with a slope less than one [9] and those of other earlier investigators, all of whom were at a loss to explain this close coupling [7, 10]. We subsequently published a larger series of studies with Jean-Francois Dhainaut in 18 septic patients wherein we varied RV EDV over a wider range using variable inflation of military anti-shock trousers, finding that the RV EDV to ESV relation was remarkably linear and unique to each patient [11]. The corollary to these findings was that if RV volume did alter RV preload, did increase RV distending pressure, then the RV was either hypertrophied with diastolic dysfunction or overdistended as in acute cor pulmonale. In all these studies the subjects were sedated and on controlled mechanical ventilation, but there is no reason to believe the findings would be different in spontaneously breathing subjects.
Relation between RV EDV and transmural Pra data pairs for all patients as PEEP is increased from 0 to 5 to 10 to 15 cmH2O. No consistent relation could be found. For individual patients, RV EDV varied widely without measurable changes in transmural Pra.
RV EDV right ventricular end-diastolic volume, Pra tm transmural right atrial pressure (recalculated from data original published in Pinsky et al. [1])
Relation between RV EDV and RV ESV for all patients as PEEP is increased from 0 to 5 to 10 to 15 cmH2O. A highly linear relation between the two variables existed (r = 0.94, P < 0.001) both for the group as a whole and for individual patients. The dotted line is the line of identity (recalculated from data original published in Pinsky et al. [1])
Relation between RV EDV and RVef as PEEP is increased from 0 to 5 to 10 to 15 cmH2O (r = −0.77, p < 0.001). RV EDV right ventricular end-diastolic volume, RVef right ventricular ejection fraction (recalculated from data original published in Pinsky et al. [1])
Implications of this original study
Initially, we were surprised to see the extremely linear RV EDV to ESV relationship and felt it must be a product of some sort of mathematical coupling. However, the calculations of RV SV and RVef were made from different aspects of the thermal decay curve, so they were not mathematically coupled. Upon further study, two findings dissuaded us from dismissing this relationship as spurious. First, using radionuclide-based estimates of left ventricular (LV) ejection fraction, there were no or minimal LV EDV to ESV correlations [12]. Indeed, if LV EDV and ESV were correlated, the subjected tended to be sicker [13]. Finally, in a previous clinical trial measuring RV ejection fraction during the expected myocardial depression and recovery following cardiopulmonary bypass, the authors had reported RV EDV and stroke volume data that allowed us to calculate RV ESV. When recalculated, it too showed that 6–8 h following bypass the RV EDV to ESV ratio was equal to or greater than one during this post-bypass myocardial depression phase, decreasing to about 0.8 approximately 12 h later [14]. We subsequently performed a three-phase study assessing the dynamic RV EDV to ESV immediately after cardiac surgery when contractility was normal, 8 h later when contractility was depressed, and then again at 24 h when it had recovered again [15]. That study clearly showed that the RV EDV/ESV ratio is usually about 0.7–0.8 increasing to 1.1–1.0 during post-bypass myocardial stunning and returning to pre-stunning values at 24 h. Since the RV EDV to ESV ratio is one minus RVef, if the slope is one, then RVef is zero and the RV is not volume responsive. Thus, increasing RV EDV by fluid loading will not increase RV SV. In these settings, fluid loading in acute RV failure states will not only increase RV EDV without increasing cardiac output, but may decrease cardiac output if RV dilation limits LV filling [16].
The implications of these data are twofold. First, measures of central venous pressure as a surrogate for right atrial pressure could never be used to predict volume responsiveness [17] because they do not equate to RV preload. However, changes in central venous pressure remain an excellent measure of when fluid resuscitation has exceeded the normal RV unstressed volume operating range. In this setting with fluid resuscitation if one sees central venous pressure increase whereas RV SV either does not change or decreases, RV failure exits and further fluid challenges are contraindicated. Indeed, Jardin et al. [10] indirectly found the same results when they measured RV volumes in patients with acute lung injury and found that if they restored RV volume to their baseline values with fluid resuscitation, cardiac output increased, whereas if further fluid resuscitation was done, cardiac output did not increase but central venous pressure rose abruptly and paradoxical leftward shift of the intraventricular septum during diastole developed. They also saw that the immediate effect of PEEP was to increase RV afterload causing the right ventricle to dilate, first with an immediate increase in RV ESV as RV SV decreased with a subsequent decrease in venous return as the dilating right ventricle caused central venous pressure to rise. These observations collectively allow the bedside clinician to use increases in central venous pressure in response to a volume challenge as a stopping rule for further fluid administration. The second implication of these findings is that for cardiac output to increase by the Starling mechanism, RV ESV must also increase. Thus, owing to pericardial restraint limiting absolute biventricular volume, there is a finite amount of volume responsiveness that can be achieved by fluid resuscitation, limited more by pericardial volume limitations than circulating blood volume. Another way of thinking about this linkage between RV EDV and ESV is that the right ventricle is primarily a conduit for flow rather than a pump. Indeed, since the ESV/EDV slope is normally 0.7, at most only 30 % of the increase in cardiac output can be explained by RV Starling mechanism.
Subsequent studies
So what happened in the practice of acute care medicine after this study was published? Subsequent clinical studies using a variety of means to measure RV volumes demonstrated similar tight RV EDV to ESV ratios, and that these ratios were inversely proportional RV performance reserve [18]. However, at about the same time as this paper’s publication, the general focus of critical care medicine assessments of RV function shifted from the pulmonary artery catheter and its RV ejection fraction data to echocardiography and functional measures of RV ejection such as its fractional area of contraction. Inherently, this altered the discussion away from acute cor pulmonale to RV diastolic volume overload as quantified by the ratio of RV to LV diameters and paradoxical septal shift [19]. The good news was that we had just entered the era of lower tidal volume ventilation. When retrospective analysis of echocardiographic analyses over years was made, the trend toward lower tidal volume ventilation was also associated with a markedly decreased RV diastolic dysfunction. Thus, using lower tidal volume ventilation not only limited ventilator-associated lung injury but also caused less of an increase in pulmonary vascular impedance and an associated lower incidence of acute cor pulmonale [20]. Furthermore, recent studies using continuously available echocardiography to assess both LV and RV function routinely document that aggressive fluid resuscitation induces acute cor pulmonale with tricuspid regurgitation and lack of further volume responsiveness [21]. These data underscore further the limits to which RV function and cardiac output can be pushed using volume resuscitation. The reader is recommended two recent reviews [22, 23] that summarize the role of central venous pressure and mechanical ventilation and PEEP on cardiovascular function.
Secondary implications of our original study relate to RV hypertrophy. Inherently, there is nothing beneficial occurring when the right ventricle hypertrophies in response to an increased afterload. RV coronary blood flow is already compromised in pulmonary arterial pressure overload states and increasing hypertrophy is not associated with new coronary vessel growth, so ischemia and the shift from aerobic to anaerobic metabolism occurs as is commonly seen with myocardial stunning [24]. This, coupled with the marked decrease in RV diastolic compliance, profoundly limits overall cardiovascular reserve [25]. Hence the importance of seeing central venous pressure decrease and RV stroke volume increase with anti-pulmonary hypertension therapies [26]. The decreasing central venous pressure may initially reflect a decreasing RV afterload, but over time it reflects reverse remodeling with restoration of normal RV diastolic compliance.
Unmasking right ventricular physiology
The determinants of RV function are uniquely different from those determining LV function even though both ventricles have anatomically and functionally similar cardiac myocytes and the same beat frequency.
First, RV filling occurs without any measurable change in RV distending pressure [1, 4]. Thus, preload is independent of RV EDV unless the RV is hypertrophied. At which point, central venous pressure increases in proportion to the increase in RV EDV [26]. Since venous return is the primary determinant of steady state cardiac output and since central venous pressure is the backpressure to venous return [27] acute RV overload must be associated with both increases in central venous pressure and cardiovascular compromise (acute cor pulmonale). Thus giving more intravenous volume challenges to patients with acute cor pulmonale (acute right heart failure) will only decrease cardiac output further.
Second, that RV filling occurs below its unstressed volume has fundamental survival advantages for the host. Since spontaneous inspiration usually decreases intrathoracic pressure, central venous pressure will also decrease increasing the pressure gradient for venous return [27]. Thus, both RV filling and subsequently RV stroke volume will increase pulmonary blood flow at the same time alveolar gas is being refreshed by the tidal breath [28]. For this to provide maximal venous return, central venous pressure must not increase as RV EDV increases. Accordingly, the natural high RV diastolic compliance allows the increased venous return to be maximal. Furthermore, for this process to be effective, pulmonary vascular resistance must remain low. Under normal circumstances, with normal pulmonary vasculature and tidal volumes, pulmonary artery pressure does not increase more than a few millimeters of mercury as flow increases greatly [28]. Thus, the cardiopulmonary system is ideally adapted to maximize blood flow and gas exchange during spontaneous breathing and to increase them rapidly with exercise.
Third, positive-pressure breathing by dissociating tidal air inflow from pulmonary blood flow [26] will result in poorer ventilation/perfusion matching and worse gas exchange than spontaneous ventilation. Furthermore, if the tidal breaths are too large, they will also impede venous return causing acute cor pulmonale and a decrease in cardiac output [19].
Summary
We now have an increasing appreciation that RV function is the primary determinant of cardiac output in our critically ill patients. Minimizing lung overdistention and protective ventilatory strategies not only help the lungs but the circulation as well, whereas over-resuscitation rapidly progresses to RV volume overload and reduced cardiac reserve. Thus, the optimal volume state may well be defined by the best RV EDV to SV ratio and any further increase in cardiac output may only be effectively created by increased inotropy without otherwise impairing biventricular ejection effectiveness [26, 29]. The right ventricle has been the “forgotten ventricle” in clinical practice for many years. But with increased ability to accurately and serially assess RV function at the bedside using echocardiographic techniques [28, 30], increased awareness of its central role in cardiovascular homeostasis is emerging. The genie is out of the bottle and it will not easily return into it.
On the basis of these findings one can make the following conclusions and perhaps oversimplifications (Table 1). First, that elevation in central venous pressure must reflect RV dysfunction either due to gross overdistention or RV hypertrophy. That the right ventricle may otherwise be normal is immaterial; pulmonary outflow obstruction whether due to hyperinflation, pulmonary embolism, or pulmonary hypertension is causing cardiovascular reserve to be compromised. Second, during fluid resuscitation, if central venous pressure raises without a concomitant increase in RV stroke volume, then the patient is slipping into acute cor pulmonale and further fluid resuscitation as isolated therapy is contraindicated. Finally, under normal conditions, since there is a tight linear relation between RV EDV and ESV and since RV preload is constant, for cardiac output to increase in response to acute volume loading RV ESV must also increase. Thus, the degree to which increasing LV preload can increase cardiac output is primarily limited by RV filling. Such findings make the interpretation of echocardiographic assessment of RV function easier. RV dilation and paradoxical septal shift are merely manifestations of these processes. Furthermore, when increasing RV EDV requires central venous pressure to also rise, the right ventricle is either overdistended or has decreased diastolic compliance, as occurs with RV hypertrophy. In essence, when the right ventricle behaves like the left ventricle, in having a definable diastolic compliance, the right ventricle is in trouble.
References
Pinsky MR, DeSmet JM, Vincent JL (1992) Effect of positive end-expiratory pressure on right ventricular function in humans. Am Rev Respir Dis 146:681–687
Biondi JW, Schulman DS, Soufer R et al (1988) The effect of incremental positive end-expiratory pressure on right ventricular hemodynamics and ejection fraction. Anest Analg 67:151–155
Martin C, Saux P, Albanese J, Bonneru JJ, Gouin E (1987) Right ventricular function during positive end-expiratory pressure: thermodilution evaluation and clinical application. Chest 92:999–1004
Tyberg JV, Taichman GC, Smith ER, Douglas ER, Smiseth OA, Keon WJ (1986) The relationship between pericardial pressure and right atrial pressure: an intraoperative study. Circulation 73:428–432
Holt JP, Rhode EA, Kines H (1960) Pericardial and ventricular pressure. Circ Res 8:1171–1181
Brown KA, Ditchey RV (1988) Human right ventricular end-systolic pressure-volume relation defined by maximal elastance. Circulation 78:81–91
Martyn JAJ, Snider MT, Farago LF, Burke JE (1981) Thermodilution right ventricular volume: a novel and better predictor of volume replacement in acute thermal injury. J Trauma 21:619–624
Boldt J, Kling D, Bormann BV, ScheId H, Hempelmann G (1988) Influence of PEEP ventilation immediately after cardiopulmonary bypass on right ventricular function. Chest 94:566–571
Reuse C, Vincent JL, Pinsky MR (1990) Measurements of right ventricular volumes during fluid challenge. Chest 98:1450–1454
Jardin F, Gueret P, Dubourg O, Farcot J, Margairaz A, Bourdarids J (1985) Right ventricular volumes by thermodilution in the adult respiratory distress syndrome. Chest 88:34–39
Dhainaut JF, Pinsky MR, Nouria S, Slomka F (1997) Right ventricular function in human sepsis: a thermodilution study. Chest 112:1043–1049
Santamore WP, Heckman JL, Bovee AA (1986) Right and left ventricular pressure-volume response to elevated pericardial pressure. Am Rev Respir Dis 134:101–107
Renlund DG, Gerstenblith G, Fleg JL et al (1990) Interaction between left ventricular end-diastolic and end-systolic volume in normal humans. Am J Physiol 258:H473–H481
Stein KL, Breisblatt WM, Wiolfe J, Gasior TA, Hardesty RL (1990) Depression and recovery of right ventricular function after cardiopulmonary bypass. Crit Care Med 18:1197–1200
Chandler JM, Stein KL, Gasior TA, Kormos RL, Pinsky MR (1992) Depression of right ventricular function after cardiopulmonary bypass (CPB) is exacerbated by elevated preload. Chest 102:128S
Brinker JA, Weiss I, Lappe DL et al (1980) Leftward septal displacement during right ventricular loading in man. Circulation 61:626–633
Shippy CR, Appel PL, Shoemaker WC (1984) Reliability of clinical monitoring to assess blood volume in critically ill patients. Crit Care Med 12:107–112
Dambrosio M, Fiore G, Brienza N et al (1996) Right ventricular myocardial function in ARF patients. Intensive Care Med 22:772–780
Vieillard-Baron A, Schmitt JM, Augarde R, Fellahi JL, Prin S, Page B, Bauchet A, Jardin F (2001) Acute cor pulmonale in acute respiratory distress syndrome submitted to protective ventilation: incidence, clinical implications and prognosis. Crit Care Med 29:1551–1555
Vieillard-Baron A, Loubieres Y, Schmitt JM, Page B, Dubourg O, Jardin F (1999) Cyclic changes in right ventricular output impedance during mechanical ventilation. J Appl Phyiol 87:1644–1650
Cioccari L, Baur HR, Berger D, Wiegand J, Takala J, Merz TM (2013) Hemodynamic assessment of critically ill patients using a miniaturized transesophageal probe. Crit Care 17:R121
Feihl F, Broccard AF (2009) Interactions between respiration and systemic hemodynamics. Part II: practical implications. Intensive Care Med 35:198–205
Funk DJ, Jacobsohn E, Kumar A (2013) Role of the venous return in critical illness and shock: part 11—shock and mechanical ventilation. Crit Care Med 41:573–579
Gomez-Arroyo J, Mizuno S, Szczepanek K, Van Tassell B, Natarajan R, dos Remedios CG, Drake JI, Farkas L, Kraskauskas D, Wijesinghe DS, Chalfant CE, Bigbee J, Abbate A, Lesnefsky EJ, Bogaard HJ, Voelkel NF (2013) Metabolic gene remodeling and mitochondrial dysfunction in failing right ventricular hypertrophy secondary to pulmonary arterial hypertension. Circ Heart Fail 6:136–144
Matthay RA, Berger HJ, Davies RA, Loke J, Mahler DA, Gottschalk A, Zaret BL (1980) Right and left ventricular exercise performance in chronic obstructive pulmonary disease: radionuclide assessment. Ann Intern Med 93:234–239
Simon M, Deible C, Mathier M, Shroff S, Pinsky MR, Lopez-Candales A (2009) Tissue Doppler imaging of right ventricular decompensation in pulmonary hypertension. Congest Heart Fail 15:271–276
Pinsky MR (1984) Instantaneous venous return curves in an intact canine preparation. J Appl Physiol 56:765–771
Pinsky MR (1984) Determinants of pulmonary artery flow variation during respiration. J Appl Physiol 56:1237–1245
Pellerin D, Sharma R, Elliott P, Veyrat C (2003) Tissue Doppler, strain and strain rate echocardiography for the assessment of left and right ventricular systolic function. Heart 89:iii9–iii17
Vieillard-Baron A, Slama M, Mayo P, Charron C, Amiel JB, Esterez C, Leleu F, Repesse X, Vignon P (2013) A pilot study on safety and clinical utility of a single-use 72-hour indwelling transesophageal echocardiographic probe. Intensive Care Med 39:629–635
Acknowledgments
This work was supported in part by National Institutes of Health (NIH) Grants HL073198, HL076124, HL67181, and RR023267.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinsky, M.R. My paper 20 years later: Effect of positive end-expiratory pressure on right ventricular function in humans. Intensive Care Med 40, 935–941 (2014). https://doi.org/10.1007/s00134-014-3294-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3294-8