Abstract
Chondral and osteochondral lesions encompass several acute or chronic defects of the articular cartilage and/or subchondral bone. These lesions can result from several different diseases and injuries, including osteochondritis dissecans, osteochondral defects, osteochondral fractures, subchondral bone osteonecrosis, and insufficiency fractures. As the cartilage has a low capacity for regeneration and self-repair, these lesions can progress to osteoarthritis. This study provides a comprehensive overview of the subject matter that it covers. PubMed, Scopus and Google Scholar were accessed using the following keywords: “chondral lesions/defects of the femoral head”, “chondral/cartilage lesions/defects of the acetabulum”, “chondral/cartilage lesions/defects of the hip”, “osteochondral lesions of the femoral head”, “osteochondral lesions of the acetabulum”, “osteochondral lesions of the hip”, “osteochondritis dissecans,” “early osteoarthritis of the hip,” and “early stage avascular necrosis”. Hip osteochondral injuries can cause significant damage to the articular surface and diminish the quality of life. It can be difficult to treat such injuries, especially in patients who are young and active. Several methods are used to treat chondral and osteochondral injuries of the hip, such as mesenchymal stem cells and cell-based treatment, surgical repair, and microfractures. Realignment of bony anatomy may also be necessary for optimal outcomes. Despite several treatments being successful, there is a lack of head-to-head comparisons and large sample size studies in the current literature. Additional research will be required to provide appropriate clinical recommendations for treating chondral/osteochondral injuries of the hip joint.
Zusammenfassung
Chondrale und osteochondrale Läsionen umfassen verschiedene akute oder chronische Defekte des Gelenkknorpels und/oder des subchondralen Knochens. Diese Läsionen können durch viele unterschiedliche Erkrankungen und Verletzungen verursacht sein, darunter Osteochondritis dissecans, osteochondrale Defekte, osteochondrale Frakturen, subchondrale Knochennekrose und Insuffizienzfrakturen. Da Knorpel eine geringe Fähigkeit zur Regeneration und Selbstheilung hat, können die Läsionen zur Arthrose fortschreiten. Die vorliegende Studie bietet einen umfassenden Überblick zum Thema. PubMed, Scopus und Google Scholar wurden mit den folgenden Begriffen durchsucht: „chondral lesions/defects of the femoral head“, „chondral/cartilage lesions/defects of the acetabulum“, „chondral/cartilage lesions/defects of the hip“, „osteochondral lesions of the femoral head“, „osteochondral lesions of the acetabulum“, „osteochondral lesions of the hip“, „osteochondritis dissecans“, „early osteoarthritis of the hip“ und „early stage avascular necrosis“. Osteochondrale Verletzungen der Hüfte können einen erheblichen Schaden an der Gelenkoberfläche verursachen und die Lebensqualität verringern. Die Behandlung solcher Verletzungen kann sich schwierig gestalten, insbesondere bei jungen und aktiven Patienten. Zur Therapie chondraler und osteochondraler Verletzungen der Hüfte werden verschiedene Verfahren angewendet, so etwa Behandlungen mit mesenchymalen Stammzellen und zellbasierte Therapien, operative Eingriffe und Mikrofrakturierung. Auch ein Realignment der Knochenanatomie kann für optimale Behandlungsergebnisse nötig sein. Trotz mehrerer erfolgreicher Therapieverfahren fehlt es in der aktuellen Literatur an Direktvergleichen und Studien mit großen Stichproben. Weitere Studien sind erforderlich, um angemessene klinische Empfehlungen für die Behandlung chondraler bzw. osteochondraler Verletzungen des Hüftgelenks formulieren zu können.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chondral and osteochondral lesions encompass several acute or chronic defects of the articular cartilage and/or subchondral bone. The chondral lesions are located solely on the cartilage surface, whereas the osteochondral lesions are located in both cartilage and subchondral bone. Goyal et al. compared the subchondral bone-cartilage equilibrium to the soil-plant equilibrium. Soil provides plants with nutrients, provides a stable environment for their roots to grow in, and these roots of plants prevent soil erosion. The subchondral bone acts as rich soil for cartilage and bears its loads [1]. Damage to various tissues in the joint, including the subchondral bone below, may result from, be caused by, or happen simultaneously with damage to the articular surface [2]. These lesions arise from a wide range of pathologies, such as femoroacetabular impingement, developmental dysplasia of the hip, osteochondritis dissecans, osteochondral defects, osteochondral fractures, subchondral bone osteonecrosis, and insufficiency fractures [3]. Osteochondral lesions can be generated by both traumatic and atraumatic conditions damaging the cartilage and subchondral bone [4]. Chondral lesions cannot heal themselves completely. Due to the migration of bone marrow mesenchymal cells (BM-MSC) and the development of an inflammatory “super clot,” full-thickness lesions with subchondral bone involvement can heal to some extent. The freshly formed fibrocartilage tissue has a different structure to the initial hyaline articular cartilage. It is mostly made of type I collagen, while hyaline cartilage is mostly made of type II collagen [5]. These lesions frequently advance to osteoarthritis (OA), which is regarded as “an organic disease of the whole joint,” because cartilage has limited ability for regeneration and self-repair [2, 4]. Hip chondral lesions continue to be challenging to diagnose and treat for orthopedic surgeons. Imaging technology, arthroscopic equipment, and insights from fundamental science and clinical research have contributed to a substantial increase in hip arthroscopy procedures over the past decade. These factors have led to a rise in the detection and treatment of hip chondral lesions [6,7,8]. With the development of numerous technologies, the idea of joint preservation was introduced to avoid or slow the onset of osteoarthritis as well as to preserve or restore joint function in joints already afflicted by osteoarthritis. Over the last decade, intriguing innovative techniques based on novel tissue engineering techniques have been developed to address chondral/osteochondral lesions of the hip [4]. The current study discusses a comprehensive overview of the management of the osteochondral lesions hip, various pathological processes associated with the osteochondral lesions hip and the currently available treatment options.
Functional anatomy of the hip joint
The hip functions as a ball and socket joint during stance and walking to keep the torso balanced. The congruency of the articulating surfaces precludes femoral head and acetabulum translation. Strong articular congruency is provided by bone cartilage, the acetabular labrum, articular cartilage, the inner capsule, and surrounding musculature [9]. The cotyloid fossa comprises a combination of fibrofatty tissue and synovium lining. The depression of the cotyloid extends into the acetabular fossa. The articular surface of the acetabulum is an upside-down, cartilage-covered horseshoe. Hyaline cartilage covers the femoral head, excluding the fovea capitis femoris, a depression on the femoral head. This depression gives rise to the ligamentum teres femoris, which attaches medially to the transverse ligament and other tissues [10]. The articular surface of normal hips has variable hyaline cartilage thickness. The average cartilage thickness in the acetabulum is 3 mm, but it can vary between 1.5 and 5 mm. The deepest point of the cartilage in the centre of the femoral head ranges from 1.5 to 5 mm in thickness. The cartilage at the femoral head’s periphery has an average thickness of 1 mm, whereas the cartilage in the anterior, superior, and medial regions of the acetabulum has an average thickness of 1.3 mm [11, 12].
Osteochondral unit
Several components make up the articular joint, each playing a crucial role in its proper function. These elements include articular cartilage, bone, synovium, ligaments, capsule and labrum. The joint performs the critical functions of providing smooth mobility and weight-bearing support. Articular cartilage, in particular, is essential for these functions, and its homeostasis is maintained by the subchondral bone. The term osteochondral unit refers to this harmonious relationship that exists between articular cartilage and subchondral bone in a joint which is essential for both the weight bearing and the mobility of a joint. Preservation of this unit is necessary for joint health as osteochondral injury and degeneration can impair joint function. While some treatment techniques focus solely on repairing articular cartilage, subchondral bone must also be repaired for successful outcomes, because it serves a crucial part in the normal functioning of joint cartilage [13].
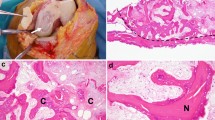
Histology
The joint contains the vital osteochondral unit consisting of hyaline cartilage and subchondral bone. Chondrocytes, which are responsible for cartilage metabolism, synthesize and degrade proteoglycans and collagens within the unit, which has four distinct layers across multiple zones. The radial zone, constituting the majority of the articular cartilage, boasts a well-developed rough endoplasmic reticulum and Golgi apparatus, while a tidemark separates it from the calcified zone. The subchondral osteochondral bone, made up of metaphyseal trabecular bone, has small holes through which blood vessels penetrate the calcified layer. It effectively absorbs loads, enabling the transmission and distribution of the cartilage matrix [14]. A schematic representation of the chondral layers is shown in Fig. 1.
Physiology and pathophysiology
The joint cartilage and the subchondral bone that form the osteochondral unit maintain the joint’s equilibrium. In normal conditions only 1–3% of the load is absorbed by cartilage but microfractures and other damage caused by FAI or dysplasia of the hip can lead to abnormal remodelling and a loss of its shock-absorbing ability, resulting in cartilage degeneration. Cartilage is nourished by two main methods: diffusion through synovial fluid in the superficial layer and vascularity in the deep calcified layer. The canalicular/lacunar network transports larger molecules, which are required for appropriate cartilage nourishment and repair [15].
Pathogenesis of chondral/osteochondral lesions
The pathogenesis of chondral and osteochondral lesions involves a complex interplay of mechanical, biochemical, and cellular factors. The initial insult often involves a traumatic event, such as a sports injury or a sudden impact, which causes damage to the cartilage and underlying bone [16, 17]. An injury to the chondral tissue of the hip joint can be caused by damage to the acetabular labrum. By stopping the leakage of joint fluid and functioning as a blocking mechanism for the interstitial fluid content, the labrum plays an essential part in the preservation of the structural integrity of the joint [18]. This trauma disrupts the smooth and frictionless surface of the cartilage, leading to the release of inflammatory mediators and activation of various cellular processes. Over time, the damaged cartilage undergoes degeneration and loss, resulting in compromised joint function. Furthermore, the altered biomechanics and increased stress on the affected area contribute to the development of osteoarthritis [16, 17].
Etiology
Chondral and osteochondral lesions in the hip can result from a variety of conditions, including femoroacetabular impingement (FAI), developmental dysplasia (DDH), avascular necrosis (AVN) and osteochondritis dissecans (OCD), and joint infection, rheumatic disease. Traumatic injuries such as hip joint dislocation, femoral head fracture, acetabular fracture or osteoarthritis can also cause these lesions.
FAI is one of the hip disorders caused by cam or pincer deformities. Cam impingement damages the anterosuperior and lateral acetabulum, while pincer lesions cause circumferential damage to the acetabular cartilage. FAI can also be caused by version abnormalities of the acetabulum or femur. The abnormal contact between the femoral head and the acetabulum in FAI results in mechanical stress on the articular cartilage, impaired blood flow, an inflammatory response, and altered joint biomechanics. These factors contribute to chondral damage, including fissuring, delamination, cartilage fibrillation, and the formation of osteochondral lesions. Understanding the mechanisms by which FAI produces these lesions is essential for appropriate management [19, 20].
In DDH, the shallow acetabulum fails to adequately cover and support the femoral head, leading to increased stress concentration on weight-bearing regions of the articular cartilage. This abnormal biomechanics cause repetitive microtrauma and friction between the femoral head and acetabulum, resulting in chondral damage. The instability of the hip joint in DDH further increases the risk of chondral and osteochondral lesions due to excessive movement and subluxation. These abnormal movements generate shear forces and impact stresses on the articular cartilage, leading to chondral injuries. Repeated subluxation or dislocation events can also cause osteochondral lesions, affecting both the cartilage and underlying bone. The presence of chondral and osteochondral lesions perpetuates joint instability, deformity, and abnormal loading, progressing the disease [21, 22].
In slipped capital femoral epiphysis (SCFE), the altered biomechanics due to femoral head displacement cause abnormal stress and shear forces within the hip joint. These forces can damage the articular cartilage, leading to chondral lesions. Additionally, the femoral head displacement can disrupt blood supply, resulting in avascular necrosis (AVN), which leads to bone and cartilage damage, causing osteochondral lesions. The development of chondral and osteochondral lesions in SCFE is influenced by factors such as slip severity, duration, and patient characteristics [23, 24].
Legg-Calvé-Perthes (LCP) disease, a pediatric hip disorder, leads to chondral and osteochondral lesions. It involves disrupted blood supply to the femoral head, causing AVN and structural changes. Ischemia leads to bone cell death, microfractures, and resorption. Revascularization occurs, but the regenerated bone may be weak and prone to fractures. Altered biomechanics and irregularities in the femoral head result in cartilage thinning and fibrillation. Abnormal contact pressures cause further cartilage damage and osteochondral lesions. Early diagnosis and management are vital to minimize long-term effects [25,26,27].
In the case of AVN, the compromised blood supply can lead to the death of osteocytes, which are the bone cells responsible for maintaining the structure and integrity of the bone tissue. The loss of osteocytes weakens the affected bone, making it more prone to damage. The progression of AVN involves the formation of microfractures within the necrotic bone. These microfractures disrupt the continuity of the bone structure and can extend to involve the overlying articular cartilage. As a result, chondral and osteochondral lesions can develop. The mechanical stress placed on the compromised bone and cartilage can further contribute to the development of chondral and osteochondral lesions. The altered biomechanics and increased load-bearing demands on the affected joint can lead to cartilage degeneration and wear. Over time, this can result in the loss of articular cartilage, exposing the underlying bone and leading to the formation of osteochondral lesions. It is important to note that AVN and its association with chondral and osteochondral lesions can vary depending on the specific location and extent of the AVN, as well as individual patient factors [28,29,30].
In the hip joint, OCD is very rare but it can produce chondral and osteochondral lesions through several mechanisms. The initial insult often involves repetitive trauma or microtrauma to the joint, which disrupts the blood supply to the subchondral bone and overlying cartilage. This compromised blood flow can lead to ischemia, resulting in the degeneration and weakening of the affected area. As a result, the affected cartilage and underlying bone become susceptible to damage. The mechanical forces exerted on the hip joint during weight-bearing activities further contribute to the development of chondral and osteochondral lesions. Over time, the weakened area can undergo further degeneration, leading to the detachment of a fragment of cartilage and bone [31, 32].
Classification
Chondral damage can be categorized in different ways, which, along with the size of the damage, can help figure out the best way to treat it. Outerbridge’s classification system, developed in 1961, is based on the severity of cartilage disruption and is widely used to grade chondral lesions [33]. Beck et al. developed a modified Outerbridge’s classification system that includes a grade 0 for normal cartilage and adds subgrades to grade III [34]. The classification system of the International Cartilage Repair Society (ICRS) classifies lesions according to their appearance, location, and depth. The appearance and location can be determined with MRI and X-ray, but the depth can only be determined with intraoperative findings [35]. Konan et al. proposed an expanded classification system that includes the six acetabular zones defined by Ilizaliturri et al. and the size of the lesion. This system is particularly useful for diagnosing and treating FAI pathology [36]. Additionally, Sampson created two classification systems for cartilage lesions, one for the femoral head and the other for the acetabulum, and suggested treatment protocols based on these classifications [37]. Table 1 describes various classifications used for chondral lesions.
Clinical assessment
A comprehensive clinical assessment is essential in the diagnosis of hip disorders and associated chondral/osteochondral injuries. The clinical manifestations of hip disorders such as FAI, dysplasia, osteochondritis dissecans, and AVN femoral head that cause chondral injury and hip discomfort vary. Unfortunately, patients with FAI wait an average of 4.2 months before seeking medical attention, and 3 years before receiving a diagnosis. In addition, approximately 13% of patients undergo operations that fail to treat the underlying hip disorder. Importantly, chondral injuries may be a consequence rather than a cause of the hip disorder [38]. Patient medical history, including prior injuries, hip conditions during childhood, athletic activities, and past surgical procedures, provides valuable insights into potential underlying causes and influences treatment options. A thorough physical examination is performed, including range of motion assessment, provocative tests, palpation, and neurovascular evaluation. These evaluations aid in identifying associated symptoms, joint instability, and mechanical issues [39].
Radiological assessment
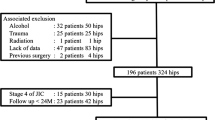
The hip joint is evaluated using a variety of imaging techniques. The acetabular index (AI) and lateral center-edge angle (LCEA) are essential parameters to take into account when interpreting anteroposterior (AP) pelvic radiographs ([40]; Fig. 2a). False profile radiography helps evaluate posterior degenerative joint changes and anterior femoral head coverage, which can be measured by calculating the anterior centre-edge angle (ACEA) ([41]; Fig. 2b).
a AP pelvic radiograph shows LCEA on the right hip; The LCEA is the angle between the vertical line from the femoral head center and the line connecting the lateral margin of the acetabulum. b The right hip false profile radiograph shows ACEA; The ACEA is the angle between the vertical line from the center of the femoral head and the posterior margin of the acetabulum.
The Dunn view is commonly employed to evaluate the sphericity of the femoral head in patients suspected of having FAI ([42]; Fig. 3). The alpha angle measures cam lesions, but other anatomical parameters can also affect clinical significance [43]. Other radiographic tools such as the cross-table lateral view and the frog-leg lateral view are also useful in evaluating FAI [44]. These tools aid in diagnosing and treating conditions affecting the hip joint.
Diagrammatic representation of radiographs of 45° Dunn’s view (a) and a 90° Dunn’s view (b). The alpha angle is formed by two lines. One line connects the center of the femoral neck’s long axis to the center of the femoral head. Another line goes from the center of the femoral head to the location on the anterolateral head-neck junction. This is the point where the radius of the femoral head starts to increase beyond the radius that is typically found more centrally in the acetabulum, where the head is more spherical. It is a measure of the asphericity of the femoral head and neck
CT is a highly effective imaging technique for evaluating the alignment of bones and detecting osteochondral injuries around the hip [45]. This method allows for accurate measurement of the extent to which the subchondral bone is involved and assessment of areas of irregularity around the junction of the femoral head and neck [46]. When combined with three-dimensional reformatting, CT provides an advantage over plain radiography and MRI in identifying both intra-articular and extra-articular impingement, including subspinal impingement [47]; however, it is important to note that while the numerical values of angle measurements used to diagnose abnormalities in coverage are based on plain X‑ray imaging, they do not correspond with the center-edge angle measurements obtained from coronal and sagittal CT slices [48].
Magnetic resonance imaging (MRI) is a most useful nonradiation method for assessing nontraumatic osteochondral pathologies of the hip joint. It can identify injuries to the labrum and areas of bony edema linked to intra-articular impingement. The latest high-field MRI technology can detect abnormalities without the need for contrast agents. To examine and define osteochondral abnormalities, several techniques, such as true proton density and T2-weighted turbo spin-echo are employed. Additionally, advanced techniques like T2 relaxation time and delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) can be used to evaluate cartilage abnormalities [49].
Treatment of underlying causes
In cases of FAI treatment options range from nonsurgical to surgical interventions. Nonsurgical approaches encompass physical therapy to enhance hip flexibility and strength, injections for inflammation reduction, and activity modification. Surgical treatment includes hip arthroscopy or open hip surgery for decompressing the bony prominence around the rim and at the femoral head neck junction. Optimal treatment depends on FAI severity and patient-specific considerations [50].
The treatment of DDH varies by age and severity. A Pavlik harness is common for infants. Surgical options for older children include closed/open reduction, osteotomy, or arthroscopy, aiming to normalize femoral head coverage and address labral injury. Surgical selection considers age, CE angle, and OA grade for optimal outcomes [51].
Treatment for slipped capital femoral epiphysis (SCFE) primarily involves surgery to stabilize the hip joint and prevent further slippage. Surgical options vary based on the severity: mild cases may require a single screw across the growth plate, while severe cases may involve multiple screws or an osteotomy. After surgery, cast/brace use aids healing, and physical therapy restores hip joint mobility. Recognition of labral injury, hip dysplasia, patient age, CE angle, and OA grade guides surgical treatment selection for optimal outcomes [52].
Surgical intervention is often necessary for young adult patients of Legg-Calvé-Perthes disease with worsening hip pain and dysfunction caused by hip articulation deformities. Treatment may involve proximal femoral osteotomy or pelvis osteotomy to restore normal femoral head coverage. In addition, when performing surgical dislocation with the trochanter, concurrent relative neck lengthening may be considered [27].
To treat osteochondral lesions in AVN of the hip, various approaches are available, including core decompression, osteochondral autograft transplantation, and total hip arthroplasty depending on the Association Research Circulation Osseous (ARCO) classification [53].
Treatment for osteochondritis dissecans (OCD) of the hip varies is based on lesion size, location, patient age, and symptom severity. Rest, physical therapy, and injections can be initial approaches. Surgery is considered if conservative methods fail or for severe cases. Surgical options include microfracture, autologous chondrocyte transplantation (ACT), and osteochondral autograft transplantation (OAT) based on lesion specifics [32].
Treatment of chondral/osteochondral lesions
It is important not only to treat the chondral/osteochondral lesions but also to treat the underlying cause of the lesion. For example, if the lesion is caused by labral tears, surgery may be needed to repair the labrum and if the lesion is caused by FAI, surgery may be needed to correct the deformity.
Hip chondral/osteochondral lesions can be treated using various methods, which can be broadly categorized into conservative, less invasive approaches and more complex procedures. Treatment decisions depend on factors, such as patient symptoms, lesion size, and activity level. Treatment algorithms have been developed to guide these decisions and provide tailored treatments.
Conservative
Conservative treatment for chondral/osteochondral lesions of the hip involves nonsurgical approaches aimed at reducing symptoms, promoting healing, and improving joint function. Conservative treatment for chondral/osteochondral lesions of the hip is indicated in cases of mild to moderate symptoms, stable and small lesions, absence of mechanical symptoms, and when the patient prefers nonsurgical options [54]. These options include patient education, pain medication, physical therapy, and muscle strengthening.
-
Patient education: providing information and education to patients about their condition, including the nature of the hip pain and strategies for symptom management.
-
Symptom control: the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to help reduce pain and inflammation associated with hip pain.
-
Identification and modification of aggravating activities: identifying activities that worsen symptoms and modifying or avoiding them to reduce stress on the hip joint.
-
Physical therapy interventions: physical therapy programs aimed at addressing neuromuscular deficits, strengthening the hip and lumbopelvic regions, improving core stability, and enhancing flexibility and range of motion. These may include exercises targeting hip musculature, pelvic positioning, core muscle strengthening, neuromuscular training, stretching, manual therapy, dynamic biomechanical control, and gait training.
-
Dynamic stabilization: establishing dynamic stabilization of the hip musculature, core, and pelvic regions to prevent excessive hip joint motion during activities.
Biologics
Biological treatments provide promising options for managing chondral and osteochondral lesions of the hip by promoting the regeneration of damaged joint tissue (Table 2). Hyaluronic acid (HA) injections have been found to be effective in managing chondral lesions of the hip by facilitating the regeneration of articular cartilage and promoting the healing process. HA injections not only provide lubrication and cushioning but also stimulate the production of chondrocytes, which are crucial for the formation of cartilage. By promoting the growth of new cartilage tissue, HA injections aid in repairing and restoring damaged areas of the hip joint. In cases where conservative treatments have failed to provide relief, HA injections can play a significant role in managing chondral lesions of the hip. Although HA injections may not provide a cure for hip chondral lesions, they can offer substantial relief from symptoms and help enhance joint function and overall quality of life [55,56,57].
PRP therapy is a non-immunogenic treatment derived from the patient’s own blood, where platelets are concentrated in a small volume of plasma, typically 3–6 times higher than baseline [58]. This therapy offers several advantages, including quick preparation and simplicity in its technique. Being autologous in nature, PRP therapy carries a distinct safety profile, as it lacks many of the side effects and interactions associated with pharmaceutical drugs [59]. PRP has been investigated as a potential treatment option for chondral and osteochondral lesions of the hip, although research in this area is limited. Animal studies have shown promising results with intra-articular injections of PRP and autologous conditioned plasma, as well as the use of platelet-enriched fibrin scaffolds [60]; however, there have been no published studies on the use of PRP for chondral defects in human subjects. The studies which examined the effects of PRP for hip osteoarthritis (OA) showed lower pain scores and better functional outcomes [61, 62].
The distinction between stem cells and bone marrow aspirate concentrate (BMAC) is that stem cells are undifferentiated cells with the ability to differentiate into various cell types, whereas BMAC is the concentration of stem cells, growth factors, and cytokines found in the bone marrow. BMAC contains a high number of stem cells, ranging from 0.001% to 0.01% [63]. To increase stem cell concentrations, they are isolated from bone marrow aspirate, seeded, and expanded for 2–6 weeks [63]. The optimal dose, frequency, and number of injections are still uncertain, but some studies indicate that higher concentrations of stem cells can lead to better clinical results [64]. MSCs can be used in the treatment of osteochondral defects with both reparative and preventative effects [65]. Gobbi et al. (2019) used expanded MSCs to treat chondral defects in 20 patients and reported significant improvements in clinical outcomes and MRI showing good to excellent repair tissue [66]. Centeno et al. (2018) reported better clinical outcomes with BMAC treatment for the treatment of knee osteoarthritis [67]. Based on these studies, stem cells and BMAC may be an effective treatment option for chondral and osteochondral lesions in the hip joint.
Surgery
Surgical treatments play a crucial role in addressing chondral and osteochondral lesions of the hip, offering a range of techniques and approaches to restore joint function and alleviate symptoms (Table 3). Chondroplasty is a widely used technique in hip arthroscopy that involves the smoothing of areas with unstable chondral flaps (mostly acetabular lesions), preventing the development of loose bodies and removing potential mechanical blocks in the joint. This method is preferred for treating low-grade and partial thickness chondral injuries and has been proven successful in such cases [68]; however, studies have indicated that performing chondroplasty during hip arthroscopy may increase the likelihood of conversion to total hip replacement in patients of all ages [69]. Chondroplasty should not be performed on advanced arthritis that requires total hip arthroscopy and should be preferentially carried out on patients with pre-existing OA [69]. It is also important to avoid using radiofrequency ablation devices around chondral tissue, as they can damage chondrocytes [70]. Chondroplasty is the most commonly performed procedure in hip arthroscopy, accounting for 49.3% of cases [68]. Good clinical outcomes have been observed with chondroplasty, making it a satisfactory treatment strategy for low-grade and partial thickness chondral injuries [68]; however, the decision to perform chondroplasty should be made on a case by case basis, taking into account the patient’s age, overall joint health, and the severity of the injury.
Cartilage delamination flaps can be repaired surgically with sutures. Sekiya et al. performed arthroscopic microfracture and suture repair of delaminated cartilage flap and reported good outcomes measured by modified Harris hip score and hip outcome scores [71]. Tzaveas et al. conducted a study on the efficacy of fibrin adhesive for arthroscopic repair of chondral delamination lesions. They found promising short-term results, with intact chondral repairs in cases that underwent revision arthroscopy [72].
Microfracture is a minimally invasive procedure used to treat osteochondral lesions in the hip. This technique involves the creation of small holes in the affected bone to stimulate the formation of fibrocartilage. The success of microfracture depends on factors such as the size and location of the lesion, as well as the patient’s age and level of physical activity. Although the formation of fibrocartilage is a potential limitation, microfracture remains a viable option for many patients and can be performed on an outpatient basis [73]. Various studies reported good outcomes following microfracture [74, 75]. Microfracture offers several advantages, including its relatively low cost and the fact that it is not considered a technically challenging procedure;however, it is important to consider the potential risks associated with microfracture. These risks include the possibility of ossification, fragility of the newly formed tissue, imperfections in the regenerated cartilage, inadequate filling of the lesion, and the susceptibility of the new cartilage to breakdown over time [76].
The repair tissue formed following microfracture has inferior properties compared to normal hyaline cartilage, leading to concerns about its long-term durability. In order to improve the outcomes of the microfracture procedure, several augmentation strategies have been developed. The use of implantable scaffolds can help maintain the fibrin clot within the defect, facilitate cell adhesion and migration, and improve integration with the surrounding cartilage. Animal models and early clinical trials have shown promising results in terms of improving the quality of the repair tissue [77, 78]. Another approach is the use of growth factors to enhance the microfracture repair. Bone morphogenetic proteins (BMPs), such as BMP‑7 and BMP‑4 and cytokine modulation, specifically interleukin‑1 receptor antagonist (IL-1ra) have been investigated for their ability to promote chondrogenesis and improve the properties of the repair tissue [79,80,81,82]. Other techniques involve the combination of scaffold implants with cultured chondrocytes or the use of HA to further enhance the repair process [80].
Adipose-derived stem cells (ADSC) have the ability to differentiate into various cell types, including bone and cartilage [83]. They are easier to isolate in larger quantities with minimal donor site morbidity compared to bone marrow. ADSCs also exhibit a higher proliferation rate compared to BM-MSCs [83]. ADSCs can be isolated from fat through mechanical or enzymatic processes [84]. One mechanical method uses a fat-processing device (Lipogem) that isolates the cellular component of harvested autologous fat, generating micronized fat that can be injected into the joint [85]. Lipogems has demonstrated the ability to yield higher amounts of progenitor cells and MSCs compared to normal lipoaspirate [86]. Even though there are limited studies on Lipogems in hip treatment, they reported improved clinical outcomes with higher mHHS scores [87, 88]. No complications or difficulties with liposuction were reported in both studies. ADSCs offer a potentially safer and easier alternative to BM-MSCs for treating small acetabular chondral defects during hip arthroscopy; however, further studies are needed to determine the specific indications for each technique [86].
Articular cartilage injuries that are too large for microfracture can be treated with autologous chondrocyte implantation (ACI), a two-stage surgical technique that involves removing the damaged cartilage and microfracturing the defect before implanting previously harvested chondrocytes mixed with a bioabsorbable matrix [89]. Limited reports exist on the use of ACI in the hip, primarily due to difficulties with harvest and the need for a surgical procedure on an unaffected joint. However, Akimau et al. [90] described a case of ACI in a 31-year-old male with femoral head osteonecrosis, resulting in improved HHS and functional outcomes. Similarly, Fontana et al. [91] conducted a retrospective study comparing ACI to debridement, showing significantly better HHS outcomes in the ACI group after approximately 5 years of follow-up. However, the formation of viable cartilage was not confirmed in this study. These findings suggest that ACI may be a beneficial treatment option for chondral lesions in the hip, while arthroscopic debridement has limited utility, especially for larger lesions.
Autologous matrix-induced chondrogenesis (AMIC) is a surgical technique that involves the use of a type I/III collagen matrix in conjunction with microfracture to treat chondral defects of grades 3 and 4 that measure 2–4 cm2 [92]. During the procedure, the matrix is inserted into the joint using arthroscopy to cover the defect and stabilize the blood clot that results from microfracture, providing a framework for the formation of repair tissue [92]. Thier et al. [93] conducted a short-term study on arthroscopic injectable matrix-associated autologous chondrocyte implantation (MACI) for hip cartilage defects. Results showed improved patient outcomes in terms of activity level, quality of life, and pain reduction after a 19-month follow-up. Krueger et al. [94] evaluated the clinical outcome of arthroscopic matrix-associated injectable autologous chondrocyte implantation (ACI) for large acetabular cartilage defects. Findings revealed promising results with significant improvements in hip scores and subjective assessments after a 3-year follow-up, indicating the effectiveness of injectable ACI for weight-bearing zone defects.
The culture process involved in 3D-ACI generates redifferentiated autologous chondrocytes along with their extracellular matrix, resulting in scaffold-free 3D spheroids of neocartilage [95, 96]. These 3D constructs are injectable solutions, making the second step of chondrocyte implantation similar to injecting scaffolds into the defect site [95]. Studies evaluating the efficacy of 3D-ACI in the treatment of chondral defects in both the knee and hip have reported promising results [96, 97]. These investigations have demonstrated improved patient outcomes, such as increased mHHS and iHOT scores, and successful cartilage healing [97,98,99]. Even patients with larger defects have shown favorable results with the ease of application and adhesive properties of 3D-ACI [98]. While 3D-ACI appears to be a safe and effective treatment option for medium to large articular cartilage defects, further studies are required to assess its long-term benefits compared to the risks associated with longer culture times and the complexity of preparation, which may contribute to failure [95].
Autologous minced cartilage implantation (AMCI) has emerged as a promising technique for addressing acetabular cartilage lesions in patients with femoroacetabular impingement syndrome (FAIS). This innovative approach, described in recent studies by Zimmerer et al. [100] and Gebhardt et al. [101], involves arthroscopic preparation of the damaged cartilage, followed by mincing of autologous cartilage fragments using specialized instruments. These minced cartilage fragments, collected with the an autologous tissue collector (Graftnet™ system, Arthrex, Inc., FL, USA), are then augmented with autologous conditioned plasma (ACP) and implanted into the lesion site.
Osteochondral autograft transplantation (OAT) entails the transplantation of osteochondral plugs that are harvested from the nonweight-bearing surface to fill larger defects and is typically used when microfracture or other treatments have failed. On the other hand, mosaicplasty involves the transplantation of multiple smaller osteochondral plugs from a healthy articular surface to fill multiple smaller defects [102]. Mosaicplasty is often used in the knee and requires surgical hip dislocation when used in the hip. The technique has been utilized to address osteochondral defects in the femoral head, which has demonstrated the ability to enhance clinical outcomes and range of motion. The OAT can be performed either arthroscopically or through an open arthroscopic retrograde approach, depending on the placement of the defect. OAT has been shown to be efficacious in treating chondral lesions and osteonecrosis of the femoral head in the hip, leading to notable advancements in clinical scores. Recent studies have found that both mosaicplasty and OAT are effective in treating osteochondral defects, particularly in the femoral head. The studies report significant improvements in patient outcomes and pain relief with both procedures, although there may be a risk of subsequent hip arthroscopy with mosaicplasty. The disadvantages of OAT therapy include a relatively new procedure with limited long-term data, is not suitable for all, is not the treatment of choice for isolated full-thickness chondral defects at the hip, because of the unfavorable risk-benefit profile, can be technically demanding, and is not a permanent solution [102,103,104,105,106,107].
Osteochondral allograft transplantation (OCA) is a promising treatment option for osteochondral lesions of the hip, particularly for large defects that are difficult to treat with alternative techniques. OCA permits the replacement of a damaged joint surface with a single-stage technique that does not cause morbidity at the donor site. In addition, the application of OCA provides an instantly functional joint surface and can lead to the replacement of hyaline cartilage [108,109,110]. However, the survival of chondrocytes from the moment of graft procurement to the time of implantation can be affected by the length of storage time after graft procurement, with the survival of the graft being significantly diminished after 28 days of storage. Various studies have reported positive outcomes with the use of OCA transplantation for treating osteochondral defects in the hip joint. The use of fresh allografts has been found to avoid donor site morbidity, while the anterior approach allows faster rehabilitation and an earlier return to function. However, challenges with OCA transplantation include donor tissue matching, the timing of donation and implantation, limited supply of donor tissue, and potential nonunion or failure to transform into live tissue. Overall, while OCA transplantation may have advantages over other treatments, it is important to consider these challenges before deciding on a course of action [108,109,110].
Prosthetic biocomposites have emerged as a promising approach for the repair of osteochondral defects, offering potential solutions to the challenges associated with tissue regeneration. Several studies have explored the use of synthetic materials as scaffolds to guide tissue regeneration in osteochondral defect repair. One study by Frassica and Grunlan highlighted the importance of synthetic materials with instructive properties, which can influence cellular behavior and promote tissue growth [111]. They discussed the development of synthetic scaffolds with complex chemical and morphological features, prepared using various fabrication techniques, to restore both articular cartilage and underlying bone. Another review by Fu et al. summarized different scaffold types, such as porous, hydrogel, fibrous, and composite scaffolds, and evaluated their advantages and disadvantages in osteochondral tissue engineering [112]. They emphasized the challenges in achieving anatomical, biochemical, and biomechanical stratification in tissue regeneration. Additionally, Xu et al. focused on the construction of a bilayered composite scaffold using chitosan and chitosan-beta-tricalcium phosphate, which demonstrated chondrogenic and osteogenic abilities, leading to effective repair of osteochondral defects in a rat model [113].
Surgical recommendations
El Bitar et al. developed a straightforward algorithm to assist with decision-making in patients presenting with symptoms of full-thickness femoral head and acetabular lesions, given the wide range of surgical treatment options available. This algorithm can be helpful in planning surgical interventions for chondral lesions of the hip ([114]; Table 4).
Guidelines by the DGOU group for biologic reconstruction of full sized cartilage defects of the hip
The German Society of Orthopedics and Trauma (Deutsche Gesellschaft für Orthopädie und Unfallchirurgie, DGOU) has published guidelines for the biologic reconstruction of full-sized cartilage defects of the hip [115]. The guidelines were developed by the DGOU’s Group for Clinical Tissue Regeneration and the Hip Committee of the working group for arthroscopy and joint surgery (AGA) [115]. The guidelines recommend the treatment options for full-sized cartilage defects of the hip given in Table 5.
Postoperative management
Hip preservation surgery often involves a combination of procedures, and the postoperative rehabilitation plan should consider all concurrent disorders [116]. Chondroplasty generally does not require any postoperative restrictions, while microfracture procedures necessitate weight-bearing precautions to protect the affected area [116]. The duration of weight-bearing restrictions after microfracture can range from 2 to 8 weeks, after which patients gradually increase their weight-bearing to full weight [116]. Other procedures, such as AMIC/ACI, mosaicplasty, osteochondral transplantation, and articular cartilage repair, usually necessitate 6 weeks of touch-down weight bearing followed by 6 weeks of partial weight bearing [117]. However, rehabilitation protocols may vary depending on the surgeon’s preferences and the patient’s specific condition. Recent studies have suggested that immediate weight-bearing after microfracture may not compromise clinical outcomes [118, 119]. A systematic review found that weight-bearing restriction after microfracture may not provide additional benefits and that early rehabilitation may be beneficial for postoperative outcomes [119].
Conclusion
Osteochondral injuries in the hip are debilitating conditions that can significantly impair daily life and negatively impact the quality of life. These injuries often result in progressive joint damage, leading to end-stage osteoarthritis. Treating such injuries is especially challenging in young and active patients because the hip joint regularly handles significant stresses through an only weight-bearing compartment. To address these injuries, various strategies are used to repair or reconstruct chondral/osteochondral tissue. These include biological therapies (stem cells, scaffolds or cell-based therapies) which have shown promise in promoting healing and regeneration of damaged tissue. Realignment procedures surrounding the hip joint are also commonly necessary to optimize outcomes. Surgical procedures such as osteotomies and arthroscopies may be used to address these issues. While various treatment options have shown success, including repair, microfracture, autograft chondrocytes, and allograft transplants, there is still a lack of head-to-head comparisons and large sample sizes in the literature. Therefore, further research is needed to evaluate the efficacy of different treatments for managing chondral injuries of the hip joint and to develop appropriate clinical guidelines for patient care. Early detection and prompt management of these injuries are crucial to prevent irreversible joint damage and minimize the need for invasive surgical interventions. A multidisciplinary approach involving orthopedic surgeons, radiologists, and rehabilitation specialists is often required to achieve the best outcomes for patients with chondral/osteochondral injuries of the hip.
Abbreviations
- 3D-ACI:
-
Three-Dimensional Autologous Chondrocyte
- ACEA:
-
Anterior center-edge angle
- ACI:
-
Autologous chondrocyte implantation
- ACT:
-
Autologous chondrocyte transplantation
- ADSCs:
-
Adipose-derived stem cells
- AGA:
-
Arbeitsgemeinschaft für Arthroskopie und Gelenkchirurgie (German working party for arthroscopy and joint surgery)
- AI:
-
Acetabular index
- ALAD:
-
Acetabular labrum articular disruption
- AMIC:
-
Autologous matrix-induced chondrogenesis
- ARCO:
-
Association Research Circulation Osseous classification
- AVN:
-
Avascular necrosis
- BMAC:
-
Bone marrow aspirate concentrate
- BM-MSC:
-
Bone marrow mesenchymal cells
- CEA:
-
Center-edge angle
- CT:
-
Computed tomography
- DDH:
-
Developmental dysplasia
- DGEMRIC:
-
Delayed gadolinium-enhanced magnetic resonance imaging of cartilage
- DGOU:
-
Deutsche Gesellschaft für Orthopädie und Unfallchirurgie (German Society of Orthopedics and Trauma)
- FAI:
-
Femoroacetabular impingement
- HA:
-
Hyaluronic acid
- ICRS:
-
International Cartilage Repair Society
- iHOT:
-
International hip outcome tool
- IL-1ra:
-
Interleukin-1 Receptor Antagonist
- LCEA:
-
Lateral center-edge angle
- LCP:
-
Legg-Calvé-Perthes
- MACT:
-
Matrix-assisted autologous chondrocyte transplantation
- MATT:
-
Microfragmented adipose tissue transplantation
- MMHS:
-
Modified Harris hip score
- MRI:
-
Magnetic resonance imaging
- MSCs:
-
Mesenchymal stem cells
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- OA:
-
Osteoarthritis
- OAT:
-
Osteochondral autograft transfer
- OCA:
-
Osteochondral allograft transplantation
- OCD:
-
Osteochondritis dissecans
- OCL:
-
Osteochondral lesion
- PRP:
-
Platelet-rich plasma
- SCFE:
-
Slipped capital femoral epiphysis
References
Goyal D, Goyal A, Adachi N (2017) Subchondral bone: healthy soil for the healthy cartilage. In: Gobbi A, Espregueira-Mendes J, Lane JG, Karahan M (eds) Bio-orthopaedics, vol 14. Springer, Berlin/ Heidelberg, pp 479–486 https://doi.org/10.1007/978-3-662-54181-4_38
Lepage SIM, Robson N, Gilmore H, Davis O, Hooper A, John StS, Kamesan V, Gelis P, Carvajal D, Hurtig M, Koch TG (2019) Beyond cartilage repair: the role of the osteochondral unit in joint health and disease. Tissue Eng Part B Rev 25(2):114–125. https://doi.org/10.1089/ten.TEB.2018.0122
Gorbachova T, Melenevsky Y, Cohen M, Cerniglia BW (2018) Osteochondral lesions of the knee: differentiating the most common entities at MRI. Radiographics 38(5):1478–1495. https://doi.org/10.1148/rg.2018180044
Vilela CA, da Silva Morais A, Pina S, Oliveira JM, Correlo VM, Reis RL, Espregueira-Mendes J (2018) Clinical trials and management of osteochondral lesions. Adv Exp Med Biol 1058:391–413. https://doi.org/10.1007/978-3-319-76711-6_18
Bae DK, Yoon KH, Song SJ (2006) Cartilage healing after microfracture in osteoarthritic knees. Arthroscopy 22(4):367–374. https://doi.org/10.1016/j.arthro.2006.01.015
Bedard NA, Pugely AJ, Duchman KR, Westermann RW, Gao Y, Callaghan JJ (2016) When hip scopes fail, they do so quickly. J Arthroplasty 31(6):1183–1187. https://doi.org/10.1016/j.arth.2015.12.024
Kemp JL, Makdissi M, Schache AG, Pritchard MG, Pollard TC, Crossley KM (2014) Hip chondropathy at arthroscopy: prevalence and relationship to labral pathology, femoroacetabular impingement and patient-reported outcomes. Br J Sports Med 48(14):1102–1107. https://doi.org/10.1136/bjsports-2013-093312
Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL (2015) Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy 31(12):2307–2313.e2. https://doi.org/10.1016/j.arthro.2015.06.008
Bowman KF Jr, Fox J, Sekiya JK (2010) A clinically relevant review of hip biomechanics. Arthroscopy 26(8):1118–1129. https://doi.org/10.1016/j.arthro.2010.01.027
Blankenbaker DG, De Smet AA (2010) Hip injuries in athletes. Radiol Clin North Am 48(6):1155–1178. https://doi.org/10.1016/j.rcl.2010.07.003
Wyler A, Bousson V, Bergot C, Polivka M, Leveque E, Vicaut E, Laredo JD (2007) Hyaline cartilage thickness in radiographically normal cadaveric hips: comparison of spiral CT arthrographic and macroscopic measurements. Radiology 242(2):441–449. https://doi.org/10.1148/radiol.2422051393
Armstrong CG, Gardner DL (1977) Thickness and distribution of human femoral head articular cartilage. Changes with age. Ann Rheum Dis 36(5):407–412. https://doi.org/10.1136/ard.36.5.407
Nakasa T, Adachi N (2022) The osteochondral unit. In: Gobbi A, Lane JG, Longo UG, Dallo I (eds) Joint function preservation. Springer, Cham https://doi.org/10.1007/978-3-030-82958-2_7
Goldring SR, Goldring MB (2004) The role of cytokines in cartilage matrix degeneration in osteoarthritis. Clin Orthop Relat Res 427 Suppl:S27–S36. https://doi.org/10.1097/01.blo.0000144854.66565.8f
Buckwalter JA (2002) Articular cartilage injuries. Clin Orthop Relat Res 402:21–37. https://doi.org/10.1097/00003086-200209000-00004
Buckwalter JA, Mankin HJ (1998) Articular cartilage: tissue design and chondrocyte-matrix interactions. Instr Course Lect 47:477–486
Hunziker EB (2002) Articular cartilage repair: basic science and clinical progress. A review of the current status and prospects. Osteoarthritis Cartilage 10(6):432–463. https://doi.org/10.1053/joca.2002.0801
Philippon MJ, Nepple JJ, Campbell KJ, Dornan GJ, Jansson KS, LaPrade RF, Wijdicks CA (2014) The hip fluid seal—Part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc 22(4):722–729. https://doi.org/10.1007/s00167-014-2874-z
Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH (2013) Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis 72(6):918–923. https://doi.org/10.1136/annrheumdis-2012-201643
Philippon MJ, Briggs KK, Carlisle JC, Patterson DC (2013) Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res 471(8):2492–2496. https://doi.org/10.1007/s11999-012-2779-4
Bohaček I, Plečko M, Duvančić T, Smoljanović T, Vukasović Barišić A, Delimar D (2020) Current knowledge on the genetic background of developmental dysplasia of the hip and the histomorphological status of the cartilage. Croat Med J 61(3):260–270. https://doi.org/10.3325/cmj.2020.61.260
Zhu J, Fernando ND (2020) Classifications in brief: the hartofilakidis classification of developmental dysplasia of the hip. Clin Orthop Relat Res 478(1):189–194. https://doi.org/10.1097/CORR.0000000000000802
Novais EN, Millis MB (2012) Slipped capital femoral epiphysis: prevalence, pathogenesis, and natural history. Clin Orthop Relat Res 470(12):3432–3438. https://doi.org/10.1007/s11999-012-2452-y
Samelis PV, Papagrigorakis E, Konstantinou AL, Lalos H, Koulouvaris P (2020) Factors affecting outcomes of slipped capital femoral epiphysis. Cureus 12(2):e6883. https://doi.org/10.7759/cureus.6883
Kim HK (2010) Legg-Calvé-Perthes disease. J Am Acad Orthop Surg 18(11):676–686. https://doi.org/10.5435/00124635-201011000-00005
Rosenfeld SB, Herring JA, Chao JC (2007) Legg-calve-perthes disease: a review of cases with onset before six years of age. J Bone Joint Surg Am 89(12):2712–2722. https://doi.org/10.2106/JBJS.G.00191
Rodríguez-Olivas AO, Hernández-Zamora E, Reyes-Maldonado E (2022) Legg-Calvé-Perthes disease overview. Orphanet J Rare Dis 17(1):125. https://doi.org/10.1186/s13023-022-02275-z
Petek D, Hannouche D, Suva D (2019) Osteonecrosis of the femoral head: pathophysiology and current concepts of treatment. EFORT Open Rev 4(3):85–97. https://doi.org/10.1302/2058-5241.4.180036
Mollazadeh S, Fazly Bazzaz BS, Kerachian MA (2015) Role of apoptosis in pathogenesis and treatment of bone-related diseases. J Orthop Surg Res 10:15. https://doi.org/10.1186/s13018-015-0152-5
Vicaş RM, Bodog FD, Fugaru FO, Grosu F, Badea O, Lazăr L, Cevei ML, Nistor-Cseppento CD, Beiuşanu GC, Holt G, Voiţă-Mekereş F, Buzlea CD, Ţica O, Ciursaş AN, Dinescu SN (2020) Histopathological and immunohistochemical aspects of bone tissue in aseptic necrosis of the femoral head. Rom J Morphol Embryol 61(4):1249–1258. https://doi.org/10.47162/RJME.61.4.26
Siebenrock KA, Powell JN, Ganz R (2010) Osteochondritis dissecans of the femoral head. Hip Int 20(4):489–496. https://doi.org/10.1177/112070001002000412
Edmonds EW, Heyworth BE (2014) Osteochondritis dissecans of the shoulder and hip. Clin Sports Med 33(2):285–294. https://doi.org/10.1016/j.csm.2013.11.001
R E OUTERBRIDGE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43-B:752–757. https://doi.org/10.1302/0301-620X.43B4.752
Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R (2004) Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res 418:67–73
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A(Suppl 2):58–69. https://doi.org/10.2106/00004623-200300002-00008
Konan S, Rayan F, Meermans G, Witt J, Haddad FS (2011) Validation of the classification system for acetabular chondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br 93(3):332–336. https://doi.org/10.1302/0301-620X.93B3.25322
Sampson TG (2011) Arthroscopic treatment for chondral lesions of the hip. Clin Sports Med 30(2):331–348. https://doi.org/10.1016/j.csm.2010.12.012
Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT (2007) Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy 23(12):1295–1302. https://doi.org/10.1016/j.arthro.2007.09.015
Reiman MP, Thorborg K (2014) Clinical examination and physical assessment of hip joint-related pain in athletes. Int J Sports Phys Ther 9(6):737–755
Ackermann J, Liebmann F, Hoch A, Snedeker J, Farshad M, Rahm S, Zingg P, Fürnstahl P (2021) Augmented reality based surgical navigation of complex pelvic osteotomies—A feasibility study on cadavers. Appl Sci 11:1228. https://doi.org/10.3390/app11031228
Akiho S, Yamamoto T, Kinoshita K, Matsunaga A, Ishii S, Ishimatsu T (2017) The utility of false-profile radiographs for the detection of osteoarthritis progression in acetabular dysplasia. JB JS Open Access 2(4):e23. https://doi.org/10.2106/JBJS.OA.17.00023
Maupin JJ, Steinmetz G, Thakral R (2019) Management of femoroacetabular impingement syndrome: current insights. Orthop Res Rev 11:99–108. https://doi.org/10.2147/ORR.S138454
Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J (2002) The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 84(4):556–560. https://doi.org/10.1302/0301-620x.84b4.12014
Meyer DC, Beck M, Ellis T, Ganz R, Leunig M (2006) Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res 445:181–185. https://doi.org/10.1097/01.blo.0000201168.72388.24
Christie-Large M, Tapp MJ, Theivendran K, James SL (2010) The role of multidetector CT arthrography in the investigation of suspected intra-articular hip pathology. Br J Radiol 83(994):861–867. https://doi.org/10.1259/bjr/76751715
Stevens K, Tao C, Lee SU, Salem N, Vandevenne J, Cheng C, Neumann G, Valentin-Opran A, Lang P (2003) Subchondral fractures in osteonecrosis of the femoral head: comparison of radiography, CT, and MR imaging. AJR Am J Roentgenol 180(2):363–368. https://doi.org/10.2214/ajr.180.2.1800363
Nazaroff J, Mark B, Learned J, Wang D (2021) Measurement of acetabular wall indices: comparison between CT and plain radiography. J Hip Preserv Surg 8(1):51–57. https://doi.org/10.1093/jhps/hnab008
Huellner MW, Strobel K (2014) Clinical applications of SPECT/CT in imaging the extremities. Eur J Nucl Med Mol Imaging 41(Suppl 1):S50–S58. https://doi.org/10.1007/s00259-013-2533-5
Zilkens C, Miese F, Jäger M, Bittersohl B, Krauspe R (2011) Magnetic resonance imaging of hip joint cartilage and labrum. Orthop Rev 3(2):e9. https://doi.org/10.4081/or.2011.e9
Anzillotti G, Iacomella A, Grancagnolo M, Bertolino EM, Marcacci M, Sconza C, Kon E, Di Matteo B (2022) Conservative vs. surgical management for femoro-acetabular impingement: a systematic review of clinical evidence. J Clin Med 11(19):5852. https://doi.org/10.3390/jcm11195852
Hooper N, Aroojis A, Narasimhan R, Schaeffer EK, Habib E, Wu JK, Taylor IK, Burlile JF, Agrawal A, Shea K, Mulpuri K (2020) Developmental dysplasia of the hip: an examination of care practices of orthopaedic surgeons in India. Indian J Orthop 55(1):158–168. https://doi.org/10.1007/s43465-020-00233-0
Peck DM, Voss LM, Voss TT (2017) Slipped capital femoral epiphysis: diagnosis and management. Am Fam Physician 95(12):779–784
Yoon BH, Mont MA, Koo KH, Chen CH, Cheng EY, Cui Q, Drescher W, Gangji V, Goodman SB, Ha YC, Hernigou P, Hungerford MW, Iorio R, Jo WL, Jones LC, Khanduja V, Kim HKW, Kim SY, Kim TY, Lee HY, Lee MS, Lee YK, Lee YJ, Nakamura J, Parvizi J, Sakai T, Sugano N, Takao M, Yamamoto T, Zhao DWT (2020) 2019 revised version of association research circulation osseous staging system of osteonecrosis of the femoral head. J Arthroplasty 35(4):933–940. https://doi.org/10.1016/j.arth.2019.11.029
McGovern RP, Martin RL, Kivlan BR, Christoforetti JJ (2019) Non-operative management of individuals with non-arthritic hip pain: a literature review. Int J Sports Phys Ther 14(1):135–147
Migliore A, Bizzi E, Herrero-Beaumont J, Petrella RJ, Raman R, Chevalier X (2015) The discrepancy between recommendations and clinical practice for viscosupplementation in osteoarthritis: mind the gap! Eur Rev Med Pharmacol Sci 19(7):1124–1129
Migliore A, Granata M, Tormenta S, Laganà B, Piscitelli P, Bizzi E, Massafra U, Alimonti A, Maggi C, De Chiara R, Iannessi F, Sanfilippo A, Sotera R, Scapato P, Carducci S, Persod P, Denaro S, Camminiti M, Pagano MG, Bagnato G, Iolascon G (2011) Hip viscosupplementation under ultra-sound guidance riduces NSAID consumption in symptomatic hip osteoarthritis patients in a long follow-up. Data from Italian registry. Eur Rev Med Pharmacol Sci 15(1):25–34
Migliore A, Massafra U, Bizzi E, Lagana B, Germano V, Piscitelli P, Granata M, Tormenta S (2011) Intra-articular injection of hyaluronic acid (MW 1,500–2,000 kDa; HyalOne) in symptomatic osteoarthritis of the hip: a prospective cohort study. Arch Orthop Trauma Surg 131(12):1677–1685. https://doi.org/10.1007/s00402-011-1353-y (Erratum in: Arch Orthop Trauma Surg. 2012 May;132(5):735. Alberto, Migliore [corrected to Migliore, Alberto]; Umberto, Massafra [corrected to Massafra, Umberto]; Emanuele, Bizzi [corrected to Bizzi, Emanuele]; Bruno, Laganà [corrected to Lagana, Bruno]; Valentina, Germano [corrected to Germano, Valentina])
Marx RE (2004) Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg 62(4):489–496. https://doi.org/10.1016/j.joms.2003.12.003
Bennell KL, Hunter DJ, Paterson KL (2017) Platelet-rich plasma for the management of hip and knee osteoarthritis. Curr Rheumatol Rep 19(5):24. https://doi.org/10.1007/s11926-017-0652-x
Saito M, Takahashi KA, Arai Y et al (2009) Intraar¬ticular administration of platelet-rich plasma with biodegradable gelatin hydrogel micro¬spheres prevents osteoarthritis progression in the rabbit knee. Clin Exp Rheumatol 27(2):201–207
Dallari D, Stagni C, Rani N, Sabbioni G, Pelotti P, Torricelli P, Tschon M, Giavaresi G (2016) Ultrasound-guided injection of platelet-rich plasma and hyaluronic acid, separately and in combination, for hip osteoarthritis: a randomized controlled study. Am J Sports Med 44(3):664–671. https://doi.org/10.1177/0363546515620383
Battaglia M, Guaraldi F, Vannini F, Rossi G, Timoncini A, Buda R, Giannini S (2013) Efficacy of ultrasound-guided intra-articular injections of platelet-rich plasma versus hyaluronic acid for hip osteoarthritis. Orthopedics 36(12):e1501–e1508. https://doi.org/10.3928/01477447-20131120-13
Martin DR, Cox NR, Hathcock TL, Niemeyer GP, Baker HJ (2002) Isolation and characterization of multipotential mesenchymal stem cells from feline bone marrow. Exp Hematol 30(8):879–886. https://doi.org/10.1016/s0301-472x(02)00864-0
Cavallo C, Boffa A, de Girolamo L et al (2023) Bone marrow aspirate concentrate quality is affected by age and harvest site. Knee Surg Sports Traumatol Arthrosc 31:2140–2151. https://doi.org/10.1007/s00167-022-07153-6
Kangari P, Talaei-Khozani T, Razeghian-Jahromi I, Razmkhah M (2020) Mesenchymal stem cells: amazing remedies for bone and cartilage defects. Stem Cell Res Ther 11(1):492. https://doi.org/10.1186/s13287-020-02001-1
Gobbi A, Karnatzikos G, Scotti C, Mahajan V, Mazzucco L, Grigolo B (2011) One-step cartilage repair with bone marrow aspirate concentrated cells and collagen matrix in full-thickness knee cartilage lesions: results at 2‑year follow-up. Cartilage 2(3):286–299. https://doi.org/10.1177/1947603510392023
Centeno CJ, Al-Sayegh H, Bashir J, Goodyear S, Freeman MD (2015) A dose response analysis of a specific bone marrow concentrate treatment protocol for knee osteoarthritis. BMC Musculoskelet Disord 16:258. https://doi.org/10.1186/s12891-015-0714-z
Yen YM, Kocher MS (2010) Chondral lesions of the hip: microfracture and chondroplasty. Sports Med Arthrosc Rev 18(2):83–89. https://doi.org/10.1097/JSA.0b013e3181de1189
Sampson TG (2011) Arthroscopic treatment for chondral lesions of the hip. Clin Sports Med 30(2):331–348
Lin C, Deng Z, Xiong J, Lu W, Chen K, Zheng Y, Zhu W (2022) The arthroscopic application of radiofrequency in treatment of articular cartilage lesions. Front Bioeng Biotechnol 9:822286. https://doi.org/10.3389/fbioe.2021.822286
Sekiya JK, Martin RL, Lesniak BP (2009) Arthroscopic repair of delaminated acetabular articular cartilage in femoroacetabular impingement. Orthopedics. https://doi.org/10.3928/01477447-20090728-44
Tzaveas AP, Villar RN (2010) Arthroscopic repair of acetabular chondral delamination with fibrin adhesive. Hip Int 20(1):115–119. https://doi.org/10.1177/112070001002000117
Chen H, Sun J, Hoemann CD, Lascau-Coman V, Ouyang W, McKee MD, Shive MS, Buschmann MD (2009) Drilling and microfracture lead to different bone structure and necrosis during bone-marrow stimulation for cartilage repair. J Orthop Res 27(11):1432–1438. https://doi.org/10.1002/jor.20905
Haviv B, Singh PJ, Takla A, O’Donnell J (2010) Arthroscopic femoral osteochondroplasty for cam lesions with isolated acetabular chondral damage. J Bone Joint Surg Br 92(5):629–633. https://doi.org/10.1302/0301-620X.92B5.23667
Philippon MJ, Schenker ML, Briggs KK, Maxwell RB (2008) Can microfracture produce repair tissue in acetabular chondral defects? Arthroscopy 24(1):46–50. https://doi.org/10.1016/j.arthro.2007.07.027
Erggelet C, Vavken P (2016) Microfracture for the treatment of cartilage defects in the knee joint—A golden standard? J Clin Orthop Trauma 7(3):145–152. https://doi.org/10.1016/j.jcot.2016.06.015
Erggelet C, Endres M, Neumann K, Morawietz L, Ringe J, Haberstroh K, Sittinger M, Kaps C (2009) Formation of cartilage repair tissue in articular cartilage defects pretreated with microfracture and covered with cell-free polymer-based implants. J Orthop Res 27(10):1353–1360. https://doi.org/10.1002/jor.20879
Hoemann CD, Hurtig M, Rossomacha E, Sun J, Chevrier A, Shive MS, Buschmann MD (2005) Chitosan-glycerol phosphate/blood implants improve hyaline cartilage repair in ovine microfracture defects. J Bone Joint Surg Am 87(12):2671–2686. https://doi.org/10.2106/JBJS.D.02536
Jelic M, Pecina M, Haspl M, Kos J, Taylor K, Maticic D, McCartney J, Yin S, Rueger D, Vukicevic S (2001) Regeneration of articular cartilage chondral defects by osteogenic protein‑1 (bone morphogenetic protein-7) in sheep. Growth Factors 19(2):101–113. https://doi.org/10.3109/08977190109001079
Zhang X, Zheng Z, Liu P, Ma Y, Lin L, Lang N, Fu X, Zhang J, Ma K, Chen P, Zhou C, Ao Y (2008) The synergistic effects of microfracture, perforated decalcified cortical bone matrix and adenovirus-bone morphogenetic protein‑4 in cartilage defect repair. Biomaterials 29(35):4616–4629. https://doi.org/10.1016/j.biomaterials.2008.07.051
Hung GL, Galea-Lauri J, Mueller GM, Georgescu HI, Larkin LA, Suchanek MK, Tindal MH, Robbins PD, Evans CH (1994) Suppression of intra-articular responses to interleukin‑1 by transfer of the interleukin‑1 receptor antagonist gene to synovium. Gene Ther 1(1):64–69
Roessler BJ, Hartman JW, Vallance DK, Latta JM, Janich SL, Davidson BL (1995) Inhibition of interleukin-1-induced effects in synoviocytes transduced with the human IL‑1 receptor antagonist cDNA using an adenoviral vector. Hum Gene Ther 6(3):307–316. https://doi.org/10.1089/hum.1995.6.3-307
Zhu X, Du J, Liu G (2012) The comparison of multilineage differentiation of bone marrow and adipose-derived mesenchymal stem cells. Clin Lab 58(9–10):897–903
Kunze KN, Burnett RA, Wright-Chisem J, Frank RM, Chahla J (2020) Adipose-derived mesenchymal stem cell treatments and available formulations. Curr Rev Musculoskelet Med 13(3):264–280. https://doi.org/10.1007/s12178-020-09624-0
Jannelli E, Fontana A (2017) Arthroscopic treatment of chondral defects in the hip: AMIC, MACI, microfragmented adipose tissue transplantation (MATT) and other options. SICOT J. https://doi.org/10.1051/sicotj/2017029
Chahla J, Dean CS, Moatshe G, Pascual-Garrido C, Cruz SR, LaPrade RF (2016) Concentrated bone marrow aspirate for the treatment of Chondral injuries and osteoarthritis of the knee: a systematic review of outcomes. Orthop J Sports Med 4(1):2325967115625481. https://doi.org/10.1177/2325967115625481
Dall’Oca C, Breda S, Elena N, Valentini R, Samaila EM, Magnan B (2019) Mesenchymal Stem Cells injection in hip osteoarthritis: preliminary results. Acta Biomed 90(1-S):75–80. https://doi.org/10.23750/abm.v90i1-S
Ivone A, Fioruzzi A, Jannelli E, Castelli A, Ghiara M, Ferranti Calderoni E, Fontana A (2019) Micro-fragmented Adipose Tissue Transplantation (MATT) for the treatment of acetabular delamination. A two years follow up comparison study with microfractures. Acta Biomed 90(12-S):69–75. https://doi.org/10.23750/abm.v90i12-S.8950
Fortun CM, Streit J, Patel SH, Salata MJ (2012) Cartilage defects in the hip. Oper Tech Sports Med 20:287–294
Akimau P, Bhosale A, Harrison PE, Roberts S, McCall IW, Richardson JB, Ashton BA (2006) Autologous chondrocyte implantation with bone grafting for osteochondral defect due to posttraumatic osteonecrosis of the hip—a case report. Acta Orthop 77(2):333–336. https://doi.org/10.1080/17453670610046208
Fontana A, Bistolfi A, Crova M, Rosso F, Massazza G (2012) Arthroscopic treatment of hip chondral defects: autologous chondrocyte transplantation versus simple debridement—a pilot study. Arthroscopy 28(3):322–329. https://doi.org/10.1016/j.arthro.2011.08.304
Lee YH, Suzer F, Thermann H (2014) Autologous matrix-induced chondrogenesis in the knee: a review. Cartilage 5(3):145–153. https://doi.org/10.1177/1947603514529445
Thier S, Weiss C, Fickert S (2017) Arthroscopic autologous chondrocyte implantation in the hip for the treatment of full-thickness cartilage defects—A case series of 29 patients and review of the literature. SICOT J 3:72. https://doi.org/10.1051/sicotj/2017037
Krueger DR, Gesslein M, Schuetz M, Perka C, Schroeder JH (2018) Injectable autologous chondrocyte implantation (ACI) in acetabular cartilage defects-three-year results. J Hip Preserv Surg 5(4):386–392. https://doi.org/10.1093/jhps/hny043
Jiang S, Guo W, Tian G, Luo X, Peng L, Liu S, Sui X, Guo Q, Li X (2020) Clinical application status of articular cartilage regeneration techniques: tissue-engineered cartilage brings new hope. Stem Cells Int. https://doi.org/10.1155/2020/5690252
Riedl M, Vadalà G, Papalia R, Denaro V (2020) Three-dimensional, scaffold-free, autologous chondrocyte transplantation: a systematic review. Orthop J Sports Med 8(9):2325967120951152. https://doi.org/10.1177/2325967120951152
Fickert S, Schattenberg T, Niks M, Weiss C, Thier S (2014) Feasibility of arthroscopic 3‑dimensional, purely autologous chondrocyte transplantation for chondral defects of the hip: a case series. Arch Orthop Trauma Surg 134(7):971–978. https://doi.org/10.1007/s00402-014-1997-5
Schroeder JH, Hufeland M, Schütz M, Haas NP, Perka C, Krueger DR (2016) Injectable autologous chondrocyte transplantation for full thickness acetabular cartilage defects: early clinical results. Arch Orthop Trauma Surg 136(10):1445–1451. https://doi.org/10.1007/s00402-016-2510-0
Körsmeier K, Claßen T, Kamminga M, Rekowski J, Jäger M, Landgraeber S (2016) Arthroscopic three-dimensional autologous chondrocyte transplantation using spheroids for the treatment of full-thickness cartilage defects of the hip joint. Knee Surg Sports Traumatol Arthrosc 24(6):2032–2037. https://doi.org/10.1007/s00167-014-3293-x
Zimmerer A, Gebhardt S, Kinkel S, Sobau C (2023) Das Minced-Cartilage-Verfahren zur Therapie azetabulärer Knorpelschäden am Hüftgelenk [Minced cartilage procedure for the treatment of acetabular cartilage lesions of the hip joint]. Oper Orthop Traumatol 35(2):100–109. https://doi.org/10.1007/s00064-022-00796-1
Gebhardt S, Hofer A, Wassilew GI, Sobau C, Zimmerer A (2023) Minced cartilage implantation in acetabular cartilage defects: case series with 2‑year results. Cartilage 3:19476035231189840. https://doi.org/10.1177/19476035231189840
Viamont-Guerra MR, Bonin N, May O, Le Viguelloux A, Saffarini M, Laude F (2020) Promising outcomes of hip mosaicplasty by minimally invasive anterior approach using osteochondral autografts from the ipsilateral femoral head. Knee Surg Sports Traumatol Arthrosc 28(3):767–776. https://doi.org/10.1007/s00167-019-05442-1
Girard J, Roumazeille T, Sakr M, Migaud H (2011) Osteochondral mosaicplasty of the femoral head. Hip Int 21(5):542–548. https://doi.org/10.5301/HIP.2011.8659
Bakircioglu S, Atilla B (2021) Hip preserving procedures for osteonecrosis of the femoral head after collapse. J Clin Orthop Trauma 23:101636. https://doi.org/10.1016/j.jcot.2021.101636
Kocadal O, Akman B, Güven M, Şaylı U (2017) Arthroscopic-assisted retrograde mosaicplasty for an osteochondral defect of the femoral head without performing surgical hip dislocation. SICOT J 3:41. https://doi.org/10.1051/sicotj/2017030
Tripathy SK, Goyal T, Sen RK (2015) Management of femoral head osteonecrosis: current concepts. Indian J Orthop 49(1):28–45. https://doi.org/10.4103/0019-5413.143911
Athanasiou V, Argyropoulou E, Antzoulas P, Lakoumentas J, Diamantakis G, Gliatis J (2022) Mosaicplasty of the femoral head: a systematic review and meta-analysis of the current literature. Cureus 14(11):e31874. https://doi.org/10.7759/cureus.31874
Gross AE, Kim W, Las Heras F, Backstein D, Safir O, Pritzker KP (2008) Fresh osteochondral allografts for posttraumatic knee defects: long-term followup. Clin Orthop Relat Res 466(8):1863–1870. https://doi.org/10.1007/s11999-008-0282-8
Garcia-Mansilla I, Jones KJ, Sassoon AA (2020) Surgical hip dislocation and fresh osteochondral allograft transplantation for femoroacetabular impingement and concomitant chondral lesion. Arthrosc Tech 9(12):e1857–e1863. https://doi.org/10.1016/j.eats.2020.08.012
Krych AJ, Robertson CM, Williams RJ 3rd, Cartilage Study Group (2012) Return to athletic activity after osteochondral allograft transplantation in the knee. Am J Sports Med 40(5):1053–1059. https://doi.org/10.1177/0363546511435780
Frassica MT, Grunlan MA (2020) Perspectives on synthetic materials to guide tissue regeneration for osteochondral defect repair. ACS Biomater Sci Eng 6(8):4324–4336. https://doi.org/10.1021/acsbiomaterials.0c00753
Fu JN, Wang X, Yang M, Chen YR, Zhang JY, Deng RH, Zhang ZN, Yu JK, Yuan FZ (2022) Scaffold-based tissue engineering strategies for osteochondral repair. Front Bioeng Biotechnol 11(9):812383. https://doi.org/10.3389/fbioe.2021.812383
Xu D, Cheng G, Dai J, Li Z (2021) Bi-layered composite scaffold for repair of the osteochondral defects. Adv Wound Care 10(8):401–414. https://doi.org/10.1089/wound.2019.1140
El Bitar YF, Lindner D, Jackson TJ, Domb BG (2014) Joint-preserving surgical options for management of chondral injuries of the hip. J Am Acad Orthop Surg 22(1):46–56. https://doi.org/10.5435/JAAOS-22-01-46
Fickert S, Aurich M, Albrecht D, Angele P, Büchler L, Dienst M, Erggelet C, Fritz J, Gebhart C, Gollwitzer H, Kindler M, Lampert C, Madry H, Möckel G, Niemeyer P, Schröder J, Sobau C, Spahn G, Zinser W, Landgraeber S (2017) Biologische Rekonstruktion lokalisiert vollschichtiger Knorpelschäden des Hüftgelenks: Empfehlungen der Arbeitsgemeinschaft „Klinische Geweberegeneration“ der DGOU und des Hüftkomitees der AGA [Biologic Reconstruction of Full Sized Cartilage Defects of the Hip: A Guideline from the DGOU Group “Clinical Tissue Regeneration“ and the Hip Committee of the AGA]. Z Orthop Unfall 155(6):670–682. https://doi.org/10.1055/s-0043-116218
Adler KL, Cook PC, Geisler PR, Yen YM, Giordano BD (2016) Current concepts in hip preservation surgery: part II—rehabilitation. Sports Health 8(1):57–64. https://doi.org/10.1177/1941738115577621
Rolf S, Kwan CK, Stoddart M, Li Y, Fu SC (2022) Timing of postoperative weightbearing in the treatment of traumatic chondral injuries of the knee in athletes—A systematic review of current concepts in clinicalpractice. Asia Pac J Sports Med Arthrosc Rehabil Technol 27:1–8. https://doi.org/10.1016/j.asmart.2022.01.001
Jain D, Belay ES, Anderson JA, Garrett WE, Lau BC (2021) Are weightbearing restrictions required after microfracture for isolated chondral lesions of the knee? A review of the basic science and clinical literature. Sports Health 13(2):111–115. https://doi.org/10.1177/1941738120938662
de Darren SA, Thornley P, Niroopan G, Khan M, Mccarthy C, Simunovic N, Adamich J, Sahab J, Farrokhyar F, Peterson D, Musahl V, Ayeni O (2016) No difference in outcome between early versus delayed weight-bearing following microfracture surgery of the hip, knee or ankle: a systematic review of outcomes and complications. J ISAKOS. https://doi.org/10.1136/jisakos-2015-000028
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Itha, R. Vaishya, A. Vaish and F. Migliorini declared that they have no competing interests.
For this article, no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information

Scan QR code & read article online
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Itha, R., Vaishya, R., Vaish, A. et al. Management of chondral and osteochondral lesions of the hip. Orthopädie 53, 23–38 (2024). https://doi.org/10.1007/s00132-023-04444-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-023-04444-9
Keywords
- Cartilage
- Subchondral
- Impingement
- Microfracture
- Chondroplasty
- Hyaluronic Acid
- Prosthetic Biocomposites
- Autograft
- Allograft