Abstract
Objectives
To evaluate the association between adverse experiences during Hurricane María and mental and emotional distress in Puerto Rico.
Methods
This cross-sectional study used baseline data from adult (30–75 years) participants of the Puerto Rico Observational Study of Psychosocial, Environmental, and Chronic Disease Trends (PROSPECT). Enrolled individuals prior to COVID-19 who completed a 33-item questionnaire on Hurricane María-related experiences (sub-categorized as personal, service, or property losses), depression symptomatology, post-traumatic stress disorder (PTSD), and anxiety were included for analysis (n = 456).
Results
Most participants experienced fear for their family's safety, damage to their home and personal items, communication outages, and water shortages. Each additional stressor was significantly associated with higher odds of depression symptoms, PTSD, and anxiety. Personal losses were significantly associated with higher likelihood of all outcomes, while services losses were associated with depression symptoms and anxiety; property loss was not significantly associated with any outcome.
Conclusions
Adverse experiences during a major natural disaster are associated with mental and emotional distress. Strategies to minimize hardships during natural disasters, especially personal and service losses, are essential to preserve mental health. Post-disaster psychological support to individuals is crucial.
Similar content being viewed by others
Introduction
The frequency of natural disasters, including hurricanes, is on the rise worldwide [1]. Specific geographical areas are more susceptible to hurricanes than others. In particular, the island of Puerto Rico (PR), a territory of the United States, has endured 10 major hurricanes over the past century [2]. PR recently faced one of its most catastrophic hurricane seasons in 2017 with back-to-back hurricanes Irma and María. Hurricane María made landfall in PR as a category 5 storm on September 20, 2017, and lingered on the island for hours, causing severe destruction and flooding from winds, rain and storm surge. Damage to houses, infrastructure, and roads was catastrophic and widespread, causing between $106 to $133 billion in damages [3]. The whole island was left without power [4], approximately 90% of wireless telephone towers were destroyed (hindering communication) [5], and many residents faced difficulties with transportation due to debris and landslides [6]. There were also severe limitations in access to basic needs such as food, potable water, and health services [6]. A total of 2975 (95% CI 2658, 3290) excess deaths were estimated for the post-disaster period of September 2017 through February 2018 [7]. Individual assessment of adverse experiences related to Hurricane María, as well as their potential effects on mental health, has been limited.
An extensive body of literature has documented a link between exposure to natural disasters and mental health outcomes in other geographical regions [8, 9]. For example, a metanalysis of disasters (both natural and manmade) and psychological pathologies revealed a 17% increase in the rate of post-disaster psychological pathologies (including depression, anxiety, and stress) [8]. A study that evaluated the effects of Hurricane Andrew on mental health outcomes in South Florida, United States in an at-risk sample revealed that 51% met the criteria for new onset of psychological pathologies following the hurricane, including depression (30%), post-traumatic stress disorder (PTSD; 36%) and other anxiety disorders (20%) [9] Approximately 17% of residents in PR were already experiencing a mental health pathology (e.g., depression) prior to Hurricane María [10]; thus, threats from a natural disaster could further jeopardize the population's mental health.
Research on natural disasters has also demonstrated a greater risk of poor post-disaster mental health outcomes among ethnic minorities [11]. For example, African Americans were 86% more likely to have depression than non-Hispanic white individuals following Hurricane Katrina in New Orleans in 2005, possibly due to low socioeconomic status and other pre-existing vulnerabilities [11]. This evidence is particularly relevant to residents of PR, which are an ethnic minority with a high poverty rate in the United States. A few studies have documented a high prevalence of poor mental health outcomes among adults in PR post-María (e.g., 33% depression, 27% anxiety, and 44% PTSD) [12, 13], but these studies did not evaluate the specific hurricane-related exposures that may have contributed to mental health outcomes. Only one study has evaluated this association in PR among children, finding a positive association between exposure to hurricane stressors (i.e., injuries, death of family/friends, damages to house and belongings, food/water shortages, violence, and unrestored electricity) and depression and PTSD scores [14]; these relationships among adults, however, remain to be determined. Thus, given the aforementioned research gaps, the objective of the present study was to document the prevalence of Hurricane María-related adverse experiences in adults in PR and evaluate their association with mental and emotional distress outcomes (i.e., depression, PTSD, and anxiety). Findings from this study have the potential to encourage strengthened psychological support to individuals post-disaster.
Methods
Study design and participants
We analyzed data from the Puerto Rico Observational Study of Psychosocial, Environmental, and Chronic Disease Trends (PROSPECT), an ongoing longitudinal study that started in 2019 aiming to recruit 2000 adults (30–75 years) residing in PR [15]. Participants are recruited using a multistage sampling strategy that includes probabilistic sampling (through census blocks) and community-wide sampling (from partner clinics, social media, referrals, and eligible adults from a previous pilot study [16]). Interested individuals are screened for eligibility, which includes being 30–75 years, non-institutionalized, residing in PR at least in the prior year, no plans to move out of the island within 3 years, and able to answer questions (in Spanish or English) without assistance. All participants provided written informed consent prior to study participation. Trained study staff conducted standardized interviews and clinical protocols in Spanish (English was available upon request). The study was approved by the Institutional Review Boards at Harvard T.H. Chan School of Public Health, Ponce Health Sciences University in PR, and University of Massachusetts Lowell.
A total of 947 individuals were enrolled in PROSPECT at the time of analysis. Of these, only individuals enrolled before the COVID-19 pandemic were included, given its likely influence on mental and emotional distress outcomes (n = 543). We further excluded individuals who did not report having experienced Hurricane María in PR (n = 47), had unreliable interviews (n = 13), or had missing data on exposure (n = 1), outcomes (n = 6), or covariates (n = 20). Thus, a total of 456 participants were included in this analysis.
Hurricane-related exposures
Hurricane-related adverse experiences were measured with an adapted questionnaire that included two sources that measured disaster impact [17, 18]. The resulting questionnaire asked about personal impact, property damage and loss, and loss of services and resources after Hurricane María. A total of 33 experiences were included. The questionnaire was sub-categorized into three subscales. First, 12 items evaluated personal impact experiences, including fear of dying, getting injured, or for family's safety; relocating within or outside of PR; loss of job or pet; and number of days with altered eating habits. Response options to all items were "Yes" or "No," except for the number of days with altered eating habits, which was probed as a numeric value and then categorized according to the median of 30 days (coded as 0 if at or below the median and 1 if above the median). Next, a loss of property subscale, which consisted of 7 items, specifically asked about damages to the house, other items/property (e.g., vehicles), and objects of sentimental value. Lastly, the loss of service subscale consisted of 14 items that asked about the number of days without communication, power, water, access to foods, medicine, and transportation (entered as a numeric value). We used the median number of days for each of these items to categorize them (median number of days for all loss of service exposures was zero except for power (90 days), communication (20 days), water service (4 days), access to purchased foods (7 days), and pre-hurricane stored food duration (14 days)).
To calculate the hurricane exposure subscales, we added each affirmative item within the subscale. Thus, the personal impact subscale had a possible score range of 0–12, the loss of property subscale of 0–17, and the loss of service subscale of 0–14. The scores of each subscale were then summed to generate the total hurricane experiences sum score, which had a possible score range of 0–33; a higher score indicated a higher number of adverse experiences.
Mental and emotional distress outcomes
Depressive symptoms were measured with the Center for Epidemiological Studies Depression (CESD) scale [19,20,21]. This scale has been validated and previously translated into Spanish [22]. The 20-item scale asked about frequency of depressed mood, feelings of guilt and worthlessness, feelings of helplessness and hopelessness, and sleep disturbance using the previous week as the reference period. Response options were rarely/none (0), some/little (1), occasionally/moderate (2), and most/all the time (3). The total score was calculated by adding up the responses for all items; thus, the total score ranges from 0 to 60. A score of 16 or greater was used to define presence of depressive symptoms (vs. no depressive symptoms as a score less than 16) [19].
Symptoms of PTSD were assessed using the PTSD Abbreviated Civilian Version [23, 24]. The psychometric properties of the full Spanish PTSD checklist are validated as equivalent to the English version [25]. This 6-item Questionnaire asked about re-experiencing, avoidance, and hyperarousal of past traumatic events in the previous month. Response options were on a 4-point Likert scale and ranged from not at all to extremely. Items were summed to calculate the total PTSD score. We further categorized the total score using a cut-off score of 14 or greater to define presence of PTSD (vs. no PTSD as score less than 14) [23].
Symptoms of anxiety were measured with the Generalized Anxiety Disorder (GAD) screener [26, 27]. This scale has been translated and adapted into Spanish and further validated [28]. This 7-item scale asked about the frequency of anxiety symptoms over the past 2 weeks (i.e., felt nervous, unable to stop worrying, trouble relaxing, and easily irritable). Response options were: not at all (0), several days (1), more than half of the days (2), and nearly every day (3). The total score was calculated by adding up the responses for all items; thus, the total score ranged from 0 to 21. A standard cut-off score of 10 or greater was used to define presence of anxiety (vs. no anxiety as score less than 10) [26].
Participants missing 25% or more items on each of the outcome measures were not included in the analysis.
Covariates
Participants self-reported their ethnic heritage group, and responses were categorized as Puerto Rican vs. others (i.e., Dominican, mainland American, etc.). Participants self-reported urban or other (rural or suburban) residence. Formal education was categorized as less than high school, high school graduate, some college/college graduate, and graduate school. Annual household income was categorized as ≤ $10,000, $10,001–$20,000, or > $20,000. Marital status was categorized into married or living with a partner, single, or divorced/separated/widowed. Employment status was categorized as retired, employed, unemployed, or disabled. Smoking was defined as current smoker vs. not (past or never smoker). Binge drinking was defined for men as consuming 5 or more drinks and for women as consuming 4 or more drinks in a 2-h time-span. Physical activity was measured with a modified version of the Paffenbarger questionnaire of the Harvard Alumni Activity Survey [29, 30]. The calculated physical activity score was categorized as sedentary/light activity, moderate, or vigorous activity. Lastly, chronic stress was measured with a chronic stress inventory that asked about ongoing stress in eight life domains [31, 32]. A total chronic stress score was computed by adding the number of stressors experienced for a minimum of six months and rated as moderately or very stressful.
Statistical analysis
Descriptive statistics were calculated for the total analytic sample. The proportion of individuals experiencing each of the hurricane-related stressors was also calculated for the total sample. We conducted linear regression models to determine the association between the continuous hurricane experiences sum score (and each subscale score) and the continuous scores of each mental and emotional distress outcome (i.e., depression symptoms, PTSD, and GAD). We also conducted logistic regression models to evaluate the association between the continuous total hurricane experiences sum score (and each subscale) and the odds of having each outcome. We fitted two different multivariable models for each linear and logistic regression, controlling for demographic and behavioral factors (age, sex, ethnicity, marital status, income, education, rurality, employment, smoking, binge drinking, physical activity) in the first model (Model 1), and adding chronic stress in the second model (Model 2). Sensitivity analyses were conducted with each of the hurricane-related exposures subscales standardized to z-scores due to their varying number of items and scores. Analyses were conducted with STATA version 14 and SAS version 9.4 (SAS Institute Inc; Cary, NC, USA). All tests were two-tailed; significance was set at p < 0.05.
Results
The mean (SD) age of the sample was 54.0 (10.8) years; about two-thirds were female, and the majority self-identified as Puerto Rican (92.3%) and lived in urban areas (79.8%) (Table 1). Approximately half of the sample had some college education or attained a college degree, were employed, and were married or living with a partner. Almost 40% had an annual household income greater than $20,000. Thirteen percent were current smokers, 12% engaged in binge drinking, and most were sedentary or lightly active. Lastly, about a third had elevated depression symptoms (31.1%) and met the criteria for PTSD (32.0%), and one fifth met the criteria for GAD (21.5%). Spearman correlation coefficients showed that depression, PTSD, and GAD scores were significantly and positively correlated: 0.52 for depression and PTSD, 0.71 for depression and GAD, and 0.56 for PTSD and GAD (data not shown).
Of the personal impact experiences, the most prevalent were fear of dying (72.7%), fear of getting injured or in danger (46.6%), and altering eating habits for more than 30 days (41.0%) (Table 2). The most common losses of property were home damage (58.0%), damage to personal items (50.6%), and damage to other property (37.8%). Lastly, among service losses, the most prevalent were lack of water service for more than four days (50.0%), lack of communication for three weeks or more (49.8%), and lack of power for more than 90 days (46.1%).
Adjusted linear regression models for socio-demographics and behavioral factors (Model 1) showed that the total hurricane experiences sum score was positively associated with higher symptoms of depression, PTSD, and GAD (Table 3). When evaluating hurricane exposures by sub-score, the personal impact, and the loss of service sub-scores were positively associated with depression symptoms, PTSD, and GAD (Model 1). However, the personal impact sub-score had stronger associations with all three outcomes. This observation remained in sensitivity analyses using standardized z-scores for each of the subscales (Supplemental Table 1). The loss of property sub-score was not associated with any of the outcomes. Most results remained statistically significant after further adjustment for chronic stress (Model 2), albeit with attenuated coefficients. All models were evaluated by level of income (≤ $10,000 and > $10,000); results were similar but yielded slightly stronger estimates for those of lower income (data not shown).
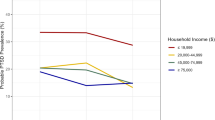
In fully adjusted models, each unit increase in the total hurricane experience sum score was associated with a 10% (95% CI 1.04, 1.16), 8% (95% CI 1.02, 1.14), and 10% (95% CI 1.04, 1.17) higher odds of depression symptoms, PTSD, and GAD, respectively (Fig. 1). Evaluation of the hurricane exposures by sub-score showed that each unit increase in the personal impact score was associated with a 29% (95% CI 1.13, 1.47), 22% (95% CI 1.09, 1.39), and 33% (95% CI 1.15, 1.54) increase in the odds of depression symptoms, PTSD, and GAD, respectively. In addition, each unit increase in the loss of service score was associated with a 14% higher odds of depression symptoms and GAD. There was no significant association between the loss of service sub-score and PTSD, or between the loss of property sub-score and any of the outcomes. Results were similar to model 1 adjusted only for socio-demographics and behavioral factors (Supplemental Table 2). Sensitivity analyses with standardized subscales also showed that the personal impact scale had the strongest ORs for all mental health outcomes (Supplemental Table 3). Evaluating the models by level of income (≤ $10,000 and > $10,000) yielded similar results but slightly stronger estimates for those of lower income (data not shown).
Odds ratio (95% confidence intervals) of mental and emotional distress outcomes by exposures to Hurricane María among adults in Puerto Rico. PTSD Post-Traumatic Stress Disorder, GAD Generalized Anxiety Disorder. Estimates are adjusted odds ratios. Model adjusted for age, sex, ethnicity, marital status, income, education, rurality, employment, smoking, drinker, physical activity, and chronic stress. All associations are statistically significant (p < 0.05). Hurricane exposure score includes personal impact, property damage and loss, and loss of services and resources after Hurricane María. Hurricane exposure sum score and sub scores used as continuous variables. Depressive symptoms measured with the Center for Epidemiological Studies Depression (CESD; cutoff score = 16) scale. Post-traumatic stress disorder measured with the PTSD Abbreviated Civilian Version (cutoff score = 14). Generalized anxiety disorder measured with the Generalized Anxiety Disorder (GAD) screener (cutoff score = 10)
Associations between each distinct hurricane experience and likelihood of depression symptoms, PTSD, or GAD are shown in Supplemental Table 4. In fully-adjusted models, the exposure most strongly and significantly associated with depression symptoms was fear of getting injured or being in danger (OR = 2.67; 95% CI 1.67, 4.26); for PTSD, the strongest exposure was being without potable water (OR = 2.33; 95% CI 1.05, 5.17); and for GAD, the strongest exposure was experiencing health problems or injuries (OR = 3.42; 95% CI 1.75, 6.67).
Discussion
In this sample of adults who experienced Hurricane María in PR, more exposures to adverse hurricane experiences were associated with higher scores and likelihood of depression symptoms, PTSD, and GAD. Our results strongly advocate for the need to minimize at- and post-disaster negative experiences and concomitantly provide prompt and high-quality mental health support during and after natural disasters. The results also call attention to a differential effect on participants based on income level with those with more limited resources experiencing a stronger effect.
The most prevalent hurricane-related experience was fear of family’s safety, followed by home damage. A previous study documented similar hurricane-related exposures in children who experienced Hurricane María in PR [14]; however, a lower proportion, compared to the adult sample evaluated in the present study, thought their own life was at risk (29.9%) and reported damage to their own homes (45.7%) and belongings (31.0%). Although these discrepancies may be attributable to potential differences in samples or the instrument used to capture hurricane-related stressors, it may be possible that adults tend to protect children from exposures during natural disasters and help them process traumatic experiences [33, 34], thus reporting higher fear of family’s safety and damages to their homes and other property. In contrast, among individuals exposed to Hurricane Katrina, the most prevalent stressors were experiencing housing adversity (71.7%) and property loss (70.2%) [35]. The high prevalence of personal stressors in our sample highlights both the severity of Hurricane María and the potential adverse psychological internalization of disaster-related fears and experiences.
Overall, results indicated that broad exposure to adverse experiences during Hurricane María was associated with higher mental and emotional distress. Other studies have shown similar findings, with exposure to a hurricane being positively associated with several mental and emotional distress outcomes (e.g., poorer self-rated mental health, depression, anxiety, and PTSD) [36,37,38,39]. For example, individuals who experienced Hurricane Harvey in the Texas Gulf Coast reported poorer self-rated mental health than the rest of the United States population [40].
Our study also showed variation across the hurricane-exposure subscales. The personal impact score was significantly associated with all three mental and emotional distress outcomes, with comparable effect estimates. However, effect estimates were generally stronger for personal experiences than for the loss of property and loss of service subscales. After full adjustment, the loss of property score was not significantly associated with any of the mental and emotional distress outcomes. In contrast, loss of service was associated with elevated depressive symptoms and GAD but not with odds of PTSD. These results suggest that the type of hurricane-related adverse experience can have a particular impact on mental and emotional distress outcomes. Among individuals who endured Hurricane Katrina, experiencing physical illness/injury and physical adversity (e.g., sleeping in a church basement, difficulty obtaining adequate food or clothing) were significantly associated with higher odds of PTSD [35]. However, the estimate of experiencing physical adversity during the storm was almost three times higher than that of experiencing physical illness/injury, providing further evidence that hurricane-related experiences of a personal displacement and loss of food and water can have a more profound impact on mental and emotional distress. Initial loss/social disruption and fear for one's life were also evaluated and positively associated with PTSD and depression in children who experienced Hurricane María in PR, with the strongest associations observed for initial loss/social disruption [14].
Our study also documented specific hurricane-related adverse exposures that were strong determinants of mental and emotional distress; specifically, lacking food for consumption, lacking potable water, experiencing health problems/injuries, fear of getting injured/in danger, fear of family’s safety, and altering eating habits. In our sample, fear of getting injured/in danger was the exposure more strongly associated with depression symptoms. Biological and psychological changes occurring during the fear response [41], especially if chronic, may affect depression symptoms, potentially explaining our findings. Furthermore, our results show that experiencing health problems/injuries was most strongly associated with GAD. Research shows that anxiety is common after injuries and new health problems [42, 43], which may be particularly exacerbated during an emergency, like a natural disaster. In addition to deeper personal experiences, research indicates that hurricanes are particularly detrimental to psychological well-being as they disrupt daily routines, such as the ones noted above [44]. In the case of PR, access to potable water was notoriously inadequate [45], which may explain its strong association with PTSD. Our study documented that adults spent a median of four days without water service, seven days unable to purchase foods, and only 14 days with lasted food stores; eating habits had to be altered for a month to accommodate these shortages. Food and water are basic human needs, and their scarcity may contribute to mental health disorders and exacerbate nutritional deficiencies and food insecurity [46].
The observed associations between hurricane exposures and mental or emotional distress were attenuated, albeit remaining statistically significant, after adjusting for chronic stress, suggesting that the detrimental influence of hurricanes on psychological well-being is independent of chronic stress. This construct captured stress from personal health problems, health problems of close friends and family, relationship stress, work stress, and financial stress experienced in the previous 6 months; thus, it may be possible that some of these stressors were concomitant consequences to exposure to Hurricane María, rather than a potential confounder or mediator. Longitudinal data may help clarify the role of chronic stress in this association, as another study conducted after the 1989 Hurricane Hugo (in North Carolina, South Carolina, and Georgia) showed that chronic stress mediated the long‐term effects of acute disaster exposures on psychological distress [47]. Additionally, given the complexity and multidimensionality of post-disaster response and recovery, future studies should implement mixed methods research to understand multilevel factors that may explain how specific hurricane-related exposures impact mental health and identify cultural and community-specific factors helping to buffer such effect. These should include factors at the societal, organizational, interpersonal, and individual levels. Such studies also need to assess biological markers in order to comprehensively understand the pathways influencing mental health disorders after natural disasters and test novel targets for effective post-disaster interventions.
Available mental health services during and after a disaster as part of a government's emergency response are essential to decrease trauma and distress and safeguard the population's mental health. In addition, strategies that help lessen personal experiences and exposures that severely disrupt basic needs and daily routines are needed. For example, rapid access to healthy foods and potable water may be achieved by having adequate emergency food reserves. Safe construction practices and preparedness need to be implemented to decrease the risk of physical danger and injuries. During emergencies, public health messages should be truthful but empathetic to help ease fears that may trigger emotional distress.
Our results need to be interpreted with several limitations in mind. Firstly, our analysis was cross-sectional; thus, we cannot determine causality. In addition, we cannot determine the potential effect of previous storms, like Hurricane Irma, or events that occurred in PR after Hurricane María but before data collection (e.g., earthquakes and political instability) on depression, PTSD, and anxiety. Furthermore, our study lacked a comparison group of people who were not exposed to Hurricane María, as this hurricane affected the entire island. Lastly, the generalizability of our study may only be limited to adults in PR, given the historical context of the island and previous natural disasters. However, this limitation is also a study strength, as PR residents remain an understudied minority population with heightened burden of stress and mental health disorders. Another study strength is the use of data from an island-wide cohort study, which ensures representation of municipalities across the territory, many of which have remained extensively understudied and underrepresented. Lastly, detailed assessment of types of hurricane-related adverse exposures, as achieved in this study, may help pinpoint specific exposures strongly associated with mental health for future intervention targets. For example, in our sample, personal loss was a stronger determinant of distress. Thus, public health policies need to ensure appropriate mental healthcare resources available for individuals facing personal losses after a natural disaster. The identification of the effect of specific hurricane-related exposures on mental health is of great public health relevance due to a rise in natural and manmade disasters.
In conclusion, having more adverse experiences during Hurricane María was associated with unfavorable mental and emotional distress outcomes in adults in PR. Strategies to minimize hardships during natural disasters, especially personal and service losses, are essential to preserving mental health; individual psychological support is crucial immediately and long after a disaster.
References
Global increases in climate-related disasters [Internet]. https://reliefweb.int/sites/reliefweb.int/files/resources/global-increase-climate-related-disasters.pdf
San Juan, Puerto Rico's history with tropical systems [Internet]. http://www.hurricanecity.com/city/sanjuan.htm
Garcia Lopez J (2018) Apuntes sobre la evaluacion de los danos causados por el huracan maria en Puerto Rico. Revista de Administración Pública 49:157–182
Una isla a oscuras (2017). El Nuevo Dia. https://huracanmaria.elnuevodia.com/2017/mapas/electricidad/
Welton M, Vélez Vega C, Murphy CB, Rosario Z, Torres H, Russell E et al (2020) Impact of Hurricanes Irma and Maria on Puerto Rico maternal and child health research programs. Matern Child Health J 24:22–29. https://doi.org/10.1007/s10995-019-02824-2
de Arzola OR (2018) Emergency preparedness and Hurricane Maria: the experience of a Regional Academic Medical Center in Southwest Puerto Rico. J Grad Med Educ 10:477–480. https://doi.org/10.4300/JGME-D-18-00547.1
Santos-Burgoa C et al (2018) Ascertainment of the Estimated Excess Mortality from Hurricane Maria in Puerto Rico [Internet]. https://nchph.org/events/ascertainment-of-the-estimated-excess-mortality-from-hurricane-mari%C2%ADa-in-puerto-rico/#:~:text=Ascertainment%20Of%20The%20Estimated%20Excess%20Mortality%20From%20Hurricane%20Maria%20In%20Puerto%20Rico,-Ascertainment%20Of%20The&text=Independent%20researchers%20from%20the%20George,six%20months%20following%20the%20storm
Rubonis AV, Bickman L (1991) Psychological impairment in the wake of disaster: the disaster–psychopathology relationship. Psychol Bull 109:384–399. https://doi.org/10.1037/0033-2909.109.3.384
David D, Mellman TA, Mendoza LM, Kulick-Bell R, Schneiderman N (1996) Psychiatric morbidity following Hurricane Andrew. J Trauma Stress 9:607–612. https://doi.org/10.1007/bf02103669
Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health (2015) BRFSS prevalence and trends data
Ali JS, Farrell AS, Alexander AC, Forde DR, Stockton M, Ward KD (2017) Race differences in depression vulnerability following Hurricane Katrina. Psychol Trauma 9:317–324. https://doi.org/10.1037/tra0000217
Scaramutti C, Salas-Wright CP, Vos SR, Schwartz SJ (2019) The mental health impact of Hurricane Maria on Puerto Ricans in Puerto Rico and Florida. Disaster Med Public Health Prep 13:24–27. https://doi.org/10.1017/dmp.2018.151
Jiménez Chávez JC, Viruet Sánchez E, Rosario Maldonado FJ, Ramos Lucca AJ, Barros Cartagena B (2020) Promoting integrated mental health care services in disaster response programs: lessons learned after the impact of Hurricane María in Puerto Rico. Disaster Med Public Health Prep 14:130–138. https://doi.org/10.1017/dmp.2019.58
Orengo-Aguayo R, Stewart RW, de Arellano MA, Suárez-Kindy JL, Young J (2019) Disaster exposure and mental health among Puerto Rican youths after Hurricane Maria. JAMA Netw Open 2:e192619–e192619. https://doi.org/10.1001/jamanetworkopen.2019.2619
Mattei J, Tucker KL, Falcón LM et al (2020) Design and implementation of PROSPECT: Puerto Rico Observational Study of Psychosocial, Environmental, and Chronic Disease Trends. Am J Epidemiol. https://doi.org/10.1093/aje/kwaa231
Mattei J, Rodrígues-Orengo J, Tmez M et al (2017) Challenges and opportunities in establishing a collaborative multisite observational study of chronic diseases and lifestyle factors among adults in Puerto Rico. BMC Public Health 17:136
Davidson TM, Price M, McCauley JL, Ruggiero KJ (2013) Disaster impact across cultural groups: comparison of Whites, African Americans, and Latinos. Am J Community Psychol 52:97–105. https://doi.org/10.1007/s10464-013-9579-1
Lowe SR, Manove EE, Rhodes JE (2013) Posttraumatic stress and posttraumatic growth among low-income mothers who survived Hurricane Katrina. J Consult Clin Psychol 81:877–889. https://doi.org/10.1037/a0033252
Sawyer-Radloff L (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
González P, Nuñez A, Brintz C et al (2017) Measurement properties of the Center for Epidemiologic Studies Depression Scale (CES-D 10): findings from HCHS/SOL. Psychol Assess 29:372–381. https://doi.org/10.1037/pas0000330
Falcón LM, Tucker KL (2000) Prevalence and correlates of depressive symptoms among Hispanic elders in Massachusetts. J Gerontol B Psychol Sci Soc Sci 55:S108-116. https://doi.org/10.1093/geronb/55.2.s108
Ruiz-Grosso P, Loret de Mola C, Vega JD et al (2012) Validation of the Spanish Center for Epidemiological Studies Depression and Zung Self-Rating Depression Scales: a comparative validation study. PLoS ONE 7:e45413. https://doi.org/10.1371/journal.pone.0045413
Lang AJ, Stein MB (2005) An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther 43:585–594. https://doi.org/10.1016/j.brat.2004.04.005
Eisenman DP, Gelberg L, Liu H, Shapiro MF (2003) Mental health and health-related quality of life among adult Latino primary care patients living in the United States with previous exposure to political violence. JAMA 290:627–634. https://doi.org/10.1001/jama.290.5.627
Miles JN, Marshall GN, Schell TL (2008) Spanish and English versions of the PTSD Checklist-Civilian version (PCL-C): testing for differential item functioning. J Trauma Stress 21:369–376. https://doi.org/10.1002/jts.20349
Spitzer R, Kroenke K, Williams J, Lowe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166:1092–1097
Löwe B, Decker O, Muller S (2008) Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care 46:266–274. https://doi.org/10.1097/MLR.0b013e318160d093
García-Campayo J, Zamorano E, Fruiz MA (2010) Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes 8:8–8. https://doi.org/10.1186/1477-7525-8-8
Paffenbarger R, Hyde RT, Wing AL et al (1993) The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med 328:538–545
Paffenbarger R, Wing A, Hyde R (1978) Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol 108:161–175
Bromberger JT, Matthews KA (1996) A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychol Aging 11:207–213. https://doi.org/10.1037//0882-7974.11.2.207
Shivpuri S, Gallo LC, Crouse JR, Allison MA (2012) The association between chronic stress type and C-reactive protein in the multi-ethnic study of atherosclerosis: does gender make a difference? J Behav Med 35:74–85. https://doi.org/10.1007/s10865-011-9345-5
Pfefferbaum R, Gurwitch R, Robertson M, Brandt E, Pfefferbaum B (2003) Terrorism, the media, and distress in youth. Prev Res 10:14–16
Prinstein MJ, La Greca AM, Vernberg EM, Silverman WK (2010) Children's coping assistance: how parents, teachers and friends help children cope with natural disasters. J Clin Child Psychol 25:463–475
Galea S, Brewin CR, Gruber M et al (2007) Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry 64:1427–1434. https://doi.org/10.1001/archpsyc.64.12.1427
Heid AR, Pruchno R, Cartwright FP, Wilson-Genderson M (2017) Exposure to Hurricane Sandy, neighborhood collective efficacy, and post-traumatic stress symptoms in older adults. Aging Ment Health 21:742–750. https://doi.org/10.1080/13607863.2016.1154016
Jaycox LH, Cohen JA, Mannarino AP et al (2010) Children’s mental health care following Hurricane Katrina: a field trial of trauma-focused psychotherapies. J Trauma Stress 23:223–231. https://doi.org/10.1002/jts.20518
Schwartz RM, Rasul R, Kerath SM et al (2018) Displacement during Hurricane Sandy: the impact on mental health. J Emerg Manag 16:17–27. https://doi.org/10.5055/jem.2018.0350
Schwartz RM, Tuminello S, Kerath SM et al (2018) Preliminary assessment of Hurricane Harvey exposures and mental health impact. Int J Environ Res Public Health 15:974. https://doi.org/10.3390/ijerph15050974
Karaye IM, Ross AD, Perez-Patron M et al (2019) Factors associated with self-reported mental health of residents exposed to Hurricane Harvey. Progress in Disaster Science 2:100016. https://doi.org/10.1016/j.pdisas.2019.100016
Schulkin J, Morgan MA, Rosen JB (2005) A neuroendocrine mechanism for sustaining fear. Trends Neurosci 28(12):629–635. https://doi.org/10.1016/j.tins.2005.09.009 (Epub 2005 Oct 7)
Wiseman T, Foster K, Curtis K (2013) Mental health following traumatic physical injury: an integrative literature review. Injury 44(11):1383–1390. https://doi.org/10.1016/j.injury.2012.02.015 (Epub 2012 Mar 10)
Lebel S, Mutsaers B, Tomei C, Leclair CS, Jones G, Petricone-Westwood D et al (2020) Health anxiety and illness-related fears across diverse chronic illnesses: a systematic review on conceptualization, measurement, prevalence, course, and correlates. PLoS ONE 15(7):e0234124. https://doi.org/10.1371/journal.pone.0234124
Espinel Z, Kossin JP, Galea S, Richardson AS, Shultz JM (2019) Forecast: increasing mental health consequences from Atlantic Hurricanes throughout the 21st century. Psychiatr Serv 70:1165–1167. https://doi.org/10.1176/appi.ps.201900273
Colón-Ramos U, Roess AA, Robien K et al (2019) Foods distributed during federal disaster relief response in Puerto Rico after Hurricane María did not fully meet federal nutrition recommendations. J Acad Nutr Diet 119:1903–1915. https://doi.org/10.1016/j.jand.2019.03.015
Golem DL, Byrd-Bredbenner C (2015) Emergency food supplies in food secure households. Prehosp Disaster Med 30:359–364. https://doi.org/10.1017/s1049023x15004884
Norris FH, Uhl GA (1993) Chronic stress as a mediator of acute stress: the case of Hurricane Hugo1. J Appl Soc Psychol 23:1263–1284. https://doi.org/10.1111/j.1559-1816.1993.tb01032.x
Acknowledgements
This work was funded by the National Heart, Lung, and Blood Institute (Grants R01-HL143792 and K01-HL120951), the National Institute on Minority Health and Health Disparities (grant R21-MD013650), and the Robert Wood Johnson Foundation (Culture of Health Leaders Award). MT received Grant support from the NIH (Grant no. T32-HL098048).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
López-Cepero, A., O’Neill, H.J., Marrero, A. et al. Association between adverse experiences during Hurricane María and mental and emotional distress among adults in Puerto Rico. Soc Psychiatry Psychiatr Epidemiol 57, 2423–2432 (2022). https://doi.org/10.1007/s00127-022-02355-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02355-2