Abstract
Purpose
To examine associations between COVID-19-related stressors and symptoms of depression and anxiety in Black cisgender sexual minority men (SMM) and transgender women during the initial peak of the COVID-19 pandemic.
Methods
Participants from the N2 Cohort Study comprised Black cisgender SMM and Black transgender women in Chicago, IL, completed a face-to-face video or phone interview between April 20 and July 31, 2020. The survey included 18 measures of individual, network, and structural COVID-19 stressors such as income loss, network COVID-19 diagnoses, and housing loss, as well as 5 outcome measures: anxiety, depression, loneliness, worry and hope.
Results
Of 226 participants, 56.6% experienced anxiety on at least 1 of the last 14 days, 48.7% experienced depression, 48.7% experienced loneliness, 42.0% experienced worry, and 51.8% did not experience hope. Completing the study during a later phase of reopening was associated with hopefulness, RR = 1.37 95% CI [1.02, 1.85]. Fifteen of the 18 multi-level COVID-19 stressors were associated with 1 or more symptoms of depression and anxiety, for example, physical stress reactions, income loss, food loss, medication loss, network COVID-19 diagnoses, partner violence, housing loss, and neighborhood pandemic concerns (aRRs = 0.61–2.78, ps < 0.05).
Conclusion
COVID-19-related stressors were associated with depression and anxiety symptoms in Black cisgender SMM and transgender women. Mitigation strategies to reduce virus transmission should be supplemented with measures to prevent depression and anxiety among marginalized populations, such as targeted economic relief and eHealth/mHealth interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since it was declared a pandemic in March 2020, COVID-19 has had an unprecedented and lasting global impact across domains of contemporary society. In addition to direct impacts of the spread of SARS-CoV-2, the virus that causes COVID-19, most countries implemented mitigation measures. These include widespread closure of schools, workplaces, and public transport; restrictions on mass gatherings, public events, and movement; and similar physical distancing interventions to slow the incidence of contagious disease, commonly referred to as “lockdowns” or “shelter-in-place” orders. Restrictions, such as these, appear to have been effective in slowing the spread of SARS-CoV-2 [1,2,3] and thus minimizing mortality and other sequelae of this unprecedented pandemic. However, such interventions are burdensome and may have contributed to a rise in anxiety, depression, post-traumatic stress disorder, and other mental health outcomes which have been documented since the onset of this global pandemic [4,5,6,7]. For example, a global meta-analysis estimated that the prevalence of depression, anxiety, and general distress in the COVID-19 pandemic was 31.4%, 31.9%, and 41.1% respectively, compared with lower estimates in previous population studies ranging from 6.2 to 14.7% [6]. These figures point to a mounting public mental health crisis requiring intervention. Identifying the causes and subpopulations most affected will be crucial to this effort.
Race, sexual orientation, and gender identity are three key sociodemographic variables in the COVID-19 public mental health crisis. To illustrate, Black people in the U.S. have experienced disproportionate COVID-19 stressors and it has been proposed that they will experience increased mental health issues as a result [8]. Research has thus far has indicated that depression and anxiety rates have increased across racial groups, and that indicators of trauma- and stressor-related disorders, coping through substance use, and serious consideration of suicide have been higher in Black populations relative to white, [9, 10], though other data have suggested slightly lower rates of depression in Black populations in the era of COVID-19 [11]. Notably, epidemiologic research typically shows major depression to be less prevalent in non-Hispanic Black (relative to non-Hispanic white) Americans despite greater exposure to stressors, a paradox yet to be satisfactorily explained [12]. Regardless, these stressors are linked to mental health outcomes in these populations [13], and research has shown that COVID-19-related stressors such as economic loss [14], negative economic expectations [14], and fear of infection [15] have been associated with mental health outcomes in Black populations in the U.S. and the United Kingdom, underlying the need to understand the role these stressors took in increasing the mental health burden on Black Americans.
With regards to sexual and gender minorities (SGM), these groups are well-established as having higher rates of a range of mental health issues than cisgender, heterosexual populations [16,17,18] likely due to increased general and SGM-specific stressors [19, 20], and these disparities have been shown to persist during the pandemic [21, 22]. Initial data indicate that increases in mental health issues might be more severe for sexual minority groups, particularly bisexual men, compared to heterosexual adults [22]. Other research has shown that many cisgender sexual minority men (SMM) in the U.S. have had negative impacts on their wellbeing during the pandemic, as well as their social interactions, finances, food, drug use, and alcohol consumption—all risk factors for mental health problems [23, 24]. Indeed, COVID-19 related stressors at multiple levels have shown associations with mental health outcomes in research, including economic loss [25], financial worries [26], fear of infection [27, 28], concerns about COVID-19 [29], and network cases of COVID-19 [29].
For those that are both Black and SGM, the COVID-19 pandemic may have had even more severe mental health impacts. In addition to the above-outlined impacts experienced by Black and SGM people, from an intersectional perspective, the experiences of those who are both Black and SGM are unique, rather than just one plus the other, and thus in need of specific study [30]. Crucially, for example, Black SGM individuals are more likely to live in poverty than either white SGM people or Black cisgender heterosexual people [31] and Black SGM people have been shown to be more vulnerable to intimate partner violence and abuse (IPVA) than white SGM people [32, 33]. As such, there may be acute impacts on the mental health of these already at-risk groups, particularly as research has shown that COVID-19 stressors at multiple levels are associated with HIV status neutral care in these populations [34]. Despite this, we are not aware of any research to date that has examined COVID-19-related stressors and symptoms of depression and anxiety in Black cisgender SMM or transgender women, let alone research which examines these across the individual, network and structural levels at which these stressors may occur.
We examined multi-level COVID-19-related correlates of depression and anxiety symptoms in a sample of Black SMM and transgender women from the Neighborhoods and Networks (N2) Cohort Study, an ongoing study including Black cisgender SMM and transgender women in Chicago, IL. Notably, Chicago was the location of the first known human-to-human transmission of SARS-CoV-2 in the U.S. [35]. We hypothesized that COVID-19 stressors would be associated with higher levels of depression and anxiety symptoms. In addition, we conducted an exploratory analysis to examine if phase of the lockdown was associated with these symptoms, hypothesizing that later phases of the lockdown would be associated worse symptoms.
Methods
Data collection
As a part of the ongoing Neighborhoods and Networks (N2) Cohort Study in Chicago [36], we conducted a “check-in” survey during the initial peak of the COVID-19 pandemic to assess their health and wellbeing. A total of N = 226 participants took part between April 20th and July 31st, 2020. To take part in the Chicago site of N2, at the original time of recruitment participants needed to be aged 16–34, have been assigned male at birth, identify as Black or African American, have had at least one sexual encounter with a cisgender man or a transgender woman in the past year, and reside in the Chicago, IL metropolitan statistical area, without plans to move out of the area during the study. To collect this sample, we contacted 405 of the 412 baseline participants in N2 Chicago. Of those who did not take part, we succeeded in contacting 52, failed in contacting 118 and only 9 refused contact.
Participant interviews were conducted via face-to-face video using Zoom or phone by highly trained interviewers at the Survey Lab at the University of Chicago. Interviews lasted 40 min on average. At the conclusion of the interview, participants were given a $35 incentive via Venmo, CashApp or PayPal and referrals to social and health services were provided (e.g., housing, food, HIV and STI testing, COVID-19 testing). The Biological Sciences Division/University of Chicago Medical Center Institutional Review Board (IRB) at the University of Chicago has reviewed and approved all protocols to be implemented at the Chicago Center for HIV Elimination. In addition, the Columbia University Mailman School of Public Health IRB has reviewed and approved all protocols for the N2 Study at all sites.
Measures
Depression and anxiety symptoms
We measured symptoms of depression and anxiety using five questions regarding how often participants experienced anxiety, depression, loneliness, worry, and hope. These were two items adapted from the General Anxiety Disorder-7 item measure (GAD-7) [37], “On how many of the past 14 days have you felt nervous, anxious or on edge?” and “On how many of the past 14 days have you not been able to stop or control worrying?”, and three adapted from the Center for Epidemiologic Studies Depression Scale (CES-D) [38], “On how many of the past 14 days have you felt depressed?”, “On how many of the past 14 days have you felt lonely?”, and “On how many of the past 14 days have you felt hopeful about the future?”.
Phase of participation
Participants were coded into two categories based on which local restrictions were in place at the time of participation. Illinois issued a state-wide “Stay at Home” order beginning March 21, 2020. This phased into a five-stage regional reopening plan entitled “Restore Illinois’. The basic details of this plan and dates during the study are outlined in Table SI. Participants were coded as taking part during a restrictive phase if they took part during Phase 1 “Rapid Spread” or Phase 2 “Flattening” (April 20th–June 2nd 2020). Participants were coded as taking part during a reopening phase if they took part during Phase 3 “Recovery” or Phase 4 “Revitalization” (June 3rd–July 31st 2020).
Individual-level stressors
We measured (1) number of days with a physical stress reaction to social distancing, loss of income or work, or concerns about infection in the past 14 days; (2) thinking one has been “infected with COVID-19”; (3) perceived chance one will get COVID-19 in the next 3 months; (4) travel-related financial burden since the “shelter in place” (SIP) order; (5) loss of a source of income due to COVID-19; (6) perceived chance of economic challenges due to COVID-19; (7) loss of health insurance due to COVID-19; (8) loss of access to enough food since the SIP order; and (9) loss of access to enough medication to last a month since the SIP order.
Network-level stressors
We measured (1) number of the last 7 days one received emotional, material, or financial support from friends or loved ones; (2) whether friends or loved ones experienced COVID-19 symptoms such as fever, coughing, upper respiratory distress, or shortness of breath; (3) personally knowing someone diagnosed with COVID-19; (4) being in close proximity with anyone diagnosed with COVID-19 in the last 2 weeks; (5) perceived likelihood of having had sex with someone that had COVID-19; and (6) five IPVA items, e.g., “Have you been verbally attacked, put down, or otherwise emotionally abused by an intimate sexual partner?”, binary-coded as experiencing one or more form of IPVA since the SIP order or not.
Structural-level stressors
We measured (1) housing instability, i.e., whether one lost a place to stay due to the COVID-19 pandemic; (2) perceived likelihood of losing a place to stay due to COVID-19 within the next 3 months; and the (3) level of concern about the COVID-19 pandemic in one’s neighborhood in the past 14 days.
Baseline sociodemographic factors and mental health
Several covariates from the pre-pandemic baseline of N2 were included based on their theoretical link to both economic and/or social stressors and symptoms of depression and anxiety. Specifically, these consisted of age (indicators: 23–24, 25–28, 29–34, reference: 16–22), gender (man vs. woman/another gender), sexual orientation (indicators: gay, bisexual, reference: straight/other), relationship status (single vs. in one or more relationships), education (high school or higher vs. no high school and nothing higher), employment (employed vs. unemployed), income (≥ $20,000 USD vs. < $20,000 USD), baseline depression, using ten items from the CES-D [38], baseline anxiety, using the General Anxiety Disorder-7 item measure (GAD-7) [37], and housing stability. Housing stability was binary coded as per previous work with this cohort [39].
Analysis plan
One item, depression, was asked using 7 days in error, rather than 14 days for the first 43 participants, and so these data were considered missing. The 14-day version had a single case with unrelated missing data and three participants had missing data for worry. Missing data for these two items were handled using single imputation with anxiety and loneliness as indicator variables due to their sufficient levels of correlation (r = 0.45–0.61), as well as phase of participation, due to its relationship with missingness. Sensitivity analyses using pairwise deletion for these missing cases were conducted to test the effect of this analytic strategy. Missing data on independent and control variables ranged from 0.0 to 3.5%. These were accounted for using indicator variables for missingness in regression analyses. Due to the lower levels of missing data for these variables, our choice of method is not expected to drastically affect the outcome of tests [40].
We tested the association between each stressor variable and each symptom of depression and anxiety using modified Poisson regressions. Modified Poisson regressions were chosen as this technique robustly estimates relative risk (RR) rather than the odds ratio. The latter is often misinterpreted, resulting in overstatement of research findings, particularly when the probability of the outcome is not rare [41]. We adjusted for phase of reopening and the following baseline variables: age, gender, sexual orientation, relationship status, education, employment, income, housing stability, depression, and anxiety. Unfortunately, as only 24 participants were women or another gender, we were unable to complete meaningful subgroup analyses.
Results
Sample
The final sample consisted of N = 226 participants. To collect this sample, we contacted 405 of the 412 N2 baseline participants in Chicago, making for a response rate of 55.8%. A significantly higher proportion of baseline participants who took part in the “check-in” survey had completed high school education or higher (89.8% vs. 81.2%), χ2(1) = 6.30, p = 012, were employed (57.5% vs. 38.2%), χ2(1) = 15.3, p < 001, and had stable housing (68.6% vs. 53.8%), χ2(1) = 11.81, p = 003, whereas a significantly lower proportion had depression, (38.1% vs. 48.9%), χ2(1) = 4.96, p = 027. Significant differences were not found for gender, sexual orientation, income, or anxiety.
In total, 77 participants (34.1%) took part during either Phase 1 or Phase 2 of Chicago’s reopening plan and 149 (65.9%) took part during either Phase 3 or Phase 4. In terms of gender/sex, 199 participants (88.1%) were cisgender men and 24 participants (10.6%) were transgender women or another gender and assigned male at birth. In terms of sexual orientation, 131 participants (58.0%) identified as gay, 62 (27.4%) as bisexual and 33 (14.7%) as either straight, something else or do not know. The sample had a mean age of 25.7 (SD = 4.0). Based on pre-pandemic baseline measures, 203 (89.8%) had completed high school or higher education, 130 (57.5%) were employed, 84 (37.2) earned $20,000 or more a year, and 155 (68.6%) were stably housed. In terms of symptoms over the past 14 days, 128 (56.6%) experienced anxiety on at least 1 day, 110 (48.7%) experienced depression on at least 1 day, 119 (48.7%) experienced loneliness on at least 1 day, 95 (42.0%) experienced worry on at least 1 day, and 109 (48.2%) did not experience hope on any days. Further details are outlined in Table 1.
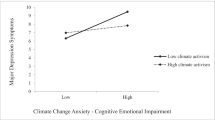
Multivariable associations between multi-level COVID-19-related stressors (phase of participation, individual, network and structural) and symptoms of depression and anxiety are shown in Table 2. We found that taking part in the survey during a reopening phase of Restore Illinois as compared to a restrictive phrase was significantly associated with higher levels hopefulness, RR = 1.37 95% CI [1.02, 1.85].
With regard to individual stressors in adjusted analyses, having had a physical stress reaction to COVID-19 related stressors (social distancing, loss of income or work, concerns about infection) on at least 1 of the last 14 days was significantly associated with anxiety, aRR = 1.89, 95% CI [1.50, 2.39], depression, aRR = 2.42, 95% CI [1.82, 3.22], loneliness, aRR = 2.29, 95% CI [1.74, 3.03], and worry, aRR = 2.69, 95% CI [1.92, 3.77]. Perceiving a ≥ 1% chance of becoming infected with COVID-19 in the next 3 months was associated with anxiety, aRR = 1.39, 95% [1.08, 1.80]. Experiencing a moderate/high/extreme travel-related financial burden due to COVID-19 was significantly associated with depression, aRR = 1.46, 95% [1.11, 1.91], loneliness aRR = 1.40, 95% [1.08, 1.84], and worry, aRR = 1.37, 95% [1.00, 1.88], though the latter was non-significant in the sensitivity analysis using pairwise deletion for cases with missing data for worry. Losing an income source was associated with loneliness aRR = 1.55, 95% [1.05, 2.30] as was perceiving there was a ≥ 1% chance of losing your job due to the pandemic, aRR = 2.78, 95% [1.20, 6.44]. Not having enough food since the order was significantly associated with depression, aRR = 1.51, 95% [1.10, 2.07], loneliness, aRR = 1.58, 95% [1.16, 2.16] and worry, aRR = 1.50, 95% [1.06, 2.14], and not having enough medication to last a month since the order was associated with higher levels of loneliness, aRR = 1.67, 95% [1.12, 2.47].
In terms of network stressors, having a friend or loved one who experienced COVID-19 symptoms was significantly associated with anxiety, aRR = 1.64, 95% [1.32, 2.04], depression, aRR = 1.49, 95% [1.14, 1.94], loneliness, aRR = 1.60, 95% [1.23, 2.09], worry, aRR = 1.67, 95% [1.23, 2.29] and personally knowing someone who was diagnosed with COVID-19 was significantly associated with anxiety, aRR = 1.41, 95% [1.10, 1.82], loneliness, aRR = 1.44, 95% [1.08, 1.93], and worry, aRR = 1.53, 95% [1.09, 2.15]. Notably, we found being in close proximity with someone who was diagnosed with COVID-19 in the last 2 weeks was only significantly associated with worry, aRR = 1.82, 95% [1.21, 2.73]. Reporting that it is somewhat/very/extremely likely that the individual had had sex with someone that had COVID-19 was significantly associated with anxiety, aRR = 1.35, 95% [1.00, 1.81], loneliness, aRR = 1.44, 95% [1.05, 1.98] and depression, aRR = 1.47, 95% [1.03, 2.10] with this latter finding being non-significant in the sensitivity analysis. Experiencing IPVA during the pandemic was significantly associated with anxiety, RR = 1.78, 95% [1.44, 2.19], depression, RR = 1.60, 95% [1.22, 2.11], loneliness, RR = 1.65, 95% [1.26, 2.17], and worry RR = 2.23, 95% [1.65, 3.02].
In terms of structural stressors, we found that losing a place to stay due to the pandemic was associated with depression, aRR = 1.43, 95% [1.03, 1.98], and worry, aRR = 1.74, 95% [1.22, 2.48], perceiving there to be a ≥ 1% chance of losing a place to stay was associated with not feeling hopeful on any of the last 14 days, RR = 0.69, 95% [0.48, 0.99]. Finally, being not very or not at all concerned about the pandemic on a neighborhood level was associated with feeling hopeful on at least 1 of the last 14 days, RR = 1.34, 95% [1.04, 1.72], not feeling lonely on any of those days aRR = 0.62, 95% [0.40, 0.94], and not feeling worried, RR = 0.61, 95% [0.38, 1.00], though this latter effect was non-significant in the sensitivity analysis. No other significant associations were found with symptoms of depression and anxiety (see Table 2).
Discussion
This study adds to our knowledge by identifying multi-level stress-related correlates with symptoms of depression and anxiety for cisgender Black SMM and transgender women in Chicago during the initial peak of the COVID-19 pandemic. To varying degrees, COVID-19 stressors were associated with these symptoms, including anxiety, depression, loneliness, worry, and hopefulness. These results corroborate research which has shown that COVID-19-related stressors such as economic loss [25], financial worries [26], fear of infection [27, 28], concerns about COVID-19 [29], and network cases of COVID-19 [29] are associated with mental health in SGMs, as well as similar research in Black populations that has found that COVID-19-related stressors such as economic loss [14], negative economic expectations [14], and fear of infection [15] as associated with mental health outcomes. By extending these findings to Black SMM and transgender women during the initial peak of the pandemic in Chicago, IL, we have provided initial evidence that the increases in these stressors during this time are risk factors for increases in negative mental health outcomes in these multiply marginalized groups.
In contrast, we did not find a significant association between loss of health insurance and symptoms of depression and anxiety. While we hypothesized a significant effect, it is notable that evidence suggests that loss of health insurance affects short-run healthcare utilization, but not necessarily mental health [42]. Such effects may only occur after living without health insurance for a period of time, though evidence for associations between health insurance coverage and mental health suggest the relationship is limited at best, though this area remains understudied [43, 44]. That said, non-significance does not in and of itself imply a null effect [45, 46], and so this finding should be interpreted as specifically as evidence against a large effect only.
Notably, three significant associations were non-significant in sensitivity analyses, specifically those between travel-related financial burden due to COVID-19 and worry, likelihood of having had sex with someone that had COVID-19 and depression, and neighborhood concerns about the pandemic and worry. This may be due to differences in biases between single imputation and pairwise deletion or the smaller sample size used in pairwise deletion. Regardless, results for these three associations should be interpreted with caution.
Importantly, though comparison with other studies is difficult due to differences in measurement of outcome variables, participants in this study appeared to have particularly high rates of depression and anxiety compared with the general U.S. population during the early days of the pandemic. For example, research using data from this time has found that 29% of adults reported some depression or anxiety symptoms [47], though other studies have found comparable numbers to those in this study such as 52.5% [48]. This is despite our attrition analyses indicating our subsample was biased towards those with lower economic precarity and depression to begin with, which suggests that the true rates in Black SGMs may be much worse than those in this study. Thus, there may be worsened mental health disparities between Black SGMs and the general population because of these increased stressors. These should be investigated in future studies.
Nevertheless, the results of this study have important implications. First, these results add to the evidence that the continuation of racism, homophobia, transphobia, and their intersections represent ongoing public health issues [30, 49, 50]. In addition to the known public health impacts of these structural inequalities, COVID-19 has revealed an underlying potential for exacerbation of these health impacts under emergency conditions such as these. Ending and preventing these health disparities depends on ending these systematic social ills. More immediately, these findings underscore the need to address the potential mental health impacts of COVID-19-related stressors, including SIP orders, on these marginalized groups. The COVID-19 pandemic is far from over and, at the time of writing, there are still racial disparities in COVID-19 vaccination rates in the U.S. [51]. In addition, novel infectious diseases in humans have increased in recent decades and epidemics are expected to increase in frequency in the future [52], which may require future stay-at-home orders. Strategies could include population-wide methods to reduce negative mental health outcomes during early mitigation measures and targeted interventions designed to address the specific stressors faced by these groups, such as providing reliable and accessible sources of information relating to COVID-19 and encouraging safe, daily physical activity, which data have suggested were beneficial for mental health during this pandemic [53]. Policymakers could also consider targeted economic relief, food packages, funding services for victims of IPVA and providing additional social housing in neighborhoods where Black SGMs live, and redoubling their work to prevent COVID-19 infection in these groups through building vaccine confidence and increasing ease of geographical access to vaccines. Access to therapy such as Cognitive Behavior Therapy and Acceptance and Commitment Therapy with clinicians trained in intersectional cultural humility could also be considered [54], but should not be seen as a replacement for directly targeting the stressors identified in this study, or indeed root causes, specifically racism, homophobia, transphobia, and their intersections.
Limitations
The results of this study should be contextualized by the limitations of the data. First, the outcome measures of depression and anxiety symptoms were not full standardized scales. Therefore, there were not specific cutoff points to use for potential diagnoses. However, as the items were derived from validated screening measures of depression and anxiety, they are indicators for these mental health outcomes. An additional issue of measurement is that all exposure and outcome data were self-reported. As such, they may be subject to social desirability and same-source bias. For example, the mental health of an individual may have influenced their perceptions of the stressors they experienced. Furthermore, due to the non-probability sampling methods, the specific focus on Chicago, and the low response rate, these results may have limited generalizability. It is unclear the extent to which these results would generalize to the larger Black cisgender SMM or Black transgender populations during this or future pandemics. However, the use of snowball sampling for the original N2 sample helped it reach participants who would not have been be found using typical methods associated with sexual minority health research [55]. In addition, research suggests that stay-at-home orders have been effective in slowing the spread of SARS-CoV-2, as well as, inadvertently, influenza [1, 56]. Given this, such measures are likely to be considered for future pandemics, and so these results should be considered as part of a broader discussion when deciding on such interventions during this and potential future pandemics.
Conclusion
A variety of COVID-19 stressors during early COVID-19 mitigation efforts in Chicago were associated with mental health outcomes in Black cisgender SMM and Black transgender women. It is possible that some of these associations may have resulted from the mitigation measures themselves. Moving forward, mitigation measures to control the spread of disease should be supplemented with measures specifically designed to prevent disproportionate mental health impact of lockdowns on marginalized populations and maintain overall wellbeing. Future research should examine the long-term impacts of the pandemic and resulting policies on the mental health of marginalized groups, as well as the impact of future pandemics and policies using psychiatric interviews. Such research should examine Black SGM subgroups, including Black bisexual people and Black transgender people.
Availability of data and materials
Data will be available upon reasonable request.
Code availability
Stata commands will be available upon reasonable request.
References
Islam N, Sharp SJ, Chowell G, Shabnam S, Kawachi I, Lacey B, Massaro JM, D’Agostino RB, White M (2020) Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. https://doi.org/10.1136/bmj.m2743
Brauner JM, Mindermann S, Sharma M, Johnston D, Salvatier J, Gavenčiak T, Stephenson AB, Leech G, Altman G, Mikulik V (2021) Inferring the effectiveness of government interventions against COVID-19. Science 371 (6531). https://doi.org/10.1126/science.abd9338
Li Y, Campbell H, Kulkarni D, Harpur A, Nundy M, Wang X, Nair H, for COVID UN, (2021) The temporal association of introducing and lifting non-pharmaceutical interventions with the time-varying reproduction number (R) of SARS-CoV-2: a modelling study across 131 countries. Lancet Infect Dis 21(2):193–202. https://doi.org/10.1016/S1473-3099(20)30785-4
Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS (2020) Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord 277:55–64. https://doi.org/10.1016/j.jad.2020.08.001
Chiesa V, Antony G, Wismar M, Rechel B (2021) COVID-19 pandemic: health impact of staying at home, social distancing and ‘lockdown’measures—a systematic review of systematic reviews. J Public Health (Oxford, England). https://doi.org/10.1093/pubmed/fdab102
Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, Wang X (2021) Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord 281:91–98. https://doi.org/10.1016/j.jad.2020.11.117
Jones EA, Mitra AK, Bhuiyan AR (2021) Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health 18(5):2470. https://doi.org/10.3390/ijerph18052470
Novacek DM, Hampton-Anderson JN, Ebor MT, Loeb TB, Wyatt GE (2020) Mental health ramifications of the COVID-19 pandemic for Black Americans: Clinical and research recommendations. Psychol Trauma Theory Res Pract Policy. https://doi.org/10.1037/tra0000796
Czeisler M, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA, Howard ME, Rajaratnam SMW (2020) Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 69 (32):1049–1057. https://doi.org/10.15585/mmwr.mm6932a1
Vahratian A, Blumberg SJ, Terlizzi EP, Schiller JS (2021) Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic—United States, August 2020–February 2021. Morbid Mortal Week Rep 70 (13):490. https://doi.org/10.15585/mmwr.mm7013e2
Saltzman LY, Lesen AE, Henry V, Hansel TC, Bordnick PS (2021) COVID-19 mental health disparities. Health security
Pamplin JR, Bates LM (2021) Evaluating hypothesized explanations for the Black-white depression paradox: a critical review of the extant evidence. Soc Sci Med 281:114085. https://doi.org/10.1016/j.socscimed.2021.114085
Pieterse AL, Todd NR, Neville HA, Carter RT (2012) Perceived racism and mental health among Black American adults: a meta-analytic review. J Couns Psychol 59(1):1–9. https://doi.org/10.1037/a0026208
Bui CN, Peng C, Mutchler JE, Burr JA (2020) Race and ethnic group disparities in emotional distress among older adults during the COVID-19 pandemic. Gerontologist 61(2):262–272. https://doi.org/10.1093/geront/gnaa217
Jaspal R, Lopes B (2021) Discrimination and mental health outcomes in British Black and South Asian people during the COVID-19 outbreak in the UK. Ment Health Relig Cult 24(1):80–96. https://doi.org/10.1080/13674676.2020.1871328
Dhejne C, Van Vlerken R, Heylens G, Arcelus J (2016) Mental health and gender dysphoria: a review of the literature. Int Rev Psychiatry 28(1):44–57. https://doi.org/10.3109/09540261.2015.1115753
Plöderl M, Tremblay P (2015) Mental health of sexual minorities: a systematic review. Int Rev Psychiatry 27(5):367–385. https://doi.org/10.3109/09540261.2015.1083949
King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, Nazareth I (2008) A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry 8(1):70. https://doi.org/10.1186/1471-244X-8-70
Meyer IH (2003) Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 129(5):674–697. https://doi.org/10.1037/0033-2909.129.5.674
Timmins L, Rimes KA, Rahman Q (2017) Minority stressors and psychological distress in transgender individuals. Psychol Sex Orientat Gend Divers 4(3):328–340. https://doi.org/10.1037/sgd0000237
Moore SE, Wierenga KL, Prince DM, Gillani B, Mintz LJ (2021) Disproportionate impact of the COVID-19 pandemic on perceived social support, mental health and somatic symptoms in sexual and gender minority populations. J Homosex. https://doi.org/10.1080/00918369.2020.1868184
Fish JN, Salerno J, Williams ND, Rinderknecht RG, Drotning KJ, Sayer L, Doan L (2021) Sexual minority disparities in health and well-being as a consequence of the COVID-19 pandemic differ by sexual identity. LGBT Health. https://doi.org/10.1089/lgbt.2020.0489
Sanchez TH, Zlotorzynska M, Rai M (2020) Characterizing the impact of COVID-19 on men who have sex with men across the United States in April. AIDS Behav 24(7):2024–2032. https://doi.org/10.1007/s10461-020-02894-2
Santos G-M, Ackerman B, Rao A, Wallach S, Ayala G, Lamontage E, Garner A, Holloway IW, Arreola S, Silenzio V (2021) Economic, mental health, HIV prevention and HIV treatment impacts of COVID-19 and the COVID-19 response on a global sample of cisgender gay men and other men who have sex with men. AIDS Behav 25 (2):311–321. https://doi.org/10.1007/s10461-020-02969-0
Restar AJ, Jin H, Jarrett B, Adamson T, Baral SD, Howell S, Beckham SW (2021) Characterising the impact of COVID-19 environment on mental health, gender affirming services and socioeconomic loss in a global sample of transgender and non-binary people: a structural equation modelling. BMJ Glob Health 6(3):e004424. https://doi.org/10.1136/bmjgh-2020-004424
Suen YT, Chan RC, Wong EMY (2020) Effects of general and sexual minority-specific COVID-19-related stressors on the mental health of lesbian, gay, and bisexual people in Hong Kong. Psychiatry Res 292:113365. https://doi.org/10.1016/j.psychres.2020.113365
Gato J, Barrientos J, Tasker F, Miscioscia M, Cerqueira-Santos E, Malmquist A, Seabra D, Leal D, Houghton M, Poli M, Gubello A, Ramos MdM, Guzmán M, Urzúa A, Ulloa F, Wurm M (2021) Psychosocial effects of the COVID-19 pandemic and mental health among LGBTQ+ young adults: A cross-cultural comparison across six nations. J Homosex 68(4):612–630. https://doi.org/10.1080/00918369.2020.1868186
Gava G, Fisher AD, Alvisi S, Mancini I, Franceschelli A, Seracchioli R, Meriggiola MC (2021) Mental health and endocrine telemedicine consultations in transgender subjects during the COVID-19 outbreak in Italy: a cross-sectional web-based survey. J Sex Med 18(5):900–907. https://doi.org/10.1016/j.jsxm.2021.03.009
Gonzales G, de Mola EL, Gavulic KA, McKay T, Purcell C (2020) Mental health needs among lesbian, gay, bisexual, and transgender college students during the COVID-19 pandemic. J Adolesc Health 67(5):645–648. https://doi.org/10.1016/j.jadohealth.2020.08.006
Bowleg L (2012) The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health 102(7):1267–1273. https://doi.org/10.2105/AJPH.2012.300750
Badgett M, Choi SK, Wilson BD (2019) LGBT poverty in the United States: A study of differences between sexual orientation and gender identity groups
Reuter TR, Newcomb ME, Whitton SW, Mustanski B (2017) Intimate partner violence victimization in LGBT young adults: demographic differences and associations with health behaviors. Psychol Violence 7(1):101. https://doi.org/10.1037/vio0000031
Whitton SW, Newcomb ME, Messinger AM, Byck G, Mustanski B (2019) A longitudinal study of IPV victimization among sexual minority youth. J Interpers Violence 34(5):912–945. https://doi.org/10.1177/0886260516646093
Chen Y-T, Duncan DT, Del Vecchio N, Timmins L, Pagkas-Bather J, Lacap S, Hotton A, Knox J, Hanson H, Koli K, Durrell M, Dehlin J, Schneider JA (2021) COVID-19 related stressors, sex behaviors, and HIV status neutral care among Black men who have sex with men and transgender women in Chicago, USA. J Acquir Immune Defic Syndr Advance Online Publication. https://doi.org/10.1097/qai.0000000000002770
Ghinai I, McPherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K, Rubin R, Morales-Estrada S, Black SR, Pacilli M (2020) First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. The Lancet. https://doi.org/10.1186/s13063-020-04446-4
Duncan DT, Hickson DA, Goedel WC, Callander D, Brooks B, Chen Y-T, Hanson H, Eavou R, Khanna AS, Chaix B (2019) The social context of HIV prevention and care among black men who have sex with men in three US cities: The neighborhoods and networks (N2) cohort study. Int J Environ Health Res 16 (11):1922
Spitzer RL, Kroenke K, Williams JB, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 166(10):1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Radloff LS (1977) The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas 1(3):385–401. https://doi.org/10.1177/014662167700100306
Chen Y-T, Duncan DT, Issema R, Goedel WC, Callander D, Bernard-Herman B, Hanson H, Eavou R, Schneider JA, Hotton A (2020) Social-environmental resilience, PrEP uptake, and viral suppression among young black men who have sex with men and young black transgender women: the neighborhoods and networks (N2) study in Chicago. J Urban Health 97(5):728–738. https://doi.org/10.1007/s11524-020-00425-x
Tabachnick BG, Fidell LS (2013) Using multivariate statistics, 6th edn. Pearson, New York
Zou G (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159(7):702–706. https://doi.org/10.1093/aje/kwh090
Schaller J, Stevens AH (2015) Short-run effects of job loss on health conditions, health insurance, and health care utilization. J Health Econ 43:190–203. https://doi.org/10.1016/j.jhealeco.2015.07.003
Jacobs AW, Hill TD, Burdette AM (2015) Health insurance status and symptoms of psychological distress among low-income urban women. Soc Ment Health 5(1):1–15. https://doi.org/10.1177/2156869314549674
Michael McWilliams J (2009) Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q 87(2):443–494. https://doi.org/10.1111/j.1468-0009.2009.00564.x
Greenland S (2012) Nonsignificance plus high power does not imply support for the null over the alternative. Ann Epidemiol 22(5):364–368. https://doi.org/10.1016/j.annepidem.2012.02.007
Amrhein V, Greenland S, McShane B (2019) Scientists rise up against statistical significance. Nat Publ Group. https://doi.org/10.1038/d41586-019-00857-9
Kämpfen F, Kohler IV, Ciancio A, Bruine de Bruin W, Maurer J, Kohler H-P (2020) Predictors of mental health during the Covid-19 pandemic in the US: role of economic concerns, health worries and social distancing. PLoS One 15(11):e0241895
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S (2020) Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 3(9):e2019686–e2019686
Wright JL, Jarvis JN, Pachter LM, Walker-Harding LR (2020) “Racism as a public health issue” APS racism series: at the intersection of equity, science, and social justice. Pediatr Res 88(5):696–698
Bowleg L (2020) We’re not all in this together: On COVID-19, intersectionality, and structural inequality. vol 110. American Public Health Association
Centers for Disease Control (2021) Demographic Characteristics of People Receiving COVID-19 Vaccinations in the United States. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic
Priyadarsini SL, Suresh M, Huisingh D (2020) What can we learn from previous pandemics to reduce the frequency of emerging infectious diseases like COVID-19? Global Transit 2:202–220. https://doi.org/10.1016/j.glt.2020.09.003
Safieh J, Broughan J, McCombe G, McCarthy N, Frawley T, Guerandel A, Lambert JS, Cullen W (2021) interventions to optimise mental health outcomes during the COVID-19 pandemic: a scoping review. Int J Ment Heal Addict. https://doi.org/10.1007/s11469-021-00558-3
Freeman-Coppadge DJ, Langroudi KF (2021) Beyond LGBTQ-affirmative therapy: fostering growth and healing through intersectionality. In: Queer Psychology. Springer, pp 159–179
Meyer IH, Wilson PA (2009) Sampling lesbian, gay, and bisexual populations. J Couns Psychol 56 (1):23–31. https://doi.org/10.1037/a0014587
Wiese AD, Everson J, Grijalva CG (2020) Social distancing measures: evidence of interruption of seasonal influenza activity and early lessons of the SARS-CoV-2 pandemic. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa834
Acknowledgements
We thank the participants for engaging in this research.
Funding
The Neighborhoods and Networks (N2) Cohort Study is funded through a grant from the National Institute on Mental Health (Grant Number: R01MH112406; Principal Investigators: Dustin T. Duncan, ScD and John A. Schneider, MD, MPH), a cooperative agreement with the Centers for Disease Control and Prevention under the Minority HIV/AIDS Research Initiative (Grant Number: U01PS005122; Principal Investigator: Dustin T. Duncan, ScD), and two grants from the National Institute on Drug Abuse (Grant Number: 1R03DA053161; Principal Investigators: Yen-Tyng Chen, PhD, and John A. Schneider, MD, MPH; Grant Number: R01DA054553; Principal Investigators: Justin Knox and Dustin T. Duncan, ScD). Dr. Dustin Duncan was funded in part by National Institutes of Health grants R01MH112406 and R01MD013554 and the Centers for Disease Control and Prevention grant U01PS005202. We thank the participants for engaging in this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Approval was obtained from the ethics committees of Columbia University IRB. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Timmins, L., Schneider, J.A., Chen, YT. et al. COVID-19 stressors and symptoms of depression and anxiety among Black cisgender sexual minority men and Black transgender women during the initial peak of the COVID-19 pandemic. Soc Psychiatry Psychiatr Epidemiol 57, 1999–2011 (2022). https://doi.org/10.1007/s00127-022-02282-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02282-2