Abstract
Background
Social connections have been linked to the genesis and amelioration of mental health problems and thus have potential therapeutic value.
Purpose
To identify the current evidence base, assess risk of bias and synthesise findings on the effectiveness of social network interventions for people with mental health problems.
Methods
Electronic databases (MEDLINE, Embase, PsycINFO, CINAHL, Cochrane Library, Web of Science, Scopus) and grey literature databases were systematically searched from inception to October 2021 using free text syntax combining synonyms for ‘mental health problems’ and ‘social network interventions’. Articles were eligible for inclusion if they reported data from randomised controlled trials on the effectiveness of interventions designed to improve social networks for adults (18+) with mental health problems. Papers were independently reviewed for inclusion with conflicts resolved through consensus. Included papers were quality assessed and data extracted and synthesized narratively. Risk of bias was assessed using the Cochrane Risk of Bias Tool.
Results
Nine studies randomising 2226 participants were included. Four focused on those with a diagnosis of schizophrenia or psychosis, one on major depressive disorder and four included all types of mental health diagnoses. The current evidence base is of unclear quality. However, interventions which focused on supporting social activities appear to hold the most promise for enhancing social networks. Data on cost-effectiveness and research acceptability were limited, but suggest the potential economic feasibility of and acceptability for evaluating these interventions.
Conclusion
There is emerging evidence that social network interventions can be effective in improving social connections for people with mental health problems. However, further evaluations with robust methodological approaches are required to inform evidence-based recommendations for health services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental health problems commonly occur with estimated lifetime prevalence rates of between 18 and 36% [1]. There are more disability-adjusted life years lost per year to mental health problems than any other health condition in the UK and costs to the individual, society and the economy are considerable [2]. Adults with severe mental health problems,Footnote 1 such as schizophrenia and bipolar disorder, experience higher rates of multiple and more complex physical co-morbidities resulting in significantly reduced life expectancy of approximately 15–20 years [3, 4]. It is therefore imperative that health services are able to effectively and appropriately offer a range of support to people with mental health problems.
Social networks refer to the structure and function of a person’s social relationships and the nature of the ties that connect them [5]. A person’s social network constitutes the set of connections which have the capacity to link people to relationships and resources, and can aid, restrict and reshape the way in which mental health problems are managed [6]. These connections can take a variety of configurations covering the broad range of people, non-human agents, places, things and activities which may be involved in the everyday management of mental health problems [6, 7]. Increased connectivity is linked to the provision of social support, interpersonal contact and the mobilisation of resources [8] which acts to buffer stress through the provision of functional support as well as enhancing individual coping strategies [9]. However, this differs across groups and contexts [10, 11]. For example, high contact with social networks can increase levels of depressive symptoms for women if they are accompanied by a burden of obligation to provide large amounts of social support to others [9].
The Network Episode Model (NEM) provides a theoretical basis for understanding the contributions social networks make to the daily management of mental health problems [12, 13]. The NEM rejects individualistic approaches to mental health self-management and conceptualizes self-management instead as a collective activity that people do in conjunction with their social network [12, 13]. In line with other social network approaches, the NEM provides an analytic focus on the activation of social network ties in response to mental health problems and captures the dynamic social processes through which an individual manages their mental health problems with formal (mental health professionals) and informal (friends and family) networks [12, 14].
An individual’s ability to obtain support from their social networks and negotiate its acceptability to themselves and other members of their network is impacted by existing cultures and available network and individual resources [13, 15]. Social networks can provide a range of supports to an individual with a health condition, but such support is contingent on the availability of requisite knowledge, understanding and willingness to provide help within networks which is not always present or available to individuals [16]. Whilst cross-cultural social network studies are limited in number, research has demonstrated that network homogeneity and generalized trust within networks vary across cultures [17, 18]. Furthermore, research has demonstrated that propensity to seek help from others amongst older adults was dependent on informal logical and cultural rules which affected their decisions to help-seek, where to go to obtain support, whether it was available and adequate and interpretations of others willingness to provide help [19].
Diverse and supportive social networks have been found to have a positive influence on recovery for people with a diagnosis of severe mental illness [20]. However, people with mental health problems also tend to have smaller networks of poorer quality and configuration [21]. There is evidence too of variability in the availability of network resources over time, illness phases, illness severity and setting [22]. A mental health diagnosis has been shown to lead to an erosion of existing high-quality network connections in terms of size, diversity and access to resources [14]. However, network disruption can result in network reconfiguration with new network members replacing weak, lost or absent ties which may be more protective against psychological distress and of greater utility in managing a long-term condition [23]. The latter points to markers for the development and implementation of interventions aimed to improve mechanisms for mental health management and recovery.
Improving network-based strategies for managing everyday mental health and promoting social integration are necessary for accessing community-based support and promoting and engagement in meaningful activity [24]. In turn, social activity can lead to increased social network size and access to social capitalFootnote 2 [25] creating a virtuous circle [6]. Social networks can also mediate the effects of social isolation and loneliness, and enhance self-management [20, 26]. Thus, social network interventions which assist with eliciting preferences for connecting to meaningful, valued activities in domestic and local environments extends the availability of heterogenous support for the secondary prevention of mental health problems. [7, 27]. Whilst such interventions are successful for long-term physical health conditions (e.g., social prescribing), they have been slow to translate into mainstream mental healthcare despite the relevance of community engagement and integration for recovery [7].
This review aimed to provide a critical overview of the evidence base underpinning interventions designed to improve the quantity and quality of social networks of people with mental health problems. The acceptability, feasibility and cost-effectiveness of evaluating these social network interventions were explored by examining available data on evaluation adherence, attrition and cost evaluations within included trials.
Review questions
What is the effectiveness of interventions designed to improve the quantity and quality of social networks of adults with mental health problems?
What are the factors that influence the effectiveness of social network interventions for people with mental health problems?
Methods
The methods and reporting of this systematic review and narrative synthesis follow PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidance [28]. The protocol for the review is available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020206490.
Eligibility criteria
Only published research articles containing primary data were included in the review. Literature or systematic reviews on related topics were excluded, but reference lists examined for potentially relevant studies. Studies which recruited adult participants (aged 18+) with any form of self-report or professionally diagnosed mental health difficulty (excluding organic mental health difficulties such as dementia, learning disability and co-morbidities such as substance abuse) were considered, with no restrictions placed on the diagnosis, severity or length and stage of illness. In mixed samples, mean age requirement was a minimum of 18 years and 75% of identified samples required a primary diagnosis of mental health difficulties or self-reported emotional distress.
Eligible studies had to report on an intervention designed specifically to increase the quantity or quality of social networks. In the context of this review, social networks were defined as personal communities—the constellation of relevant relationships, activities and resources that are identified as important by an individual [29]. Eligible studies also had to include a measure of social network quantity or quality as either a primary or secondary outcome and utilise a randomised design with a comparison group. There were no restrictions placed on eligible studies based on language or date of publication. Non-English language articles were screened for eligibility by native speakers affiliated with the research team. See Table 1 for inclusion and exclusion criteria.
Search strategy
Seven electronic databases were searched (MEDLINE, Embase, PsycINFO, CINAHL, Cochrane Library, Web of Science, Scopus) were searched on the 29th of August 2020 from the earliest record and updated on the 5th October 2021. The search strategy was organised using the first two components of the PICO framework and was purposively broad to optimise retrieval (see “Appendix 1” for example search):
-
Population: People with a diagnosis of mental illness or self-reported emotional distress
-
Intervention: Social network
The search strategy was informed by published reviews, extant literature on social network interventions and following discussions with the wider authorship team. A draft version of the strategy was also subject to a PRESS review by an expert librarian [30].
To minimise the impact of publication bias, grey literature sites were searched including OpenGrey and EThoS. We contacted authors of identified conference abstracts for full manuscripts where these were not readily available through web search strategies. Reference lists of included manuscripts were also scrutinized for relevant studies. Additionally, we examined identified book chapters and literature reviews for relevant literature. Key journals were hand searched: Social Psychiatry and Psychiatric Epidemiology, BMC health services research, Journal of Mental Health, British Journal of Psychiatry and Lancet Psychiatry.
Data selection and extraction
Search results were uploaded to the data management software Covidence (http://www.covidence.org) and duplicates removed. Titles and abstracts were double screened with conflicts resolved by a third reviewer. Eligibility assessments of full texts of potentially eligible manuscripts were undertaken by two reviewers with conflicts resolved by consensus. A systematic data extraction tool was developed using Excel into which quantitative data relating to the outcomes of interventions were extracted, along with data relating to study design, participants, adherence/attrition, cost-effectiveness and other relevant contextual factors. 30% of extractions and quality appraisals were checked for accuracy.
Analysis
A meta-analysis of included studies including pooling the data and comparing mean differences of related outcomes (e.g., network size) was originally planned, but given the heterogeneity of included studies, this was not possible and a narrative synthesis was undertaken. This followed the stages outlined in the Guidance on the Conduct of Narrative Synthesis in Systematic Reviews [31].
An initial synthesis was undertaken by producing textual summaries of study characteristics (e.g., design, participants, intervention, and recruitment) in data extraction spreadsheets. Included studies were organised alphabetically in excel sheets, but allocated a colour code by type of intervention. We used ‘vote counting’ to describe the number of studies which demonstrated positive, negative or neutral results relating to social network outcomes [31]. The next stage of the narrative synthesis involved a consideration of the factors that influenced successful outcomes and any other included outcome measures. Prior to finalising the synthesis, all included studies were revisited along with the PRISMA checklist (“Appendix 2”) to ensure that relevant data were not omitted from the presentation of results.
Results
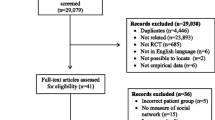
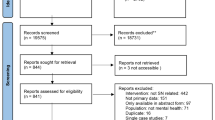
The results of the search, screening and selection for final included studies can be found in Fig. 1. Searches generated 22,367 hits of which 2792 duplicates were removed. The majority of the remaining 19,575 were excluded at title and abstract screening. Of the 841 full texts screened for eligibility, 9 were included in the systematic review. The main reasons for exclusion were interventions not being designed with an explicit focus to improve social networks, non-mental health populations and non-RCT designs (Fig. 1).
Description of included studies
The studies reported were heterogenous in terms of intervention format and delivery, outcome measures and length of follow-up. Descriptions of included studies can be found in Supplementary File 1.
Study characteristics
Three studies were carried out in the USA [32,33,34], two in the UK [35, 36] and one each in Denmark [37], Italy [38], Ireland [39], and the Netherlands [40]. All studies reported on the results of interventions for formal mental health diagnoses and no studies included those with self-reported emotional distress. Four studies included only those with a diagnosis of schizophrenia or psychosis [35, 37, 38, 40] with one recruiting only those with first episode psychosis [37]. One study exclusively comprised people with major depressive disorder [33], and the remaining studies included people with broader diagnostic categories of mental illness described as enduring mental health problems [39], AXIS I and II disorders (using DSM-III-R), [34], AXIS I Psychotic or mood disorders (DSM version not reported) [32] or included all forms of mental health conditions [36]. Most studies utilised broad conceptualisations of social networks incorporating both quantity and quality of social network support [32,33,34,35,36, 38,39,40]. Only one used social network size as the sole proxy for social network contributions with the authors acknowledging this as a limitation [37].
Participant characteristics
Included studies randomised a total of 2,226 participants across intervention and control conditions. The average age of included participants was 35.7 years. On average, 49.4% of participants were female. Only 5 reported ethnicity data with White participants accounting for 47% of participants across these included studies. Black participants accounted for 34.4%, Hispanic participants for 6.2%, Asian participants for 1% and other ethnicity groups accounting for 11.4%.
Intervention characteristics
Included studies recruited from formal health services (community and inpatient settings) and all interventions were delivered in the community. Five were delivered/facilitated by health professionals [33,34,35, 37, 40], three by lay volunteers including peers or family members [32, 36, 38] and one by a combination of professional and lay facilitators [38]. Allocated control conditions were mostly treatment as usual [32,33,34,35, 37, 38] or wait list control [40]. Active comparators included financial stipend [39] and personal recovery workbook [36].
Intervention duration ranged from 3 to 12 months with follow-up data collection periods ranging from 3 to 24 months. All interventions were delivered face-to-face. Interventions mostly comprised supported social activity/community; one explicitly aimed to develop a friendship between participant and facilitator [39]; and one included financially supported socialisation [39]. One intervention was a closed peer support group with a primary aim of improving participants’ social networks [40]. Two interventions involved one-to-one work with participants using either cognitive behavioural therapy [33] or recovery-focused activities aiming to enhance social networks [36]. Three interventions were assertive community treatment interventions with a social network focus which included family members and friends in the treatment process [34, 35, 37].
Risk of bias
Details of the risk-of-bias assessments drawing on the Cochrane Risk of Bias Tool [41] are presented in Supplementary File 1 which incorporated six domains where bias could be introduced into trial design. No studies were assessed as being “low risk of bias”. Five studies were assessed as being high risk and the other four did not provide sufficient information for risk-of-bias assessments to be undertaken. Therefore, the proportion of information from studies at high risk of bias is considered sufficient to affect the interpretation of results [41].
Clinical effectiveness
Summary information on clinical effectiveness, effect size and study quality can be found in Tables 2, 3, 4. Interventions were categorised into four types based on core activities: supported social activity, peer support, assertive community treatment and one-to-one interventions.
Social network quality and quantity
Structured support for undertaking social activity
All three interventions in this category provided some evidence of the potential impact of structured support for socialising in terms of improving the quantity and quality of social networks [32, 38, 39]. The two interventions which had a usual care comparator demonstrated significant improvements in social networks at 12-month (medium-effect size: 0.47) [32] and 24-month follow-up (OR: 1.8)—[38]) in the intervention groups. The third which compared supported socialisation with a financial stipend to the provision of finical stipend only demonstrated significant improvement in both groups which favoured the intervention, but did not reach significance. All three interventions targeted severe and enduring mental health problems such as psychosis and schizophrenia.
Terzian and colleagues targeted people under 45 years. Those with poor social networks (defined as five relationships) demonstrated a significant social network improvement (defined as an increase in number, frequency, importance, or closeness of relationships) at both 1-year (OR 1.8, 95% CI 1.2–2.8) and 2-year follow-up (OR 1.8, 95% CI 1.2–2.9) for the supported socialisation intervention which was delivered by professionals and lay facilitators (friends/family) [38]. The intervention was most effective for people who also demonstrated improvement in clinical, work or daily activity outcomes. For those who had no such improvement in these outcomes, the authors reported no impact of the intervention on social networks. The study reported that participants attached greater value to more distal ties than close friendships or confiding relationships [38].
Sheridan et al. [39] compared the effectiveness of a monthly stipend to support weekly leisure/social activity vs. monthly stipend plus supported social activity and friendship activities facilitated by people with no connection to mental health services. There were no significant differences between groups on social network outcome measures. However, there was a reduction in the number of people who had the most vulnerable types of networks post-intervention and increases in the weekly number of social contacts with friends in both groups [39]. Over the 10-month follow-up period, both groups demonstrated significant increases in social activities (e.g., going to the cinema, enjoying a conversation which favored the partnered group, but did not reach statistical significance), and increased social functioning, and decreased social loneliness [39].
Finally, Rivera et al. (2007) examined the outcomes of consumer-assisted case management, non-consumer-assisted case management and standard clinic-based care. Consumer-assisted case management involved matching service users with peers on socio-demographics and mental health experience to provide supported socialisation. The study found a significant increase (medium-effect size: 0.47) in the number of contacts from baseline to 12-month follow-up in consumer-assisted case management [32]. This effect was suggested to be due to increased contact with peer volunteers and professional staff, rather than with family/friends outside of health services. However, there were significant improvements in all conditions for other network variables including network density, numbers of people who helped the participant, and number of people who were helped by the participant.
Peer support
Castelein et al. [40] evaluated the effectiveness of a closed peer support group. This study demonstrated a significant improvement (small effect size: 0.4) in terms of contacts with peer facilitators outside of intervention activities and on ‘esteem support’ (e.g., asking for help, support and advice, receiving complements). However, esteem support did not extend to the number of other kin/non-kin relationships or to other measures of network quality or satisfaction with network support [40]. People who experienced greater distress from positive symptoms and a longer duration of illness were more likely to report improved social networks at follow-up, in contrast to those with higher distress from negative symptoms who were significantly less likely to improve their social networks [40].
Assertive community treatment
The three assertive community treatment interventions (Calsyn et al. [34], Tempier et al. [35], Thorup et al. [37]) demonstrated impact in terms of increasing the number of professionals in networks [34] and the number of significant others at 18-month follow-up (medium-effect size: 0.6) [35]. Increases in the size of lay/informal networks were identified as a trend in other studies, but did not reach statistical significance [34]. Other studies reported no differences between control and intervention groups at follow-up in relation to social network quantity, quality or the amount of social support received [34, 37]. Increased social network size at follow-up was closely related to younger age, being female, having completed A-levels, less negative symptoms, larger network size at entry [37].
One-to-one interventions
The two one-to-one interventions demonstrated no significant impact on social networks [33, 36], though one reported medium (0.7) effect sizes for increases in social support for those in the intervention group suggesting some improvement to social network quality outcomes [33].
Other outcome measures
Interventions demonstrating impact in terms of improving the quantity or quality of social networks either did not report other health-related outcome measures [34] or did not demonstrate significant intervention superiority [32, 38, 39]. However, both groups (stipend and stipend plus peer supported socialisation) in the trial by Sheridan et al. reported a significant reduction in depression symptomatology over the 10-month follow-up period (p = 0.001) [39].
Other included interventions demonstrated significant impact in terms of symptomatology [33, 35, 40], psychological distress [33], self-esteem [33], functioning [35], readmission to mental health services [36] and satisfaction with care [36]. Medium-reported effect sizes ranged from 0.5 to 0.7 demonstrating the direct impact of interventions aiming to improve network engagement may be independent from observable changes in social networks.
Economic evaluation
Only two studies reported data pertaining to the evaluation of the costs associated with the interventions [38, 40] with only one of these constituting a formal cost assessment [40]. Castelein et al. [40] registered all prospective healthcare costs for included participants and other costs associated with the intervention. Their mixed model analysis demonstrated no significant differences in the mean total costs for both the intervention and control group. Terzian included an economic assessment and concluded their intervention had the potential to be readily included in routine care without the need for supplementary resources [38].
Research feasibility and acceptability of evaluating social network interventions
Of the 2,226 participants randomised, 586 (26%) dropped out of the research follow-up and 1640 completed data collection at all time points. The lowest drop-out rates were identified in the supported socialisation intervention delivered by health professionals and natural facilitators [38] and the closed peer support intervention [40]. The highest withdrawal rates were found in the one-to-one recovery-focused intervention [36] and the supported socialisation with friendship intervention [40]. For the one-to-one recovery-focused intervention, the 18-month follow-up response rate was considered a limitation, but reasons for withdrawal were not discussed [36]. For the supported socialisation intervention, reasons for the high level of withdrawal which were concentrated in the intervention group included the emotional and practical demands of establishing and sustaining new friendships initiated during the intervention [39].
Most studies reported that participants and facilitators viewed the intervention positively with adherence not explained by demographic or clinical characteristics [34, 36, 40]. Data from associated process evaluations were lacking.
Patient and public involvement
No included studies provided detail on any formal patient and public involvement in either the design and delivery of the intervention or the randomised controlled trial. One study reported that an intervention was adapted following feedback from participants [33].
Discussion
We undertook a narrative synthesis of empirical data from randomised controlled trials to systematically examine whether social network interventions are effective in enhancing the quantity and quality of social networks for people with mental health problems. Despite the small number and inadequacies of the included studies, our analysis points to most promise of interventions which provide support for social activities supporting the findings of previous research [42, 43]. However, most studies (7/9) lacked requisite information to undertake the assessments of potential bias on at least one quality domain. Information on adherence to the candidate interventions was lacking in 7/9 studies, and detail on blinding of outcome assessors was omitted in 4/9 studies or assessed as high risk in another. Future research would benefit from more detailed descriptions of methods in order for quality assessments to be fully undertaken and to allow definitive conclusions about optimal treatments to be derived.
For interventions which were effective in enhancing social networks, effect sizes were generally small to moderate when compared to usual care. These benefits did not routinely translate to improvements in mental health outcomes, suggesting that more research is needed to investigate whether there is an embedding period beyond the follow-up periods in included studies [32, 38, 39]. Other studies which were not effective in improving social networks did provide evidence of demonstrable impact in a range of other outcomes (in particular assertive community outreach and one-to-one treatment) suggesting a more direct mode of action but one that might not be sustainable post-treatment without associated network improvements [33, 35, 36, 40]. More research is required to provide an in-depth understanding of the mechanisms underpinning such impacts [44]. For example, the extent to which specific properties of networks such as homophily (being together with similar others), weak tie contact or the opportunity for reciprocity might be candidate elements to include in future network interventions. One option is to undertake mixed-method systematic reviews to synthesise qualitative data which could be explored in relation to the available quantitative data on outcomes to identify potential mechanisms or determinants of behaviour change. This would allow hypotheses to be generated for future testing and would inform logic models for social network interventions to allow for theorizing to be initiated in terms of what works best for whom in what circumstances [45, 46]. Existing measures of social network size and quality may also not reflect more subtle changes in network enhancement (availability of acceptable support or collective efficacy within networks) which indicates the need for more sensitive measures of social networks. The development of a Patient-Reported Outcome Measure might allow for the quantification of social network structural and functional aspects by incorporating the perspectives of service user and carers themselves [47].
Only a small number of included studies highlighted factors associated with the effectiveness of social network interventions. However, there was emerging evidence of the potential influence of a number of factors. For example, people with better clinical prognoses experienced greater improvements to their social networks [38] as did people with better quality networks at baseline [37]. Older age and being male were negatively associated with enhanced social networks at follow-up periods [37]. This may reflect the findings in the wider literature which indicates that older people and men tend to have smaller social networks of poorer quality more generally and are more likely to face more challenges developing and sustaining social networks over time [48, 49]. Negative symptoms were associated with poorer quality of networks at follow-up [37, 40], whereas distress from positive symptoms was associated with enhanced social networks at follow-up [37]. Future research is required to examine mediating factors to guide future implementation [46].
Most interventions limited the types of network members included within networks to friends and family members and failed to incorporate alternative forms of network members identified as important to mental health management in the wider literature, including weak ties [7, 50], valued places, objects and activities [6, 7] and companion animals [51, 52]. This broader view of social network support was supported by the value attached to distal relationships by participants. Furthermore, complexities associated with establishing and maintaining friendships leading to withdrawal, and the equivalence in social networks of those involving financial stipend ± peer support [39], lend further support to the value of alternative network members [7].
Despite a number of included studies, reporting that the research processes were well received by participants and facilitators which suggest a willingness to participate in such evaluations [34, 36, 40], in-depth data on the feasibility of evaluating social network interventions were not reported and studies had an average drop-out rate in excess of 26%. There were also limited data in included manuscripts about intervention acceptability. The Medical Research Council’s guidance for the evaluation of complex intervention recommends the undertaking of process evaluation to understand the mechanisms through which interventions work and future evaluation should incorporate these in the design of evaluative studies [45]. Future research should also consider the minimum intervention period required, potential for intervention latitude—the freedom to undertake local adaptation which is critical for maximising intervention effect, ownerships and for promoting sustainability [53]—and consider the reasons for participant withdrawal and how to mitigate against these to inform intervention development and implementation.
Peer support in the design and delivery of mental health services has been shown to reduce hospital admissions and drive recovery-focused care, a core value enshrined in global health policy [54]. However, evidence in terms of using peer-supported socialisation outside formal mental health services, however, is mixed [55]. This review contributes to this debate by demonstrating that professional facilitators appear best placed to bring about increases in professional support within networks and peer workers are effective in developing relationships with service users that endure outside of health services [32, 40]. The review also supports other studies which have shown that, to make changes to whole networks and improve socialisation in the wider community, efforts are best focused outside of mental health services. This includes interventions drawing on lay workers that have no connection to formal service provision [56]. Potential reasons for this evident in the wider literature include expectations of acceptance by peers with similar experiences which were not realised in practice, limited instrumental resources and social networks of peer facilitators and the community stigma associated with mental health problems [56] Future research is required to understand optimal facilitation and what characteristics, training and support plans are required to effectively facilitate social network interventions for people with mental health problems [57].
This systematic review draws strength from the rigorous search strategy and extraction methods. To mitigate against bias, researchers independently screened all potentially eligible manuscripts with any conflicts resolved through consensus. Our research team included a range of health services researchers, practitioners and five patient and involvement (PPI) contributors. This enhanced the quality of the review in terms of the development of search terms and classification of interventions and resultant interpretation and presentation of findings. Specifically, PPI contributors suggested extracting information relating the PPI in included studies which illuminated the dearth of such activities, provided additional search terms not originally considered, enabled the context of interventions to be understood in more depth to support classification, and supported the development of recommendations for future research and practice. Analysis was hindered by the clinical and methodological heterogeneity of included studies and a lack of shared definitions and theoretical underpinnings of the term ‘social network’ and related concepts within manuscripts. The majority of included studies focused on schizophrenia or other forms of psychosis and generalisability to other mental health problems is unclear. There were a lack of economic data in included studies which meant that a full analysis in this regard was not possible. Despite employing no country or language restrictions, all identified studies were limited to USA and Europe which is an important limitation given that social networks are embedded in and reflect local cultures and contexts. Further research is required which incorporates wider geographical and cultural diversity.
Conclusion
We found preliminary evidence that social network interventions can be effective in improving social networks for people with mental health problems. However, this review demonstrates that evidence for social network interventions for people with mental health problems is in its infancy and further rigorous evaluation is required to inform evidence-based recommendations for health services. Future research should incorporate nested process evaluations to understand and optimise implementation, adequate patient and public involvement to increase intervention uptake and acceptability and high-quality cost data to allow in-depth economic modelling to be undertaken.
Notes
Defined as mental health problems which substantially interfere with or limits functional or occupational activities 3.Public Health England, Severe mental illness (SMI) and physical health inequalities: briefing. 2018, Public Health England: London.
Defined as “Features of social organisation, such as trust, norms and networks that can improve the efficiency of society by facilitating coordinated actions” 25. Putnam RD., R. Leonardi, and R. Nanenetti, Making democracy work: civic traditions in modern Italy. 1993, Princeton: Princeton University Press.
References
Kessler RC et al (2007) Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 6(3):168–176
Ferrari AJ et al (2014) The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study 2010. PLoS ONE 9(4):e91936
Public Health England (2018) Severe mental illness (SMI) and physical health inequalities: briefing. Public Health England, London
Chesney E, Goodwin GM, Fazel S (2014) Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry 13(2):153–160
O’Reilly P (1988) Methodological issues in social support and social network research. Soc Sci Med 26(8):863–873
Sweet D et al (2018) Personal well-being networks, social capital and severe mental illness: exploratory study. Br J Psychiatry 212(5):308–317
Brooks HL et al (2020) Negotiating support from relationships and resources: a longitudinal study examining the role of personal support networks in the management of severe and enduring mental health problems. BMC Psychiatry 20(1):50
Berkman LF et al (2000) From social integration to health: Durkheim in the new millennium. Soc Sci Med 51(6):843–857
Kawachi I, Berkman LF (2001) Social ties and mental health. J Urban Health Bull N Y Acad Med 78(3):458–467
De Vogli R, Chandola T, Marmot MG (2007) Negative aspects of close relationships and heart disease. Arch Intern Med 167(18):1951–1957
Christakis NA, Fowler JH (2007) The spread of obesity in a large social network over 32 years. N Engl J Med 357(4):370–379
Pescosolido BA (1992) Beyond rational choice: the social dynamics of how people seek help. Am J Sociol 97(4):1096–1138
Pescosolido BA (1991) Illness careers and network ties: a conceptual model of utilization and compliance. In: Albrecht G, Levy J (eds) Advances in medical sociology. JAI Press, Greenwich, p 161–184
Perry BL, Pescosolido BA (2012) Social network dynamics and biographical disruption: the case of “First-Timers” with mental illness. Am J Sociol 118(1):134–175
Vassilev I et al (2016) Social network type and long-term condition management support: a cross-sectional study in six European countries. PLoS ONE 11(8):e0161027
Vassilev I et al (2019) The role of collective efficacy in long-term condition management: a metasynthesis. Health Soc Care Commun 27(5):e588–e603
Igarashi T et al (2008) Culture, trust, and social networks. Asian J Soc Psychol 11:88–101
Satterwhite RC et al (2000) Culture and perceptions of self-other similarity. Int J Psychol 35:287–293
Jacobson D (1987) The Cultural Context of Social Support and Support Networks. Med Anthropol Q 1:42–67
Salehi A et al (2019) Bonding and bridging social capital in the recovery of severe mental illness: a synthesis of qualitative research. J Ment Health 28(3):331–339
Albert M et al (1998) Social Networks and Mental Health Service Utilisation - a Literature Review. Int J Soc Psychiatry 44(4):248–266
Rusca R et al (2021) Comparing the social networks of service users with long term mental health needs living in community with those in a general adult in-patient unit. Int J Soc Psychiatry 2021:00207640211017590
Perry BL (2006) Understanding social network disruption: the case of youth in foster care. Soc Prob 53(3):371–391
Evert H et al (2003) The relationship between social networks and occupational and self-care functioning in people with psychosis. Soc Psychiatry Psychiatr Epidemiol 38(4):180–188
Putnam RD, Leonardi R, Nanenetti R (1993) Making democracy work: civic traditions in modern Italy. Princeton University Press, Princeton
Daker-White G, Rogers A (2013) What is the potential for social networks and support to enhance future telehealth interventions for people with a diagnosis of schizophrenia: a critical interpretive synthesis. BMC Psychiatry 2013:13
Reeves D et al (2014) The contribution of social networks to the health and self-management of patients with long-term conditions: a longitudinal study. PLoS ONE 9:6
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Vassilev I et al (2013) Social networks, the “work” and work force of chronic illness self-management: a survey analysis of personal communities. PLoS ONE 8:4
McGowan J et al (2016) PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 75:40–46
Popay J et al (2006) Guidance on the conduct of narrative synthesis in systematic reviews a product from the ESRC methods programme. Lancaster University
Rivera JJ, Sullivan AM, Valenti SS (2007) Adding consumer-providers to intensive case management: does it improve outcome? Psychiatric Serv Washington (DC) 58(6):802–809
Ammerman RT et al (2013) Treatment of depressed mothers in home visiting: impact on psychological distress and social functioning. Child Abuse Negl 37(8):544–554
Calsyn RJ et al (1998) The impact of assertive community treatment on the social relationships of people who are homeless and mentally ill. Commun Ment Health J 34(6):579–593
Tempier R et al (2012) Does assertive community outreach improve social support? Results from the Lambeth Study of early-episode psychosis. Psychiatric Serv (Washington DC) 63(3):216–222
Johnson S et al (2018) Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet 392(10145):409–418
Thorup A et al (2006) Social network among young adults with first-episode schizophrenia spectrum disorders: results from the Danish OPUS trial. Soc Psychiatry Psychiatr Epidemiol 41(10):761–770
Terzian E et al (2013) Social network intervention in patients with schizophrenia and marked social withdrawal: a randomized controlled study. Can J Psychiat 58(11):622–631
Sheridan AJ et al (2015) Improving social functioning and reducing social isolation and loneliness among people with enduring mental illness: report of a randomised controlled trial of supported socialisation. Int J Soc Psychiatry 61(3):241–250
Castelein S et al (2008) The effectiveness of peer support groups in psychosis: A randomized controlled trial. Acta Psychiatr Scand 118(1):64–72
Sterne JAC et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. Br Med J 366:l4898
Anderson K, Laxhman N, Priebe S (2015) Can mental health interventions change social networks? A systematic review. BMC Psychiatry 2015:15
Webber M, Fendt-Newlin M (2017) A review of social participation interventions for people with mental health problems. Soc Psychiatry Psychiatr Epidemiol 52(4):369–380
Fletcher A et al (2016) Realist complex intervention science: applying realist principles across all phases of the Medical Research Council framework for developing and evaluating complex interventions. Evaluation 22(3):286–303
Moore, G.F., et al., Process evaluation of complex interventions: Medical Research Council guidance. BMJ, 2015. 350: p. h1258.
Kislov R et al (2019) Harnessing the power of theorising in implementation science. Implement Sci 14(1):103
Nelson EC et al (2015) Patient reported outcome measures in practice. BMJ 350:g7818
McLaughlin D et al (2010) Gender differences in social network size and satisfaction in adults in their 70s. J Health Psychol 15(5):671–679
Antonucci TC, Ajrouch KJ, Birditt KS (2014) The convoy model: explaining social relations from a multidisciplinary perspective. Gerontologist 54(1):82–92
Rogers A et al (2014) Why less may be more: a mixed methods study of the work and relatedness of “weak ties” in supporting long-term condition self-management. Implement Sci 9:1
Brooks HL et al (2018) The power of support from companion animals for people living with mental health problems: a systematic review and narrative synthesis of the evidence. BMC Psychiatry 18(1):31
Brooks H et al (2016) Ontological security and connectivity provided by pets: a study in the self-management of the everyday lives of people diagnosed with a long-term mental health condition. BMC Psychiatry 16(1):409
Ovretveit J (2011) Widespread focused improvement: lessons from international health for spreading specific improvements to health services in high-income countries. Int J Qual Health Care 23(3):239–246
Repper J, Carter T (2011) A review of the literature on peer support in mental health services. J Ment Health 20(4):392–411
Fisk D, Frey J (2002) Employing people with psychiatric disabilities to engage homeless individuals through supported socialization: the Buddies Project. Psychiatr Rehabil J 26(2):191–196
Davidson L et al (2004) Supported socialization for people with psychiatric disabilities: Lessons from a randomized controlled trial. J Commun Psychol 32(4):453–477
James E et al (2020) Mediating engagement in a social network intervention for people living with a long-term condition: a qualitative study of the role of facilitation. Health Expect 23(3):681–690
Funding
This project is funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0418-20011). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study. All extracted data are available with the manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix 1: Searches


Appendix 2: PRISMA Checklist
Section and Topic | Item # | Checklist item | Location where item is reported |
|---|---|---|---|
TITLE | |||
Title | 1 | Identify the report as a systematic review | Page 1 |
ABSTRACT | |||
Abstract | 2 | See the PRISMA 2020 for Abstracts checklist | Page 2 |
INTRODUCTION | |||
Rationale | 3 | Describe the rationale for the review in the context of existing knowledge | Pages 3–4 |
Objectives | 4 | Provide an explicit statement of the objective(s) or question(s) the review addresses | Pages 4–5 |
METHODS | |||
Eligibility criteria | 5 | Specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses | Table 1 |
Information sources | 6 | Specify all databases, registers, websites, organisations, reference lists and other sources searched or consulted to identify studies. Specify the date when each source was last searched or consulted | Page 6 |
Search strategy | 7 | Present the full search strategies for all databases, registers and websites, including any filters and limits used | Appendix 1 |
Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and if applicable, details of automation tools used in the process | Pages 6–7 |
Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators, and if applicable, details of automation tools used in the process | Pages 6–7 |
Data items | 10a | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g. for all measures, time points, analyses), and if not, the methods used to decide which results to collect | Pages 6–7 and Supplementary File 1 |
10b | List and define all other variables for which data were sought (e.g. participant and intervention characteristics, funding sources). Describe any assumptions made about any missing or unclear information | Pages 6–7 and Supplementary File 1 | |
Study risk-of-bias assessment | 11 | Specify the methods used to assess risk of bias in the included studies, including details of the tool(s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process | Page 8 and Supplementary File 1 |
Effect measures | 12 | Specify for each outcome the effect measure(s) (e.g. risk ratio, mean difference) used in the synthesis or presentation of results | Page 8 and Table 2 |
Synthesis methods | 13a | Describe the processes used to decide which studies were eligible for each synthesis (e.g. tabulating the study intervention characteristics and comparing against the planned groups for each synthesis (item #5)) | Page 7 |
13b | Describe any methods required to prepare the data for presentation or synthesis, such as handling of missing summary statistics, or data conversions | N/A | |
13c | Describe any methods used to tabulate or visually display results of individual studies and syntheses | Page 7 | |
13d | Describe any methods used to synthesize results and provide a rationale for the choice(s). If meta-analysis was performed, describe the model(s), method(s) to identify the presence and extent of statistical heterogeneity, and software package(s) used | Page 7 | |
13e | Describe any methods used to explore possible causes of heterogeneity among study results (e.g. subgroup analysis, meta-regression) | N/A | |
13f | Describe any sensitivity analyses conducted to assess robustness of the synthesized results | N/A | |
Reporting bias assessment | 14 | Describe any methods used to assess risk of bias due to missing results in a synthesis (arising from reporting biases) | Page 8 |
Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome | N/A |
RESULTS | |||
Study selection | 16a | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram | Figure 1 |
16b | Cite studies that might appear to meet the inclusion criteria, but which were excluded, and explain why they were excluded | Pages 5–6 and Table 1 | |
Study characteristics | 17 | Cite each included study and present its characteristics | Supplementary File 1 |
Risk of bias in studies | 18 | Present assessments of risk of bias for each included study | Supplementary File 1 |
Results of individual studies | 19 | For all outcomes, present, for each study: (a) summary statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g. confidence/credible interval), ideally using structured tables or plots | Supplementary File 1 and Table 2 |
Results of syntheses | 20a | For each synthesis, briefly summarise the characteristics and risk of bias among contributing studies | Page 8 |
20b | Present results of all statistical syntheses conducted. If meta-analysis was done, present for each the summary estimate and its precision (e.g. confidence/credible interval) and measures of statistical heterogeneity. If comparing groups, describe the direction of the effect | N/A | |
20c | Present results of all investigations of possible causes of heterogeneity among study results | N/A | |
20d | Present results of all sensitivity analyses conducted to assess the robustness of the synthesized results | N/A | |
Reporting biases | 21 | Present assessments of risk of bias due to missing results (arising from reporting biases) for each synthesis assessed | N/A |
Certainty of evidence | 22 | Present assessments of certainty (or confidence) in the body of evidence for each outcome assessed | N/A |
DISCUSSION | |||
Discussion | 23a | Provide a general interpretation of the results in the context of other evidence | Pages 14–16 |
23b | Discuss any limitations of the evidence included in the review | Page 16 | |
23c | Discuss any limitations of the review processes used | Page 16 | |
23d | Discuss implications of the results for practice, policy, and future research | Pages 14–16 | |
OTHER INFORMATION | |||
Registration and protocol | 24a | Provide registration information for the review, including register name and registration number, or state that the review was not registered | Page 5 |
24b | Indicate where the review protocol can be accessed, or state that a protocol was not prepared | Page 5 | |
24c | Describe and explain any amendments to information provided at registration or in the protocol | Page 5 | |
Support | 25 | Describe sources of financial or non-financial support for the review, and the role of the funders or sponsors in the review | Page 17 |
Competing interests | 26 | Declare any competing interests of review authors | Page 17 |
Availability of data, code and other materials | 27 | Report which of the following are publicly available and where they can be found: template data collection forms; data extracted from included studies; data used for all analyses; analytic code; any other materials used in the review | Page 17 |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brooks, H., Devereux-Fitzgerald, A., Richmond, L. et al. Assessing the effectiveness of social network interventions for adults with a diagnosis of mental health problems: a systematic review and narrative synthesis of impact. Soc Psychiatry Psychiatr Epidemiol 57, 907–925 (2022). https://doi.org/10.1007/s00127-022-02242-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02242-w