Abstract
Purpose
A cancer diagnosis can have a substantial impact on one’s mental health. The present study investigated the prevalence and predictors of psychiatric comorbidities in cancer patients at the time of their discharge from the hospital.
Methods
Psychiatric comorbidities were assessed shortly before hospital discharge and half a year after hospitalization using a structured clinical interview (SCID), based on the diagnostic and statistical manual of mental disorders (DSM-IV). Frequencies at both time points were estimated using percentages and corresponding 95% confidence intervals. Predictors of mental disorders were identified using binary logistic regression models.
Results
At time of hospital discharge, 39 out of 334 patients (12%) were diagnosed with a psychiatric comorbidity, and 15 (7%) were diagnosed half a year later. Among the diagnoses, adjustment disorders (3%) were most frequent at the time of hospital release, while major depression (3%) was the most frequent 6 months later. Having a mental disorder was associated with unemployment (odds ratio (OR) 3.4, confidence interval (CI) 1.1–10.9, p = 0.04). There was no evidence that school education (OR 2.0, CI 0.4–9.0, p = 0.38), higher education (OR 0.7, CI 0.2–2.4, p = 0.60), income (OR 1.0, CI 1.0–1.0, p = 0.06), tumor stage (OR 1.1, CI 0.4–3.2, p = 0.85), type of disease (OR 0.6, CI 0.2–2.1, p = 0.47), pain (OR 1.0, CI 1.0–1.0, p = 0.15), fatigue (OR 1.0, CI 1.0–1.0, p = 0.77), or physical functioning (OR 1.0, CI 1.0–1.0, p = 0.54) were related to the presence of a psychiatric comorbidity.
Conclusions
Unemployment was associated with at least a threefold increased risk of mental disorder, which highlights the need for special attention to be given to this subgroup of cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Confrontation with a life-threatening illness such as cancer can lead to anxiety, depression, and other mental health problems in many patients [1,2,3]. Furthermore, the treatment of this disease and health-related restrictions can be an additional burden for patients [4]. In particular, pain and fatigue have been found to be negatively associated with patients’ well-being and their daily lives [5,6,7]. As a consequence of the multifarious requirements of a cancer patient, one-third of them suffer from a psychiatric comorbid condition [8,9,10]. Particularly after diagnosis and at the beginning of the treatment, patients are exposed to a high level of psychological burden. Due to the fact that mental health problems are negatively associated with treatment adherence [11, 12] and cancer survival [13, 14], special attention should be given to such problems. However, they are not always recognized by physicians [15]; thus psychiatric comorbidities can lead to untreated side effects in clinical practice [16]. If left untreated, these mental health conditions can have far-reaching consequences not only for the patients, such as by developing a chronic disease [17], but also for the health care system, such as by increasing costs. For example, it has been shown that psychiatric comorbidity is associated with more frequent treatments and longer hospital stays [17,18,19].
Physical well-being (e.g., functioning, pain), medical (e.g., tumor stage, type of disease), and sociodemographic characteristics (e.g., age, sex) as well as psychosocial factors (e.g., social support) have been shown to predict anxiety and depressive symptoms in cancer patients [20,21,22,23]. The results regarding predictors of structured assessed mental disorders are inconclusive thus far.
This inconclusiveness may result from the fact that in studies on comorbidities, data collection is sometimes carried out using screening instruments and is at other times identified through comprehensive clinical interviews. The studies that have used structured clinical interviews to ascertain psychiatric comorbid diseases have shown that prevalence varies between 23 and 53% [3]. In a study with cancer patients of working age, pain (odds ratio (OR) 1.7), fatigue (OR 1.9), and unemployment (OR 2.0) emerged as predictors of comorbid mental health conditions [24]. In another study of acute care, younger age (< 40 years OR 3.1, 40–49 years OR 2.9), trauma (OR 1.6), and low levels of physical function (OR 2.4) emerged as predictors of the presence of a mental disorder, whereas employment status was not predictive [25]. A study based on national registry data found older age to be a risk factor for psychiatric comorbidities [2]. Results on sex differences have also been inconsistent. While in some studies, comorbidities were higher in female cancer patients [2, 16], others studies did not find any such differences [25, 26].
The aim of the present study is to examine the prevalence of psychiatric comorbidities in cancer patients before their hospital release and half a year later and to investigate potential predictors of comorbid mental health conditions based on the literature shortly before hospital release.
Methods
Design and data collection
In this prospective study, all patients admitted to the Visceral, Transplantation, Thoracic, and Vascular Surgery Departments, as well as the Otolaryngology, Radiation–Oncology, Neurosurgery, Urology, and Pneumology Departments of the Leipzig University Hospital between October 2012 and June 2014 for the treatment of cancer were eligible. The exclusion criteria were (a) no histologically confirmed malignancy, (b) age < 18 years, (c) dementia or cognitive restrictions, and (d) insufficient German language skills to participate. Study nurses contacted eligible patients about the content, procedure, and aim of the study shortly after their admission. Patients were approached upon hospitalization (t1), shortly before hospital discharge (t2), 3 months after baseline (t3), and 6 months after baseline (t4). Psychiatric comorbidity was assessed at t2 and t4. Written informed consent was obtained by study nurses from all participants prior to data collection. The study received ethical approval from the Institutional Review Board of Leipzig University (#210-12-02072012)..
Instruments
Psychiatric comorbidity was assessed by study nurses at t2 and t4 using a structured clinical interview (SCID-I) based on the diagnostic and statistical manual of mental disorders (DSM-IV). The SCID is a standardized diagnostic instrument for the assessment of mental health conditions [27]. The following syndromes were assessed: major depressive disorder single episode, dysthymic disorder, adjustment disorder, posttraumatic stress disorder, acute stress disorder, social phobia, specific phobia, general anxiety disorder, panic disorder, alcohol abuse, and alcohol dependence. All the interviewers in this study were trained in conducting the SCID before the start of the study. Each potential diagnosis was discussed by the study team, and in case of doubt, no diagnosis was given. Patients with a diagnosed psychiatric comorbidity in this study did not receive any further treatment.
Fatigue, pain, and physical functioning were measured with the Quality of Life Core Questionnaire of the European Organization for Research and Treatment of Cancer (EORTC), the EORTC QLQ-C30 [28]. The scores were calculated according to the EORTC guidelines [29]. The measures were scaled from 0 to 100, whereby higher scores on the physical functional scale and lower scores on the symptom scales (pain and fatigue) indicate better quality of life. Participants responded using a four-point Likert scale ranging from 0 (“not at all”) to 3 (“very much”). Overall, the scales showed good reliability: fatigue (three items, Cronbach’s alpha = 0.79), pain (two items, Cronbach’s alpha = 0.85), and physical functioning (five items, Cronbach’s alpha = 0.85).
Education pertained to (a) the patient’s highest level of primary or secondary education completed (college, postcompulsory education, compulsory education) and (b) the patient’s level of higher education completed (none, apprenticeship, higher, university). Both variables were further dichotomized into compulsory and postcompulsory for “low school education” (versus “high”) and no degrees or apprenticeship as “low higher education” (versus “high”).
To ascertain the equivalent income of every patient, the net household income (total income minus taxes) was weighted with the number of people living in the household and their age according to OECD (Organization for Economic Co-operation and Development) standards.
A patient’s employment status was classified as follows: patients were coded as “not employed” (versus “employed, in training or retired”) if they were not working at least halftime, were not in training, and were not retired.
Clinical data were ascertained from the medical records. Tumor stage was classified according to the Union for International Cancer Control [UICC] classification system [30] and was dichotomized with I + II = “low” and III + IV = “high”. If cancer was recurrent, metastatic or secondary, the type of cancer was classified as “advanced cancer” (versus “not advanced”).
Statistical analyses
Participants and nonparticipants were compared in terms of basic data available (age, sex, and tumor stage at presentation) using Pearson’s chi-squared and Fisher’s exact tests. Equally, patients who took part in an SCID interview were compared to those who declined concerning demographic data (age, sex), socioeconomic variables (income, school education, higher education, unemployment status), and medical information (tumor stage, type of cancer).
Frequencies of psychiatric comorbidities at t2 and t4 were estimated using percentages and corresponding 95% confidence intervals. To test potential predictors of psychiatric comorbidity, binary logistic regression analyses were performed with having a diagnosed comorbidity (yes/no) as the dependent variable. We only analyzed predictors at hospital discharge (t2) because of the small number of patients with psychiatric diagnoses at t4. Putative risk factors were determined a priori based on the literature and were stepwise included in the models. Independent variables that were not measured continuous were dichotomized before the analyses. The models included the following independent variables: age and sex (model 1); school education (high/low), higher education (high/low), income, unemployment status (yes/no) (model 2); tumor stage (high/low), type of disease (advanced/not advanced) (model 3); and pain, fatigue, and physical functioning at t2 (model 4). For these analyzes, an increase of ten observations in the sample size is necessary for each additional independent variable, whereby it should be noted that for categorical variables each factor level must be treated as one independent variable [31]. Hence, for our analyses, a minimum of 170 observations is necessary which we have fulfilled with our sample size of N = 254 (model 4). Data analyses were performed using IBM SPSS® Statistics Version 25.
Results
Nonresponder analysis
There was no evidence of differences in age (p = 0.44) or sex (p = 0.21) between participants and nonparticipants, but there were indications of differences in tumor stage at presentation (MParticipants = 3.0, MNonparticipants = 3.2 p = 0.06).
Sample characteristics
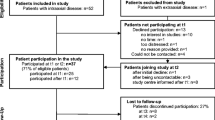
A total of 591 patients were admitted to the hospital during the study period. Twenty-six patients (4%) had to be excluded because cancer was not histologically confirmed, thereby leaving 565 patients eligible for the study. Of those patients, 123 (22%) declined study participation, resulting in 442 participants (Fig. 1). The most frequent tumor sites were head and neck (19%), prostate (18%), urinary organs (11%), brain (9%), lung (8%), and colorectal (7%). The mean age of the participants was 64 years (Table 1). The majority of the participants were male (70%), had advanced cancer (64%), and were either employed, retired or in training (70%).
Of the 442 participants, 355 (80%) participated in the study again at hospital discharge (t2), and of these, 334 (94%) agreed to take part in the SCID interview. Half a year after baseline (t4), 235 patients (53%) were interviewed, and 220 (94%) agreed to participate in an SCID interview. Participants with and without an SCID interview at t2 did not differ in age (p = 0.46), sex (p = 0.14), tumor stage at diagnosis (p = 0.39), type of cancer (p = 0.81), unemployment status (p = 0.09), school education (p = 0.56), or higher education (p = 0.62). However, there was evidence of differences in income (p = 0.03) between participants with and without an SCID interview; those with low income declined to take part more often.
Frequency of psychiatric comorbidity
At t2, 39 patients (12%) were diagnosed with a psychiatric comorbidity according to the SCID interview (Table 2). The most common comorbid diseases were adjustment disorder (n = 10, 3%), major depression (n = 8, 2%), and alcohol dependence (n = 7, 2%). One participant (0.3%) had two diagnoses: major depression and specific phobia. 6 months after baseline, 15 patients (7%) were diagnosed with at least one psychiatric disorder. Similar to t2, major depression (n = 7, 3%), specific phobia (n = 4, 2%), and alcohol dependence (n = 3, 1%) were the most common diagnoses. Two patients (1%) had a dual diagnosis: major depression and panic disorder, and major depression and specific phobia.
Predictors of psychiatric comorbidity
In the multivariate model, we found that when controlling for other socioeconomic and medical variables, unemployed patients had 3.4-fold higher odds of having a psychiatric comorbidity (95% CI 1.1–10.9, p = 0.04) at t2 than patients with full or halftime employment, patients who were in training, or pensioners (Table 3). Other socioeconomic variables (school, higher education and income) and medical characteristics, as well as fatigue, pain, and physical functioning, showed no association with psychiatric comorbidities in our study.
Discussion
The present study investigated the prevalence of comorbid psychiatric diagnosis according to SCID shortly before hospital discharge and half a year later in cancer patients.
Our results show that 12% of the patients suffered from a psychiatric comorbidity at time of hospital release, and 7% suffered from a psychiatric comorbidity half a year after their hospital stay. Compared to other studies that have reported a prevalence of 30% in acute care, the proportion in this study is considerably lower [8, 32]. This discrepancy may be explained by the fact that we did not include the consumption of nicotine and drug dependence as mental health conditions, although they were classified as one in the SCID interview. Furthermore, in our study, older patients (> 70 years) were more frequently included than in other studies (30% versus 20%) [25, 32]. Other studies have found that younger cancer patients are more likely to suffer from psychiatric comorbidities [25, 33]. Another reason for this difference could be that the abovementioned studies about mental disorders in acute care conducted their clinical interviews at the beginning of the patient’s hospital stay, while we did so at the time of hospital discharge. Furthermore, not all patients had just received their diagnosis; in some cases, the initial diagnosis had already occurred years ago.
In our study, the most frequent category of psychiatric comorbidity after hospitalization was adjustment disorder, followed by major depression. Half a year after baseline, major depression followed by a specific phobia were the most common. This result is similar to other studies that have found these disorders to be the most common [1, 24, 32].
Another aim of the study was to investigate predictors of psychiatric comorbidity shortly before hospital discharge. We found that unemployed patients were three times more likely to have a diagnosis according to the SCID compared to full- or halftime employed patients, persons in training, and pensioners. This result is in line with previous studies showing that cancer patients who are unemployed or those who had to suspend their work due to their disease suffer more frequently from comorbid psychiatric disorders [24, 34]. The number of mental disorders is also higher in unemployed persons in the general population [35]. The more common comorbidities in unemployed individuals may be because the loss of the job leads to a decrease in one’s social network and thus to reduced social support, which has been found to negatively influence the development of psychological comorbidities in cancer patients [36].
Clinicians should have a special focus on unemployed patients because they seem to be a specific at-risk group who may need additional support. Screening instruments could help in an economical way to identify if an unemployed patient is in need of health care. Referral to cancer support services or psycho-oncological treatment seems to be of great importance, especially because it has been shown that many cancer patients express a desire for psychosocial help [32]. In the case of patients with psychiatric comorbid conditions, clinicians should also point out the possibility of psychotherapeutic support since there is an undersupply of mental health care in cancer patients [24]. In addition, clinicians should discuss with their patients work-related issues and the idea of returning to work because these topics are often neglected [37]. If it then becomes apparent that support is necessary, the patients should be referred to occupational health professionals. However, there are also studies that report no association between employment status and psychiatric diagnoses in cancer patients [33, 38]. All the other predictors examined in this study showed no association with psychiatric comorbidities. However, this outcome could also have occurred because of the small sample size.
The study has several limitations that need to be considered when interpreting the results. First, we found psychiatric comorbidities much less often than in other studies with cancer patients; therefore, we do not know if our study sample is representative of the whole population. Another explanation may be that the prevalence of mental disorders varies between countries due to differences in the organization and financing of health care and social security systems. Since the German health care system offers comprehensive insurance coverage and a high level of health services, the lower number of psychiatric comorbidities in our study could be due to this fact. Second, we had no information about the psychiatric comorbidities of the patients before their cancer diagnosis, which could have been an important predictor as well. Third, we have to note that our results about associations between unemployment and mental disorders may be biased by the large differences in group size between employed and unemployed patients. Finally, because of the small number of mental disorders, we had to limit our analyses to a few predictors. We also did not examine predictors of psychiatric comorbidity half a year after hospitalization because of the low prevalence of mental disorders. Even with these limitations, the current study provides insight into predictors of psychiatric comorbidities in cancer patients who were assessed with structured clinical interviews at the time of their discharge from the hospital.
In summary, our study has shown that one in ten patients suffer from a psychiatric comorbidity at the end of their hospitalization. Unemployed patients should be given special attention because they are three times more likely to suffer from a mental disorder than other cancer patients. For these patients, it might be helpful for them to discuss their problems with hospital social services or to be referred to ambulant cancer care services.
Availability of data and material
The dataset analyzed in the current study is not available publicly as eligible patients were informed at the time of the survey their data would be stored securely and confidentially. The data may be available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Miovic M, Block S (2007) Psychiatric disorders in advanced cancer. Cancer 110(8):1665–1676. https://doi.org/10.1002/cncr.22980
Lee BO, Choi W-J, Sung NY et al (2015) Incidence and risk factors for psychiatric comorbidity among people newly diagnosed with cancer based on Korean national registry data. Psychooncology 24(12):1808–1814. https://doi.org/10.1002/pon.3865
Singer S, Das-Munshi J, Brähler E (2010) Prevalence of mental health conditions in cancer patients in acute care–a meta-analysis. Ann Oncol 21(5):925–930. https://doi.org/10.1093/annonc/mdp515
Henry DH, Viswanathan HN, Elkin EP et al (2008) Symptoms and treatment burden associated with cancer treatment. Results from a cross-sectional national survey in the US. Support Care Cancer 16(7):791–801. https://doi.org/10.1007/s00520-007-0380-2
Curt GA, Breitbart W, Cella D et al (2000) Impact of cancer-related fatigue on the lives of patients. New findings from the Fatigue Coalition. Oncologist 5(5):353–360. https://doi.org/10.1634/theoncologist.5-5-353
Tchekmedyian NS, Kallich J, McDermott A et al (2003) The relationship between psychologic distress and cancer-related fatigue. Cancer 98(1):198–203. https://doi.org/10.1002/cncr.11463
Zaza C, Baine N (2002) Cancer pain and psychosocial factors. J Pain Symptom Manag 24(5):526–542. https://doi.org/10.1016/S0885-3924(02)00497-9
Atesci FC, Baltalarli B, Oguzhanoglu NK et al (2004) Psychiatric morbidity among cancer patients and awareness of illness. Support Care Cancer 12(3):161–167. https://doi.org/10.1007/s00520-003-0585-y
Mehnert A, Brähler E, Faller H et al (2014) Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J Clin Oncol 32(31):3540–3546. https://doi.org/10.1200/JCO.2014.56.0086
Mitchell AJ, Chan M, Bhatti H et al (2011) Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings. A meta-analysis of 94 interview-based studies. Lancet Oncol 12(2):160–174. https://doi.org/10.1016/S1470-2045(11)70002-X
McDonough EM, Boyd JH, Varvares MA et al (1996) Relationship between psychological status and compliance in a sample of patients treated for cancer of the head and neck. Head Neck 18(3):269–276. https://doi.org/10.1002/(SICI)1097-0347(199605/06)18:3%3c269:AID-HED9%3e3.0.CO;2-Y
DiMatteo MR, Lepper HS, Croghan TW (2000) Depression is a risk factor for noncompliance with medical treatment. Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 160(14):2101–2107. https://doi.org/10.1001/archinte.160.14.2101
Giese-Davis J, Collie K, Rancourt KMS et al (2011) Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer. A secondary analysis. J Clin Oncol 29(4):413–420. https://doi.org/10.1200/JCO.2010.28.4455
Weihs KL, Enright TM, Simmens SJ et al (2000) Negative affectivity, restriction of emotions, and site of metastases predict mortality in recurrent breast cancer. J Psychosom Res 49(1):59–68. https://doi.org/10.1016/s0022-3999(00)00143-4
Fallowfield L, Ratcliffe D, Jenkins V et al (2001) Psychiatric morbidity and its recognition by doctors in patients with cancer. Br J Cancer 84(8):1011–1015. https://doi.org/10.1054/bjoc.2001.1724
Walker J, Hansen CH, Martin P et al (2014) Prevalence, associations, and adequacy of treatment of major depression in patients with cancer. A cross-sectional analysis of routinely collected clinical data. Lancet Psychiatry 1(5):343–350. https://doi.org/10.1016/S2215-0366(14)70313-X
Härter M, Reuter K, Aschenbrenner A et al (2001) Psychiatric disorders and associated factors in cancer. Results of an interview study with patients in inpatient, rehabilitation and outpatient treatment. Eur J Cancer 37(11):1385–1393. https://doi.org/10.1016/s0959-8049(01)00136-8
Häuser W, Wilhelm-Schwenk R, Klein W et al (2006) Einfluss psychischer Komorbidität auf die stationäre Verweildauer internistischer Patienten im G-DRG-System (The influence of psychiatric comorbidity on the length of hospital stay of medical inpatients within the German Diagnosis Related Groups System). Psychother Psychosom Med Psychol 56(9–10):370–375. https://doi.org/10.1055/s-2006-940179
Zabora J, BrintzenhofeSzoc K, Curbow B et al (2001) The prevalence of psychological distress by cancer site. Psychooncology 10(1):19–28. https://doi.org/10.1002/1099-1611(200101/02)10:1%3c19:aid-pon501%3e3.0.co;2-6
Godding PR, McAnulty RD, Wittrock DA et al (1995) Predictors of depression among male cancer patients. J Nerv Ment Dis 183(2):95–98. https://doi.org/10.1097/00005053-199502000-00005
Hill J, Holcombe C, Clark L et al (2011) Predictors of onset of depression and anxiety in the year after diagnosis of breast cancer. Psychol Med 41(7):1429–1436. https://doi.org/10.1017/S0033291710001868
Kim SH, Kang S, Kim Y-M et al (2010) Prevalence and predictors of anxiety and depression among cervical cancer survivors in Korea. Int J Gynecol Cancer 20(6):1017–1024. https://doi.org/10.1111/IGC.0b013e3181e4a704
Aschenbrenner A, Härter M, Reuter K et al (2003) Prädiktoren für psychische Beeinträchtigungen und Störungen bei Patienten mit Tumorerkrankungen – Ein systematischer Überblick empirischer Studien. Z Med Psychol 12:15–28
Singer S, Szalai C, Briest S et al (2013) Co-morbid mental health conditions in cancer patients at working age–prevalence, risk profiles, and care uptake. Psychooncology 22(10):2291–2297. https://doi.org/10.1002/pon.3282
Krauss O, Ernst J, Kuchenbecker D et al (2007) Prädiktoren psychischer Störungen bei Tumorpatienten. Empirische Befunde (Predictors of mental disorders in patients with malignant diseases: empirical results). Psychother Psychosom Med Psychol 57(7):273–280. https://doi.org/10.1055/s-2006-952034
Miller S, Lo C, Gagliese L et al (2011) Patterns of depression in cancer patients. An indirect test of gender-specific vulnerabilities to depression. Soc Psychiatry Psychiatr Epidemiol 46(8):767–774. https://doi.org/10.1007/s00127-010-0246-7
First MB, Spitzer Robert L, Gibbon M et al (1996) User’s guide for the structured clinical interview for DSM-IV Axis I disorders (SCID-I), clinician version. American Psychiatric Pr, Washington DC
Aaronson NK, Ahmedzai S, Bergman B et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30. A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376. https://doi.org/10.1093/jnci/85.5.365
Fayers PM, Aaronson NK, Bjordal K et al (2001) The EORTC QLQ-C30 Scoring Manual (3rdEdition). European Organisation for Research and Treatment of Cancer, Brussels
Sobin LH, Gospodarowicz MK, Wittekind C (eds) (2010) TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, Chichester
Verma JP (2013) Data analysis in management with SPSS software. Springer, New York
Singer S, Bringmann H, Hauss J et al (2007) Häufigkeit psychischer Begleiterkrankungen und der Wunsch nach psychosozialer Unterstützung bei Tumorpatienten im Akutkrankenhaus (Prevalence of concomitant psychiatric disorders and the desire for psychosocial help in patients with malignant tumors in an acute hospital). Dtsch Med Wochenschr 132(40):2071–2076. https://doi.org/10.1055/s-2007-985643
Akechi T, Okamura H, Nishiwaki Y et al (2001) Psychiatric disorders and associated and predictive factors in patients with unresectable nonsmall cell lung carcinoma. Cancer 92(10):2609–2622. https://doi.org/10.1002/1097-0142(20011115)92:10%3C2609:AID-CNCR1614%3E3.0.CO;2-K
Omne-Pontén M, Holmberg L, Burns T et al (1992) Determinants of the psycho-social outcome after operation for breast cancer. Results of a prospective comparative interview study following mastectomy and breast conservation. Eur J Cancer 28A(6–7):1062–1067. https://doi.org/10.1016/0959-8049(92)90457-d
Fryers T, Melzer D, Jenkins R (2003) Social inequalities and the common mental disorders. A systematic review of the evidence. Soc Psychiatry Psychiatr Epidemiol 38(5):229–237. https://doi.org/10.1007/s00127-003-0627-2
Mehnert A, Lehmann C, Graefen M et al (2010) Depression, anxiety, post-traumatic stress disorder and health-related quality of life and its association with social support in ambulatory prostate cancer patients. Eur J Cancer Care (Engl) 19(6):736–745. https://doi.org/10.1111/j.1365-2354.2009.01117.x
Verbeek J, Spelten E, Kammeijer M et al (2003) Return to work of cancer survivors. A prospective cohort study into the quality of rehabilitation by occupational physicians. Occup Environ Med 60(5):352–357. https://doi.org/10.1136/oem.60.5.352
Akechi T, Okuyama T, Sugawara Y et al (2004) Major depression, adjustment disorders, and post-traumatic stress disorder in terminally ill cancer patients. Associated and predictive factors. J Clin Oncol 22(10):1957–1965. https://doi.org/10.1200/JCO.2004.08.149
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was funded by the German Federal Ministry of Health (grant number NKP-332-026).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SS received a grant from Pfizer, honoraria from Lilly, and lecture fees from Pfizer, Bristol-Myers Squibb, and Boehringer Ingelheim; all were outside of this study. All other authors declare that they have no conflict of interest.
Ethical approval
All procedures performed within this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments. Approval was granted by the Ethics Committee of University of Leipzig (#210–12-02072012).
Consent to participate
Informed consent was obtained from all individual participants included.
Consent to publish
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roick, J., Danker, H., Kersting, A. et al. Predictors of psychiatric comorbidity in cancer patients at the time of their discharge from the hospital. Soc Psychiatry Psychiatr Epidemiol 57, 553–561 (2022). https://doi.org/10.1007/s00127-021-02138-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-021-02138-1