Abstract
Purpose
Maternal depression has been associated with bonding difficulties and lower maternal sensitivity in observed mother–infant interactions. However, little research has examined the impact of disordered personality traits in mothers on these outcomes. We investigated the association between disordered personality traits in mothers measured during pregnancy and postnatal (a) self-reported bonding with infant; (b) observational mother–infant interactions.
Methods
Five hundred fifty-six women were recruited during early pregnancy and subsequently followed up at mid-pregnancy (approximately 28 weeks’ gestation) and when infants were aged approximately 3 months (n = 459). During early pregnancy, data were collected on disordered personality traits (using the Standardised Assessment of Personality Abbreviated Scale) and depressive symptoms (using the Edinburgh Postnatal Depression Scale). At 3 months postpartum, self-reported perceived bonding (using the Postpartum Bonding Questionnaire) were collected. A sub-sample of women additionally provided observational mother–infant interaction data (n = 206) (coded using the Child–Adult Relationship Experimental Index).
Results
Higher disordered personality traits was not associated with maternal perceptions of bonding impairment, but was associated with reduced maternal sensitivity during observational mother–infant interactions [adjusted for age, education, having older children, substance misuse prior to pregnancy, infant sex and gestational age: coefficient = − 0.28, 95% CI = − 0.56 to − 0.00, p < 0.05]. After adjusting for depressive symptoms, the association was attenuated [coefficient = − 0.19, 95% CI = − 0.48 to 0.11, p = 0.217].
Conclusions
Mothers with disordered personality traits did not perceive themselves as having bonding impairments with their infants but were less sensitive during observed interactions, though depressive symptoms attenuated this relationship. Both depression and disordered personality traits need to be addressed to optimize mother–infant interactions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Substantial evidence demonstrates an association between perinatal mental disorders and adverse child social, emotional, behavioral, cognitive and health outcomes, with postpartum mother–infant interactions being a key mediator of these relationships [1,2,3,4,5]. Core aspects of mother–infant interactions include maternal sensitivity (mother’s ability to perceive and respond appropriately to her infant’s emotional and behavioral signals) and disrupted interactions such as maternal unresponsiveness and control or intrusiveness [6, 7]. To date, the research agenda has been largely driven by concerns about maternal depression and its impact on adverse mother–infant interactions. This literature has demonstrated an association between perinatal maternal depression and a range of negative child outcomes (including behavioral, emotional and cognitive development) [3, 5, 8,9,10]. For this reason, research into the prevention and treatment of maternal depression has become a priority, with the antenatal period now recognized as an ideal time to identify and implement interventions for depression [11]. However, other maternal characteristics are likely to be important in determining the quality of mother–infant interaction and may require tailored interventions: personality disorder, for example, is a risk factor for depression [12, 13] and as a distal exposure, may need specific interventions.
Personality disorders are characterized by inflexible and unstable patterns of thoughts, feelings and behaviors that are associated with impaired interpersonal functioning [14]. Three systematic reviews have reported that personality disorders are associated with impaired parenting behaviors [15,16,17]. Most of this literature has focused on borderline personality disorder and derives from clinical samples. This small but important body of research suggests that borderline personality disorder is associated with lower maternal sensitivity, lower perceived bonding, increased maternal intrusiveness (control), greater maternal unpredictability, less structured maternal interactions and reduced vocal and imitative maternal responses, compared to mothers without borderline personality disorder [15,16,17,18,19,20,21,22,23,24]. It has been suggested that such behaviors might be a result of mothers’ with borderline personality disorder being unable to correctly identify infants’ emotional cues and respond to them appropriately [25]. Another study found mothers with Cluster A personality disorder (schizoid, schizotypal, or paranoid) and depression were less sensitive towards their infants, compared to mothers with only personality disorder or depression, suggesting that the comorbidity of the two disorders are important to consider [26].
In community settings, fewer individuals meet diagnostic criteria for personality disorder thresholds, yet, disordered traits might still be present. Thus, taking a dimensional approach to measuring personality disorder symptoms may be more appropriate for research in community samples [27,28,29,30,31,32], and more relevant for public health. As disordered personality traits are on a spectrum, diagnostic personality disorder would be considered at the severe end of the spectrum. This may be associated with extreme problems with interpersonal relationships, such as the relationship between a mother and her infant. Indeed, recent studies have reported an association between disordered personality traits in mothers and increased emotional and behavioral problems among offspring during childhood and adolescence, independent of maternal depression [30, 31]. However, studies on the mechanisms underpinning these associations are needed.
To our knowledge, no studies have investigated the prospective association between disordered personality traits, measured during pregnancy, and early mother–infant interactions; as maternal personality is rarely recorded in perinatal mental health studies, and assessing mother–infant interactions objectively and reliably is time consuming and challenging. This is an important gap in the literature because the identification of an association between disordered personality traits in mothers and mother–infant interactions could inform the development of tailored preventative interventions [33, 34].
Aims of the study
The objective of the current study was to investigate whether disordered personality traits in mothers measured during pregnancy are associated with postnatal (a) mother’s self-report of perceived bonding with her infant and (b) observed mother–infant interaction patterns. We hypothesized that higher disordered personality traits would be prospectively associated with higher maternal perceived impaired bonding and lower observed maternal sensitivity, and higher ratings on maternal control. As mother–infant interactions patterns are derived from the dyadic interaction between the mother and the baby, we also report on infant behavioral patterns.
Method
Participants and general procedures
The participants (mother and infant dyads) were derived from two linked datasets (n = 556) recruited for a research program examining the effectiveness of perinatal mental health services for mothers with mental illness (ESMI) https://www.kcl.ac.uk/ioppn/depts/hspr/research/ceph/wmh/projects/a-z/esmi.aspx [35, 36]. Recruitment was based in South-East London, a socioeconomically and ethnically diverse population [37], and used a stratified sampling design to address one of the original study questions on the effectiveness of the Whooley questions [36]. Ethical approval for the study was obtained by the National Research Ethics Service, London Committee—Camberwell St Giles (Ref No. 14/LO/0075). Exclusion criteria were women under 16 years of age, lacking capacity to consent, and termination or miscarriage prior to baseline interview. Eligible pregnant women were provided with information sheets and had the opportunity to ask questions prior to providing informed consent. Women consenting to participate were recruited into the study within 3 weeks of their first antenatal booking appointment, at around 10–12 weeks gestation.
Data were collected between November 2014 and June 2017. Participants completed the baseline interview during early pregnancy (n = 556) and then follow-up interviews during mid-pregnancy (approximately 28 weeks’ gestation, n = 508, 91% follow-up rate) and approximately 3 months postpartum (n = 484, 87% follow-up rate). During the 3-month postpartum follow-up, when funding became available, a sub-sample of women (n = 264) were additionally asked to take part in an observational mother–infant interaction video recording during a home visit (78% agreed, n = 206). See Fig. 1 for flowchart of participants through the study time points. Women who experienced miscarriage or stillbirth were not asked to complete infant-related measures.
Measures
Pregnancy measures: maternal mental health
Disordered personality traits
The Standardised Assessment of Personality Abbreviated Scale (SAPAS) is an eight-item, researcher-administered, screening questionnaire/mini-interview which measures disordered personality traits [38]. Items correspond to descriptive statements about the person scored as either 0 = “no” or 1 = “yes”, measuring difficulties such as making friends, trust, excessive worrying and impulsivity. Responses are summed (item 3 reverse scored) for a total score ranging between 0 and 8. Higher scores indicate greater number of disordered personality traits. In clinical populations, a cut-off of ≥ 3 is indicative of high risk of the presence of personality disorder [38]. The measure demonstrates good sensitivity and specificity (0.94 and 0.85, respectively) with the structural clinical interview for DSM-IV Axis II borderline personality disorders (SCID-II) [38, 39]. In the current analysis we used the continuous scale for all main analyses and cut-off (binary) for descriptive statistics.
Maternal depressive symptoms
The Edinburgh Postnatal Depression Scale (EPDS) is a 10-item self-report questionnaire for perinatal depression and validated in 20 languages [40]. The measure was included in the self-report questionnaire pack during the baseline (early pregnancy) and mid-pregnancy follow-up time point. The mean EPDS score from baseline and mid-pregnancy was used to generate a variable to represent women’s depressive symptoms during pregnancy.
Borderline personality disorder
The structured clinical interview DSM-IV Axis II borderline personality disorders is a researcher-administered semi-structured diagnostic interview using the sub-section module (SCID-II), which was utilized to measure DSM-IV Axis II borderline personality disorders [39]. The SCID-II was administered at the baseline interview.
Outcomes at 3 months postpartum
Mothers perceived bonding: Postpartum Bonding Questionnaire (PBQ)
A 25-item self-administered questionnaire, designed to provide an early indication of disorders within mother–infant relationships through the assessment of a mother’s feelings and attitudes towards her infant [41]. Items are rated on a six-point scale from 0 = “always” to 5 = “never”. When the statement reflects a negative emotion or attitude, the scoring is reversed. Total scores are calculated by summing the 25 items (scores range between 0 and 125). Higher scores indicate more impaired bonding.
Observational mother–infant interactions: CARE-Index
Mothers were filmed for 5 min during a free play session with their infants. Videos were coded using The Child–Adult Relationship Experimental Index (CARE-Index) [42, 43] which has several subscales to measure mother–infant interaction patterns; including maternal scales (sensitive, controlling and unresponsive) and infant scales (cooperative, difficult, compulsive and passive). This is a reliable and valid coding system for infants aged 0–15 months and validated across different social class and ethnic backgrounds [43, 44]. Coding was performed by a highly experienced and independent CARE-Index coder certified with Level II+ (research level reliability certified by the Family Relations Institute). The coder was blind to women’s mental health status and the specific aims of the study. All patterns are rated on a scale of 0–14, with higher scores indicating a higher rating of the particular pattern. The interaction patterns of interest for the current analysis were sensitivity and control for the maternal patterns. Also, cooperative, difficult and compulsive for the infant patterns (for descriptions see Table S1 in supplementary materials).
Sociodemographic characteristics
Information about maternal sociodemographic characteristics (age, information on if women had older children, and education) were obtained at the baseline interview during early pregnancy. Age was treated as a continuous variable in years and education was divided into three categories to indicate highest level of maternal education: none/school level, college/diploma/higher certificate/training and degree level/postgraduate qualification. Information regarding infant factors such as sex and date of birth (to calculate gestational age at birth) was collected during the 3-month home visit.
Maternal substance use
Information about maternal substance misuse was collected in two self-reported questionnaires administered at the baseline interview during early pregnancy, which asked about use within the previous year (covering mostly pre-conception period). The Alcohol Use Disorders Identification Test (AUDIT) includes 10-items regarding alcohol-related consumption [45], with two questions on quantity and frequency of alcohol use, a question on binge drinking, two CAGE questions, and five DSM-III criterion questions. The rating are on a five-point scale (the first item is scored from 0 = “never” to 4 = “4 or more times a week”; the second item from 0 = “1 to 2” to 4 = “ten or more” and the following six items from 0 = “never” to 4 “daily or almost daily”. The final two items are rated on a three-point scale: 0 = “no”, 2 = “yes, but not in the past year”, and 4 = “yes during the past year”). The total score ranged between 0 and 40, with the cut-off score of ≥ 8 as indicative of harmful or hazardous drinking [45, 46]. The Drug Use Disorders Identification Test (DUDIT) is an 11-item questionnaire of drug-related problems [47], rated on a five-point scale (the first two items are scored from 0 = “never” to 4 = “4 or more times a week”; the third item from 0 = “0” to 4 = “seven or more”, and the following six items from 0 = “never” to 4 “daily or almost every day”. The final two items are rated on a three-point scale: 0 = “no”, 2 = “yes, but not over the past year”, and 4 = “yes over the past year”). The total scores ranged between 0 and 44, with a score of ≥ 2 indicating drug-related problems for women.
Missing data
Four participants (1%) had missing data on the SAPAS measure and eight participants (2%) had missing data on the PBQ. Therefore, 459 participants had complete data available for analysis investigating the association between disordered personality traits (SAPAS) and maternal perceptions of bonding (PBQ). There was missing data on sex for one infant. One infant had missing data on date of birth and therefore gestational age at delivery could not be accurately calculated. There was some missing data in the baseline and 28 weeks EPDS scores. Consistent with our previous methods [36], where women who had 1–3 items (10–30%) missing, the predictive mean matching option in Stata (v15.0) was used to impute missing EPDS data. Of the women that were included the PBQ analysis (n = 459), 14 (3%) had missing data on the alcohol use measure (AUDIT) and 10 (2%) on the drug use measure (DUDIT). As a consequence, the sub-sample of women included the mother–infant interaction analysis (n = 206) had some missing data; 7 (3%) had missing data on the AUDIT and 4 (2%) on the DUDIT. As there were < 5% missing data on these variables, no data imputation was conducted. There were no other missing data for variables used in the statistical analysis.
Statistical analysis
Data were managed and analyzed using Stata v.15 [48]. We checked the representativeness of our sample, by comparing sociodemographic characteristics of women in the base population (women booking at the maternity site during the study recruitment period) with the cohort with complete PBQ data and the sub-sample with mother–infant interaction data. Characteristics of women with high levels of disordered personality traits (cut-off ≥ 3) versus women with low disordered personality traits were compared using Chi-square tests (Fisher’s exact test for cells n < 5) for categorical variables and independent t tests for continuous variables. The main predictor variable (SAPAS score) and outcome variables of mothers’ perception of bonding with infant (PBQ) and patterns of mother–infant interactions patterns were initially investigated by tabulating means, standard deviations and Pearson correlations between variables.
Unadjusted linear regressions were run to investigate the associations between disordered personality traits and outcomes (PBQ and mother–infant interaction patterns) (model 1). Based on previous literature [5, 10, 49], potential confounding variables associated with both the exposure and outcomes were selected a priori. On this basis, maternal age, education, mothers having an older child, infant sex and gestational age at birth were included in the multivariable regression analysis (model 2). In addition, we investigated whether any associations were attenuated by maternal substance use (alcohol and drugs, model 3), and maternal depressive symptoms during pregnancy (model 4).
Prior to analysis, data were checked for accuracy, missing data, outliers and normality. All outcome variables were slightly skewed. Therefore, in a sensitivity analysis we re-ran models 2, 3 and 4 with log transformed outcome measures that were significantly associated with disordered personality traits. In all cases, the transformed outcomes showed the same pattern of findings, therefore untransformed results are presented to facilitate interpretability of findings.
Results
Sample representativeness
Comparison of key demographics on age, ethnicity and number of children between the base population, study baseline participants (n = 556), the sample with PBQ data (n = 463) and the sub-sample with mother–infant interaction data (n = 206) are presented in Table S2 in supplementary materials. The samples were broadly similar (in age, ethnicity and number of children) to those in the base population.
Descriptive statistics
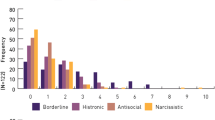
Of the women with complete SAPAS and PBQ data, the mean SAPAS score was 1.71 (SD: 1.42) (n = 459); 103 (22%) met criteria for high levels of disordered personality traits (SAPAS cut-off ≥ 3) and 356 (78%) for lower levels of disordered personality traits (SAPAS score < 3). Mothers with high SAPAS scores had significantly higher levels of depressive symptoms during pregnancy. For comorbidity with depressive symptoms during pregnancy (EPDS cut-off ≥ 13): 62 women (13%) met criteria for only high disordered personality traits, 50 (11%) for only high depressive symptoms, 41 (9%) with comorbid high disordered personality traits and depressive symptoms, and 306 controls (67%) with low symptoms of disordered personality traits and depression.
Of the 206 dyads who provided mother–infant interaction data, 62 women (30%) met criteria for high levels of disordered personality traits and 144 (70%) for lower levels of disordered personality traits. For comorbidity with depressive symptoms during pregnancy, 33 women (16%) met criteria for only high disordered personality traits, 26 (13%) for only high depressive symptoms, 29 (14%) with comorbid high disordered personality traits and depressive symptoms, and 118 controls (57%) with low symptoms of disordered personality traits and depression.
Table 1 displays maternal and infant characteristics. Overall, mothers with high levels of disordered personality traits were younger, less educated, less likely to be employed, have lower income, less likely to be in a relationship, more likely to meet diagnostic criteria for borderline personality disorder and more likely to report harmful or hazardous alcohol consumption within the year prior to the study baseline interview. Infants were on average 4 months old (range 2.5–5.5 months) and with an equal distribution of male and female infants.
Table 2 presents descriptive statistics of outcome variables PBQ and mother–infant interaction patterns. Inter-correlations for disordered personality traits (exposure) and outcomes (PBQ and mother–infant interactions patterns) are presented in Table S3 in supplementary materials. As expected, there were high correlations between maternal sensitivity and infant cooperation and maternal control and infant compulsivity.
Unadjusted univariate analysis
In the unadjusted linear regression analysis, higher levels of disordered personality traits (SAPAS scores) were not associated with maternal perceptions of bonding with their infant (PBQ), but were associated with lower maternal sensitivity, lower infant cooperation and higher maternal control during observed mother–infant interactions (Table 3, model 1). There was no evidence for an association between disordered personality traits in mothers and other infant patterns.
Multivariable regression analysis
After adjusting for maternal age, mothers having older children, education, infant sex and gestational age at birth (model 2), higher disordered personality traits remained significantly associated with lower maternal sensitivity (see Table 3). After further adjusting for maternal substance use (alcohol and drugs) (model 3, Table 3), higher disordered personality traits were still significantly associated with lower maternal sensitivity. Finally, after adjusting for maternal depressive symptoms during pregnancy (model 4, Table 3), there was an attenuation of the association between disordered personally traits and mother–infant interaction outcomes including maternal sensitivity. The final model 4 for outcome maternal sensitivity is provided with all variables in Table 4 (adjusted R2 fit 7%). Higher maternal age was the only exposure significantly associated with higher levels of maternal sensitivity in the final adjusted model (Table 4). To investigate the possibility that maternal depressive symptoms moderates the association between disordered personality traits and maternal sensitivity, we conducted a post hoc analysis which tested for the significance of a SAPAS*EPDS interaction term in the regression model. But there was no evidence of moderation (coefficient 0.01, 95% CI − 0.04 to 0.06, p = 0.629).
Sensitivity analysis
The findings were replicated when repeating analysis using log transformed outcome data (maternal sensitivity) for model 2 (transformed coefficient − 0.04, 95% CI − 0.08 to − 0.00, p = 0.038), model 3 (transformed coefficient − 0.04, 95% CI − 0.08 to 0.00, p = 0.043) and model 4 (transformed coefficient − 0.03, 95% CI − 0.07 to 0.01, p = 0.181).
Discussion
In this prospective study of a representative sample of inner-city mothers, the presence of higher levels of disordered personality traits measured during pregnancy were prospectively associated with subsequent impairments in maternal sensitivity assessed using independent ratings of observational mother–infant interactions. Higher levels of disordered personality traits were not, however, associated with maternal self-report of bonding impairments. Depressive symptoms attenuated the association with maternal sensitivity, suggesting that depressive symptoms are potentially an important driver of poorer quality mother–infant interactions in women with high levels of disordered personality traits.
Disordered personality traits have similarly been reported to be associated with mother–child interaction deficits in cross-sectional studies with toddlers [50] and older children [51]. Given that accumulating evidence is suggesting an association between disordered personality traits in mothers and child outcomes [30, 31], maternal sensitivity could potentially be a modifiable target for interventions, as maternal sensitivity during early infancy predicts mother–child attachment formation, which is known to influence later child outcomes [52].
The overall model fit statistics (R2) were low, suggesting that there are many other factors influencing mother–infant interactions which were not accounted for by our model. Such factors might include prenatal fetal attachment, child temperament, substance abuse during pregnancy, and domestic abuse [5, 53, 54], which could be investigated in future research. Although we investigated depressive symptoms as a moderator, we are likely to have been underpowered to detect moderation and thus the role of maternal depression also deserves further attention.
Strengths and limitations
There are several strengths of the current study. The sample was broadly representative of the base population and language interpreters were used to include non-English speaking women. The prospective data collection allows us to make inferences regarding the direction of associations. We accounted for socioeconomic factors, infant factors (sex and gestational age at birth) and maternal depressive symptoms, and used an observational measure to record mother–infant interaction with a culturally sensitive and well validated coding system rated independently with the coder masked to the mothers mental health status and study objectives [43, 44]. Also, this study is larger than most previous studies with observational data (total n < 90) [18,19,20,21, 23]. Limitations include use of a different construct in measuring self-reported maternal bonding which may not map onto perceptions of interaction difficulties, and a smaller sample size of women participating in the mother–infant interaction component of the study (due to funding limitations), compared to those participating in self-report PBQ data collection. It is also striking that the overall CARE-Index coding scores were somewhat lower than expected [43]; however, there are reasons to believe that this generation may be showing lower sensitivity scores [55, 56] compared to participants of past studies, even in healthy mothers with no mental disorders [57]. Finally, although the interviewer-administered screen used to measure disordered personality traits (SAPAS) in the current study is validated [38, 58], rapid (reducing participant burden) and shown to capture variance specific to personality disorder in community samples [59], the SAPAS scores have also been reported to correlate with other Axis I mental disorders (anxiety and depression) [60]. This potentially makes it hard to disentangle the specific symptomologies that might be associated with mother–infant interactions. The SAPAS (as well as other similar screening tools) also lack the clinical depth that would be provided by a diagnostic “gold standard” interview. However, the best way to conceptualize personality disorder is highly debated [61, 62] and ICD-11 is adopting a quasi-dimensional classification for personality disorder, one which is relevant for community samples such as ours [63]. Future research should attempt to replicate our findings using both dimensional personality traits and a more detailed “gold standard” measure of personality disorders with a larger sample of women meeting diagnostic criteria for personality disorders.
Clinical implications
The study of disordered personality traits in mothers and the impact of these traits on interactions between mothers and infants have received very limited research attention. Our findings suggest that women who present with high disordered personality traits have impaired interaction with their infants, but may have little awareness of their difficulties as they did not self-report more bonding difficulties than controls. These difficulties appear to be at least partly due to depressive symptoms, though other factors are also likely to play a large role.
Currently there is limited support in place for women with disordered personality traits (or indeed for women with personality disorder) in perinatal mental health services internationally. Nevertheless, interventions focusing on mother–infant interactions have been shown to impact positively on mothers emotional well-being and improve mother–infant relationship quality [5, 64]. Most women want to provide the best possible care for their new born baby and may be particularly open to accepting support in these first few months of the baby’s life. Thus, interventions tailored for women with disordered personality traits could usefully focus on supporting the mother–baby relationship. Women with disordered personality traits may find such an approach less stigmatizing and have greater engagement with it than interventions focused her personality disordered symptoms alone. In addition, identification and treatment of depressive symptoms could improve both maternal and child outcomes [65].
Conclusions
To our knowledge, this is the first study to provide evidence for the influence of disordered personality traits on subsequent maternal sensitivity assessed in dyadic interaction between a mother and her baby, independent of socioeconomic factors and maternal pre-conception substance misuse. Associations were attenuated by depressive symptoms, suggesting that depressive symptoms may be on the causal pathway. Further evidence on the influence of co-morbid disordered personality traits and depressive symptoms are required to inform development of interventions that focus on mother–infant interactions [5, 64, 66].
References
Alink LR, Mesman J, Van Zeijl J, Stolk MN, Juffer F, Bakermans-Kranenburg MJ, Van Ijzendoorn MH, Koot HM (2009) Maternal sensitivity moderates the relation between negative discipline and aggression in early childhood. Soc Dev 18(1):99–120
Moss E, Dubois-Comtois K, Cyr C, Tarabulsy GM, St-Laurent D, Bernier A (2011) Efficacy of a home-visiting intervention aimed at improving maternal sensitivity, child attachment, and behavioral outcomes for maltreated children: a randomized control trial. Dev Psychopathol 23(1):195–210
Murray L, Halligan SL, Cooper PJ (2010) Effects of postnatal depression on mother–infant interactions, and child development. In: Wachs TBG (ed) Handbook of Infant Development. Wiley-Blackwell, Malden
Letourneau NL, Kozyrskyj AL, Cosic N, Ntanda HN, Anis L, Hart MJ, Campbell TS, Giesbrecht GF (2017) Maternal sensitivity and social support protect against childhood atopic dermatitis. Allergy Asthma Clin Immunol 13(1):26
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, Pariante CM (2014) Effects of perinatal mental disorders on the fetus and child. Lancet 384(9956):1800–1819
Raby KL, Roisman GI, Fraley RC, Simpson JA (2015) The enduring predictive significance of early maternal sensitivity: social and academic competence through age 32 years. Child Dev 86(3):695–708
Ainsworth MS (1979) Infant–mother attachment. Am Psychol 34(10):932
Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D (2011) Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev 14(1):1–27. https://doi.org/10.1007/s10567-010-0080-1
Grace SL, Evindar A, Stewart DE (2003) The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of the literature. Arch Womens Ment Health 6(4):263–274. https://doi.org/10.1007/s00737-003-0024-6
Goodman SH, Bakeman R, McCallum M, Rouse MH, Thompson SF (2017) Extending models of sensitive parenting of infants to women at risk for perinatal depression. Parenting 17(1):30–50
Letourneau NL, Dennis CL, Cosic N, Linder J (2017) The effect of perinatal depression treatment for mothers on parenting and child development: a systematic review. Depress Anxiety 34:928–966
Denis A, Luminet O (2018) Cognitive factors and post-partum depression: what is the influence of general personality traits, rumination, maternal self-esteem, and alexithymia? Clin Psychol Psychother 25:359–369
Kendell RE (2002) The distinction between personality disorder and mental illness. Br J Psychiatry 180(2):110–115
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Petfield L, Startup H, Droscher H, Cartwright-Hatton S (2015) Parenting in mothers with borderline personality disorder and impact on child outcomes. Evid Based Ment Health 18(3):67–75
Eyden J, Winsper C, Wolke D, Broome MR, MacCallum F (2016) A systematic review of the parenting and outcomes experienced by offspring of mothers with borderline personality pathology: potential mechanisms and clinical implications. Clin Psychol Rev 47:85–105
Laulik S, Chou S, Browne KD, Allam J (2013) The link between personality disorder and parenting behaviors: a systematic review. Aggress Violent Beh 18(6):644–655
Crandell LE, Patrick MP, Hobson RP (2003) ‘Still-face’interactions between mothers with borderline personality disorder and their 2-month-old infants. Br J Psychiatry 183(3):239–247
Hobson RP, Patrick M, Crandell L, Garcia-Perez R, Lee A (2005) Personal relatedness and attachment in infants of mothers with borderline personality disorder. Dev Psychopathol 17(2):329–347
Newman LK, Stevenson CS, Bergman LR, Boyce P (2007) Borderline personality disorder, mother–infant interaction and parenting perceptions: preliminary findings. Aust N Z J Psychiatry 41(7):598–605
White H, Flanagan TJ, Martin A, Silvermann D (2011) Mother–infant interactions in women with borderline personality disorder, major depressive disorder, their co-occurrence, and healthy controls. J Reprod Infant Psychol 29(3):223–235
Delavenne A, Gratier M, Devouche E, Apter G (2008) Phrasing and fragmented time in “pathological” mother–infant vocal interaction. Music Sci 12(1_suppl):47–70
Hobson RP, Patrick MPH, Hobson JA, Crandell L, Bronfman E, Lyons-Ruth K (2009) How mothers with borderline personality disorder relate to their year-old infants. Br J Psychiatry 195(4):325–330
Schwarze CE, Hellhammer DH, Stroehle V, Lieb K, Mobascher A (2015) Lack of breastfeeding: a potential risk factor in the multifactorial genesis of borderline personality disorder and impaired maternal bonding. J Pers Disord 29(5):610–626
Elliot RL, Campbell L, Hunter M, Cooper G, Melville J, McCabe K, Newman L, Loughland C (2014) When I look into my baby’s eyes… Infant emotion recognition by mothers with borderline personality disorder. Infant Ment Health J 35(1):21–32
Conroy S, Marks MN, Schacht R, Davies HA, Moran P (2010) The impact of maternal depression and personality disorder on early infant care. Soc Psychiatry Psychiatr Epidemiol 45(3):285–292
Pickles A, Angold A (2003) Natural categories or fundamental dimensions: on carving nature at the joints and the rearticulation of psychopathology. Dev Psychopathol 15(3):529–551
Trull TJ, Durrett CA (2005) Categorical and dimensional models of personality disorder. Annu Rev Clin Psychol 1:355–380
Zimmerman M, Chelminski I, Young D, Dalrymple K, Martinez J (2013) Is dimensional scoring of borderline personality disorder important only for subthreshold levels of severity? J Pers Disord 27(2):244–251
Pearson RM, Campbell A, Howard LM, Bornstein MH, Omahen H, Mars B, Moran P (2018) Impact of dysfunctional maternal personality traits on risk of offspring depression, anxiety and self-harm at age 18 years: a population-based longitudinal study. Psychol Med 48(1):50–60
Huntley F, Wright N, Pickles A, Sharp H, Hill J (2017) Maternal mental health and child problem behaviours: disentangling the role of depression and borderline personality dysfunction. Br J Psychiatry Open 3(6):300–305
Hopwood CJ, Kotov R, Krueger RF, Watson D, Widiger TA, Althoff RR, Ansell EB, Bach B, Michael Bagby R, Blais MA (2018) The time has come for dimensional personality disorder diagnosis. Personal Ment Health 12(1):82–86
Stepp SD, Whalen DJ, Pilkonis PA, Hipwell AE, Levine MD (2012) Children of mothers with borderline personality disorder: identifying parenting behaviors as potential targets for intervention. Personal Disord Theory Res Treat 3(1):76
Lyons-Ruth K (2012) Methodological challenges in identifying parenting behaviors as potential targets for intervention: commentary on Stepp et al. (2011). Personal Disord Theory Res Treat 3(1):95–97
Trevillion K, Domoney J, Pickles A, Bick D, Byford S, Heslin M, Milgrom J, Mycroft R, Pariante CM, Ryan E, Hunter M, Howard LM (2016) Depression: an exploratory parallel-group randomised controlled trial of Antenatal guided self help for WomeN (DAWN): study protocol for a randomised controlled trial. Trials. https://doi.org/10.1186/s13063-016-1632-6
Howard LM, Ryan EG, Trevillion K, Anderson F, Bick D, Bye A, Byford S, O’Connor S, Sands P, Demilew J (2018) Accuracy of the Whooley questions and the Edinburgh Postnatal Depression Scale in identifying depression and other mental disorders in early pregnancy. Br J Psychiatry 212(1):50–56
Aldridge H, Born TB, Tinson A, MacInnes T (2015) London’s poverty profile: 2015. Trust for London/New Policy Institute, London
Moran P, Leese M, Lee T, Walters P, Thornicroft G, Mann A (2003) Standardised Assessment of Personality Abbreviated Scale (SAPAS): preliminary validation of a brief screen for personality disorder. Br J Psychiatry 183:228–232
Zanarini MC, Frankenburg FR, Sickel AE, Yong L (1996) The diagnostic interview for DSM-IV personality disorders (DIPD-IV). McLean Hospital, Belmont, p 340
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150:782–786
Brockington I, Oates J, George S, Turner D, Vostanis P, Sullivan M, Loh C, Murdoch C (2001) A screening questionnaire for mother–infant bonding disorders. Arch Womens Ment Health 3:133–140
Crittenden PM (2006) A dynamic-maturational model of attachment. Aust N Z J Fam Ther 27(2):105–115
Crittenden PM (2010) CARE-Index: infants coding manual. Family Relations Institute, Miami
Leventhal A, Jacobsen T, Miller L, Quintana E (2004) Caregiving attitudes and at-risk maternal behavior among mothers with major mental illness. Psychiatr Serv 55:1431–1433. https://doi.org/10.1176/appi.ps.55.12.1431
Babor F, Higgins-Biddle JC, Saunders JB, Monterio MG (2008) Audit—The Alcohol Use Disorders Identification Test—guidelines for use in primary care, 2nd edn. The World Health Orginisation, Geneva
Cherpitel CJ (1995) Analysis of cut points for screening instruments for alcohol problems in the emergency room. J Stud Alcohol 56:695–700
Berman AH, Bergman H, Palmstierna T, Schylter F (2003) DUDIT—The Drug use disorder identification test. Karolinska Institutet, Department of Clinical Neuroscience, Stockholm
StataCorp (2017) Stata statistical software: release 15. StataCorp LLC, College Station
Borjesson K, Ruppert S, Bagedahl-Strindlund M (2005) A longitudinal study of psychiatric symptoms in primiparous women: relation to personality disorders and sociodemographic factors. Arch Women’s Ment Health 8(4):232–242
Høivik MS, Lydersen S, Ranøyen I, Berg-Nielsen TS (2018) Maternal personality disorder symptoms in primary health care: associations with mother–toddler interactions at one-year follow-up. BMC Psychiatry 18(1):198
Wilson S, Durbin CE (2012) Parental personality disorder symptoms are associated with dysfunctional parent-child interactions during early childhood: a multilevel modeling analysis. Personal Disord Theory Res Treat 3(1):55
Svanberg P, Mennet L, Spieker S (2010) Promoting a secure attachment: a primary prevention practice model. Clin Child Psychol Psychiatry 15(3):363–378
Foley S, Hughes C (2018) Great expectations? Do mothers’ and fathers’ prenatal thoughts and feelings about the infant predict parent-infant interaction quality? A meta-analytic review. Dev Rev 48:40–54
Howard LM, Oram S, Galley H, Trevillion K, Feder G (2013) Domestic violence and perinatal mental disorders: a systematic review and meta-analysis. PLoS Med 10(5):e1001452
Kildare CA, Middlemiss W (2017) Impact of parents mobile device use on parent-child interaction: a literature review. Comput Hum Behav 75:579–593
Kushlev K, Dunn EW (2018) Smartphones distract parents from cultivating feelings of connection when spending time with their children. J Soc Pers Relatsh. https://doi.org/10.1177/0265407518769387
Kenny M, Conroy S, Pariante CM, Seneviratne G, Pawlby S (2013) Mother–infant interaction in mother and baby unit patients: before and after treatment. J Psychiatr Res 47(9):1192–1198
Fok MLY, Seegobin S, Frissa S, Hatch SL, Hotopf M, Hayes RD, Moran P (2015) Validation of the standardised assessment of personality–abbreviated scale in a general population sample. Personal Ment Health 9(4):250–257
Ball L, Tully RJ, Egan V (2017) The SAPAS, personality traits, and personality disorder. J Pers Disord 31(3):385–398
Crowley G, Molyneaux E, Nath S, Trevillion K, Moran P, Howard LM (2019) Disordered personality traits and psychiatric morbidity in pregnancy: a population-based study. Arch Womens Ment Health. https://doi.org/10.1007/s00737-018-0937-8
Kim Y-R, Tyrer P (2010) Controversies surrounding classification of personality disorder. Psychiatry Investig 7(1):1
Watts J (2019) Problems with the ICD-11 classification of personality disorder. Lancet Psychiatry 6(6):461–463
Tyrer P, Crawford M, Mulder R, The ICD-11 Working Group for the Revision of Classification of Personality Disorders (2011) Reclassifying personality disorders. Lancet 377(9780):1814–1815
Tsivos Z-L, Calam R, Sanders M, Wittkowski A (2015) Interventions for postnatal depression assessing the mother–infant relationship and child developmental outcomes: a systematic review. Int J Women’s Health 7:429
Wilson R, Weaver T, Michelson D, Day C (2018) Experiences of parenting and clinical intervention for mothers affected by personality disorder: a pilot qualitative study combining parent and clinician perspectives. BMC Psychiatry 18(1):152
Stein A, Netsi E, Lawrence PJ, Granger C, Kempton C, Craske MG, Nickless A, Mollison J, Stewart DA, Rapa E (2018) Mitigating the effect of persistent postnatal depression on child outcomes through an intervention to treat depression and improve parenting: a randomised controlled trial. Lancet Psychiatry 5(2):134–144
Acknowledgements
We are extremely grateful to the mothers and babies that took part in our study. We also thank our service user advisory group for all their help and advice.
Funding
The baseline data collection was funded by the National Institute for Health Research (NIHR) under the Programme Grants for Applied Research programme (ESMI Programme: Grant Reference No. RP-PG-1210-12002) and the National Institute for Health Research (NIHR)/Wellcome Trust King’s Clinical Research Facility and the NIHR Biomedical Research Centre and Dementia Unit at South London and Maudsley NHS Foundation Trust and King’s College London. The Nuffield Foundation (Grant Reference No. KID/42599) funded the 3 months’ postpartum follow-up home visits for the data collection of observational mother–infant interactions. LMH also has salary support from an NIHR Research Professorship (NIHR-RP-R3-12-011). The study team acknowledges the study delivery support given by the South London Clinical Research Network. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health or Nuffield foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PM led the original development of The Standardised Assessment of Personality Abbreviated Scale (SAPAS). There are no other conflicts of interest to report.
Ethical standards
Ethical approval for the study was obtained by the National Research Ethics Service, London Committee—Camberwell St Giles (Ref No. 14/LO/0075). Women were provided with participant information sheets, had the study explained to them by a researcher and had the opportunity to ask questions prior to providing informed consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nath, S., Pearson, R.M., Moran, P. et al. Maternal personality traits, antenatal depressive symptoms and the postpartum mother–infant relationship: a prospective observational study. Soc Psychiatry Psychiatr Epidemiol 55, 621–634 (2020). https://doi.org/10.1007/s00127-019-01790-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01790-y