Abstract
Aims/hypothesis
High-throughput metabolomics technologies in a variety of study designs have demonstrated a consistent metabolomic signature of overweight and type 2 diabetes. However, the extent to which these metabolomic patterns can be reversed with weight loss and diabetes remission has been weakly investigated. We aimed to characterise the metabolomic consequences of a weight-loss intervention in individuals with type 2 diabetes.
Methods
We analysed 574 fasted serum samples collected within an existing RCT (the Diabetes Remission Clinical Trial [DiRECT]) (N=298). In the trial, participating primary care practices were randomly assigned (1:1) to provide either a weight management programme (intervention) or best-practice care by guidelines (control) treatment to individuals with type 2 diabetes. Here, metabolomics analysis was performed on samples collected at baseline and 12 months using both untargeted MS and targeted 1H-NMR spectroscopy. Multivariable regression models were fitted to evaluate the effect of the intervention on metabolite levels.
Results
Decreases in branched-chain amino acids, sugars and LDL triglycerides, and increases in sphingolipids, plasmalogens and metabolites related to fatty acid metabolism were associated with the intervention (Holm-corrected p<0.05). In individuals who lost more than 9 kg between baseline and 12 months, those who achieved diabetes remission saw greater reductions in glucose, fructose and mannose, compared with those who did not achieve remission.
Conclusions/interpretation
We have characterised the metabolomic effects of an integrated weight management programme previously shown to deliver weight loss and diabetes remission. A large proportion of the metabolome appears to be modifiable. Patterns of change were largely and strikingly opposite to perturbances previously documented with the development of type 2 diabetes.
Data availability
The data used for analysis are available on a research data repository (https://researchdata.gla.ac.uk/) with access given to researchers subject to appropriate data sharing agreements. Metabolite data preparation, data pre-processing, statistical analyses and figure generation were performed in R Studio v.1.0.143 using R v.4.0.2. The R code for this study has been made publicly available on GitHub at: https://github.com/lauracorbin/metabolomics_of_direct.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
For conditions like type 2 diabetes where there is a clear relationship between risk factors, intermediate metabolic phenotypes and disease, attention has turned to metabolomics as a potentially useful tool for elucidating the biological mechanisms underpinning disease pathology [1, 2]. Studies to date have demonstrated a strong and consistent metabolomic signature of prevalent type 2 diabetes [3] and incident disease [4, 5]. Unsurprisingly, given the strong overlap in the metabolomic signature of type 2 diabetes and its precursors (overweight/obesity and insulin resistance) [6, 7], many of the metabolomic perturbations observed in individuals diagnosed with disease also appear to have a role in disease development [8, 9]. However, it remains to be determined whether the changes observed reflect a systemic ‘downstream’ response to high glucose per se or else ‘upstream’ excess adiposity [10, 11].
To help elucidate the role of metabolites in type 2 diabetes, studies that evaluate the metabolomic response to disease remission following interventions are critical. Weight loss is a key intervention for individuals with type 2 diabetes, with proven efficacy and evidence of sustainability of the metabolic benefits for up to 10 years [12, 13]. While there have been metabolomics studies of weight loss, the reliability and robustness of results published to date have been questioned (e.g. due to small sample sizes and single-arm designs) [14]. There remains a need to characterise the molecular underpinnings of existing interventions targeting diabetes remission through weight loss. Accordingly, we took samples from a seminal RCT involving an intensive weight management programme, the Diabetes Remission Clinical Trial (DiRECT), with the aim of characterising the metabolomic footprint of this intervention.
Methods
Study design and participants
DiRECT was a 2 year open-label, cluster RCT conducted at 49 primary care practices in Scotland and the Tyneside region of England between 25 July 2014 and 5 August 2016 (isrctn.org registration no. ISRCTN03267836). The trial was carried out to assess whether effective weight management, delivered in a primary care setting, could produce sustained remission of type 2 diabetes. The protocol has been published elsewhere [15], as have the baseline characteristics of the groups [16]. In brief, general practices were randomly assigned (1:1) to provide either a weight management programme (intervention) or best-practice care by guidelines (control), with stratification for study site (Tyneside or Scotland) and practice list size (>5700 or ≤5700). Individuals aged 20–65 years who had been diagnosed with type 2 diabetes within the past 6 years, had a BMI of 27–45 kg/m2 and were not receiving insulin were recruited. The intervention (Counterweight-Plus, https://www.counterweight.org/) comprised withdrawal of glucose-lowering and antihypertensive drugs, total diet replacement (3452–3569 kJ [825–853 kcal]/day formula diet for 3–5 months), stepped food reintroduction (2–8 weeks) and structured support for long-term weight-loss maintenance. Ethics approval was granted by West 3 Ethics Committee in January 2014, with approvals by the National Health Service (NHS) health board areas in Scotland and clinical commissioning groups in Tyneside. All participants provided written informed consent.
The trial was conducted over a period of 2 years with principal data collection points scheduled at baseline, 12 months and 2 years. Blood samples were collected and a range of clinically relevant outcomes measured, including liver function tests, cholesterol and triglycerides (TGs) [15]. In this study, we analysed samples from the baseline and 12 month time points using both an untargeted MS approach (Metabolon, Durham, NC, USA) and 1H-NMR spectroscopy (Nightingale Health, Finland). For all other data used in our analyses, we used the same version of the trial database as used for the main trial analysis at 12 months, as reported by Lean et al [17]. These data comprised an intention-to-treat population of 149 participants per group (total N=298).
Sample collection and metabolite data acquisition
Participants were asked to fast overnight before the blood draw. Sample handling procedures are described in electronic supplementary material (ESM) Methods. In total, 574 serum samples collected from 302 unique individuals during the trial were sent for metabolomic analysis. All analysts were blinded to intervention/control status. Samples were sent first to Metabolon. The dataset returned (‘MS data’) included 1276 metabolite features comprising 959 compounds of known identity (named biochemicals with the majority matched to purified standards) and 317 compounds of unknown structural identity (unnamed biochemicals, indicated by a superscript ‘a’ in the main-text tables). Remaining sample material was then sent to the MRC Integrative Epidemiology Unit Metabolomics Facility (University of Bristol) for 1H-NMR analyses (after one further freeze–thaw). The dataset returned (‘NMR data’) included 148 primary measures quantified in absolute concentrations as well as 79 additional ‘derived measures’ such as ratios and percentages. Further details of the metabolite data acquisition can be found in ESM Methods.
Metabolite data preparation
Data quality checks were carried out locally using a pre-release version of the R package metaboprep [18] with samples and features excluded from subsequent statistical analysis based on a pre-defined set of quality control (QC) metrics. Full details of the procedures are given in ESM Methods and data summaries produced are included within the associated GitHub repository (https://github.com/lauracorbin/metabolomics_of_direct). Data were restricted to include only those individuals present in the trial database (N=298) and for whom both a baseline (T0) and 12 month follow-up (T1) sample were present in the filtered metabolite data. Two processed datasets were derived: (1) RNT dataset, for which metabolite data were transformed (across individuals within timepoint) using a rank-based inverse normal transformation (where tied ranks were split by assigning a random order); and (2) PA dataset, for which metabolite data were transformed to a presence/absence phenotype such that missing values were replaced with 0 and non-missing values (i.e. those with an abundance measure) were replaced with 1.
Statistical analysis
An overview is shown in Fig. 1. We analysed all available data according to group allocation with the control group as the reference and effect estimates therefore representing the difference in the intervention group relative to the control group.
Linear regression model
In our evaluation of the effect of the intervention on metabolite levels, outcomes (metabolite levels at T1) were compared between groups with linear regression models applied to the RNT dataset. Where metaboliteT0 or metaboliteT1 was missing (unquantified) for an individual, that individual was excluded from the analysis for that specific metabolite yielding varied sample sizes across metabolites. Models were adjusted for study centre and practice list size along with the baseline measurement of the outcome (metabolite at T0), age and sex, all fitted as fixed effects:
where metaboliteT1 is metabolite level at 12 months, ‘study centre’ is a binary variable (Tyneside or Scotland), ‘list size’ is a binary variable indicating practice list size (>5700 or ≤5700), age is participant age at baseline (years), sex is a binary variable (male/female), metaboliteT0 is metabolite level at baseline and allocation is a binary exposure variable indicating the individual’s treatment group (control or intervention). Model β represents the expected difference in metabolite level at T1 expressed as normalised SD units per unit difference in the dependent variable after adjusting for metabolite level at T0 (in the case of allocation this is the mean difference between groups in metabolite at T1). Results from this analysis were considered to be the primary result for all metabolite features with <40% missing (unquantified) data at the 12 month timepoint. This missingness threshold was selected based on the increase in the SE of the treatment group effect estimated from the linear model when the number of observations fell below this level (see ESM Fig. 1). The Holm [19] method was used to adjust p values for multiple testing and an adjusted p value of <0.05 was considered as evidence for association. Extended methods relating to the linear regression model can be found in ESM Methods.
Pathway enrichment analyses
Hypergeometric-based enrichment analyses were conducted to evaluate the enrichment of classes in the subset of associated features derived from the linear model as compared with all features that were tested by the same model. Metabolite super-pathway designation provided by Metabolon was used for the enrichment analysis, with NMR-derived metabolites allocated to super pathways following the approach of Wahl et al [20].
Exploratory analysis of associated metabolites and clinical phenotypes
Where metabolites were found to be associated with the intervention, several follow-up analyses were performed (see ESM Methods for full details). To evaluate the extent to which the association between metaboliteT1 and allocation could alternatively be explained by weight change, the primary model above was re-fitted with the addition of ‘weight change’ as a fixed effect. To begin to understand the potential relevance of metabolite levels to diabetes remission, over and above their role as proxies for weight loss, metabolite change was compared in individuals who did and did not achieve diabetes remission within quantiles of weight change. Finally, a principal component analysis (PCA)-based investigation was conducted into the relationship between the metabolites found to be associated with the intervention and the change in a subset of clinical phenotypes selected based on their relevance to the long-term health of individuals with type 2 diabetes.
Comparison of intervention and incident type 2 diabetes footprints
To assess the extent to which the changes we see here in response to the DiRECT intervention are equal and opposite to those observed prior to development of type 2 diabetes, we extracted summary relative risk (SRR) estimates from a recent meta-analysis of prospective cohort studies [5]. Metabolites were matched as far as possible against those with meta-analysis results (presented in Supplementary Table 7 of Morze et al [5]) using either Human Metabolome Database (HMDB) identifiers or biochemical names. Where the metabolite was measured by both platforms, the instance with the smallest p value was retained. Intervention effects (β extracted from the linear model) were plotted against loge SRRs extracted from the meta-analysis. We focused the comparison on those metabolites where there was evidence of association with the intervention based on an unadjusted p value threshold of >0.05. Analysis with all matched metabolites is also made available.
Logistic regression model
A logistic model was applied to the PA datasets to compare the presence of each metabolite by allocation as follows:
where metaboliteT1 is metabolite presence at 12 months (1, present; 0, absent) and metaboliteT0 is metabolite presence at baseline (1, present; 0, absent) and allocation is as defined above. In this exploratory model, no covariates were fitted to maximise the power of the test. Model βs for the exposure, ‘allocation’, represent the coefficient for intervention group, that is the loge OR between intervention group and control group. Results from this analysis, in which we assume missing data are due to very low levels of the metabolite (below that which can be detected) or to complete absence of the metabolite, were considered the primary result for all features with ≥40% missing (unquantified) data. A p value of <0.05 was considered as evidence for association with no adjustment made for multiple testing.
Results
Study characteristics
At 12 months, mean body weight had fallen by 10 kg in the intervention group and by 1 kg in the control group (adjusted difference –8.8 [95% CI –10.3, –7.3] kg, p<0.0001) and almost half of the 149 participants in the trial arm (46%) had achieved type 2 diabetes remission (as defined in the trial protocol) as compared with six participants (4%) in the control arm [17]. Baseline characteristics were similar when comparing the intervention group with the control group in the subset of participants with metabolomics data (Table 1). Following in-house QC, the NMR data comprised 567 samples and 225 metabolic features (147 primary measures and 78 derived measures) and the MS data comprised 571 samples and 1254 metabolites (ESM Table 1). After merging with trial data there were 258 individuals in the NMR dataset (115 intervention and 143 control) and 261 individuals in the MS dataset (117 intervention and 144 control) available for statistical analysis.
Effect of intervention on metabolites: linear regression model
Results from the multivariable linear model formed the primary result for all 147 NMR metabolites and 78 NMR-derived measures with a minimum (median) sample size of 199 (258). Of the NMR metabolites tested at 12 months, 59 (26%) were altered by the intervention (Holm-corrected p<0.05) (including 27 derived measures) with 41 (69% of those altered) showing an increase in response to treatment (ESM Fig. 2, ESM Table 2). The strongest association was seen for glucose (β −0.71 [95% CI −0.92, −0.50], Holm-corrected p=3.77×10−8). Results from the linear model formed the primary result for 1064 (85%) of the MS metabolites, with a minimum (median) sample size of 93 (260). Of the metabolites tested, 127 (12%) were associated with the intervention (Holm-corrected p<0.05) with 72 (57% of those associated) showing an increase in response to treatment (ESM Fig. 2, ESM Table 3). The strongest association was seen for a metabolite identified as erythronate (β −0.82 [95% CI −0.99, −0.65], Holm-corrected p=2.84×10−15), although the identity of this metabolite has not yet been confirmed by Metabolon based on a standard. For most metabolites, there was little evidence for between-group (control/intervention) differences in levels at baseline; one out of 186 associated metabolites (4-hydroxychlorothalonil) had p<0.05/186 (Wilcoxon rank sum test) (for boxplots, see GitHub repository: https://github.com/lauracorbin/metabolomics_of_direct).
In the intervention group, we observed a decrease in phosphatidylethanolamines, branched-chain amino acids (BCAAs) and related metabolites (i.e. those allocated to the same super- and sub-pathways) and sugars, and in the relative abundance of TG to total lipids within specific lipid fractions (e.g. TG/total lipids ratio in small, medium and large LDL particles). In contrast, increases were seen in lipids including sphingolipids, plasmalogens and metabolites assigned to the ‘fatty acid metabolism (acyl choline)’ sub-pathway and for amino acids from the sub-pathways ‘glycine, serine and threonine metabolism’ and ‘urea cycle; arginine and proline metabolism’. There was also evidence (from NMR) for an increase in the intervention group of the proportion of cholesterol and cholesteryl esters relative to total lipids in a variety of lipid fractions and an increase in the ratio of polyunsaturated fatty acids to total fatty acids.
Pathway enrichment analyses
Enrichment analyses gave evidence for enrichment in the associated metabolites for NMR-derived measures (2.4-fold, p=5.08×10−6) and for the carbohydrate super pathway (2.4-fold, p=0.011) (ESM Fig. 3). This suggests that metabolites allocated to these groups were overrepresented in the list of associated metabolites.
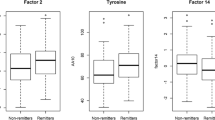
Exploratory analysis of associated metabolites and clinical phenotypes
For the vast majority of metabolites examined, when weight change was added as a fixed effect to the primary linear model, the intervention effect on metabolite level at 12 months was attenuated, as demonstrated by a qualitative reduction in the variance explained by allocation (ESM Tables 2, 3). In a small number of cases (seven for NMR and one for MS), adjusting for weight change did not result in the attenuation of the intervention effect (e.g. ‘omega-3 fatty acids’ [n-3 fatty acids] [NMR] and sphingomyelin [d17:1/14:0, d16:1/15:0]a [MS], where the superscript ‘a’ indicates that the compound has not been confirmed based on a standard). For some metabolites, there was evidence for metabolite change explaining additional variance in remission status beyond that explained by weight change (ESM Table 4). For example, a difference in mean metabolite change by remission status was seen within individuals in the first quantile of weight change (−31.6 kg to −9.0 kg) for 1,5-anhydroglucitol (p=8.52×10–5), MS-measured glucose (p=4.64×10–5) and other sugars (ESM Fig. 4). Although some of this difference may be attributable to residual variance in weight change (within quantiles), at least in the case of the aforementioned metabolites, the association of metabolite change with remission status remained after adjustment for weight change when fitted in a linear regression model (data not shown).
Prior to PCA, a hierarchical clustering approach allocated the 1289 metabolites with <40% missing data to 238 metabolite clusters (ESM Table 5). Using these clusters, the full list of 186 associated metabolites was reduced to a set of 61 approximately independent, representative features for use in the PCA, of which 51 had at least a putative identification (Table 2 and ESM Table 6). The PCA analysis (ESM Fig. 5 for resultant scree plot) exhibited separation of participants on principal component 1 (PC1; which explained 21% of the variance) according to both their allocation to intervention or control arms of the trial and their remission status at 12 months; this pattern is illustrated in Fig. 2. There was also evidence for a correlation between the metabolomic footprint of the intervention (as captured by the PCs) and clinical indicators of metabolic health (e.g. HbA1c), as well as several phenotypes relevant to non-alcoholic fatty liver disease (ESM Results, ESM Table 7 and ESM Figs 6A, B, 7).
Clustering to show treatment group allocation and type 2 diabetes remission status. Heatmap shows metabolite levels at 12 months derived from covariate-adjusted RNT data for the 61 intervention-associated representative metabolites. Further description of plot generation can be found in ESM Methods. ‘Remission status’ indicates participant’s type 2 diabetes status at 12 months, such that white indicates no remission and black indicates remission. In the case of ‘treatment group’ allocation, blue indicates control and orange indicates intervention group
Comparison of intervention and incident type 2 diabetes footprints
Of 622 unique metabolites with (unadjusted) p<0.05 in the primary analysis, 79 were matched to entries in the meta-analysis results [5], including 13 that passed the threshold for association in the primary analysis (Holm-corrected p<0.05). In this subset of intervention-associated metabolites, the correlation between the intervention effect βs and the loge SRR of incident type 2 diabetes extracted from the meta-analysis was −0.70 (95% CI −0.80, −0.57, p=6.0×10−13) (Fig. 3. When comparing estimates across all 143 matched metabolites, the correlation was −0.61 (95% CI −0.71, −0.50, p=4.9×10−16)(ESM Fig. 8, ESM Table 8).
Comparison of intervention and incident type 2 diabetes footprints. Loge SRR estimates extracted from incident type 2 diabetes meta-analysis [5] plotted against mean intervention effects (βs) from our linear regression models (these βs represent the mean difference in metabolite levels at 12 months in the intervention group relative to the control group). Each point represents a metabolite that was associated with intervention in the primary analysis (unadjusted p<0.05) and could be matched to meta-analysis results; metabolites with Holm-corrected p<0.05 in the primary analysis are labelled. Points are coloured according to the SRR-associated p value in the meta-analysis. The correlation is −0.70 (95% CI −0.80, −0.57, p=6.0×10−13). See ESM Fig. 8 for results including all matched metabolites
Effect of intervention on metabolites: logistic regression model
Data from the logistic model (based on the PA dataset and able to detect and describe the presence of xenobiotics) formed the primary result for 190 of the MS metabolites, most of which were classified as xenobiotics or unidentified molecules (Table 3 and ESM Table 9). Of these, 19 (12 identified) were associated with the intervention (p<0.05), with 11 (8 identified) showing depletion in the intervention group. Metformin showed the strongest association and was present in 26% (31/117) of the 12 month samples from those in the intervention group compared with 78% (112/144) in the control group (see also ESM Results).
Discussion
We observed a broad metabolomic signature associated with the intervention, with differences observed in metabolites from every one of the biochemical classes (or super pathways) represented. Under a conservative correction for multiple testing, 26% of NMR-derived metabolites and 12% of MS-derived metabolites were altered by the intervention, suggesting that a sizeable proportion of metabolite changes in type 2 diabetes are modifiable. We report a lipid pattern change with reduction in TG-rich lipoproteins across the lipoprotein cascade, but enrichment of (lyso)plasmalogens and reversal of amino acid changes associated with type 2 diabetes, as well as a reduction in a range of sugars beyond glucose, including fructose and mannose.
A major strength of this study is the use of samples and clinical data collected from a relatively large (compared with existing literature) cluster randomised trial with a well-matched control arm. Measuring metabolites both at baseline and at 12 months added to the robustness of the analysis while the use of two complementary metabolomics platforms increased the overall coverage of the metabolome beyond that which has been evaluated previously. However, the MS data are semi-quantitative meaning that these findings require further validation using targeted techniques to allow absolute quantification. Twelve-month samples were not available from participants who dropped out of the trial; this was only a small number and since the primary analyses concerned paired baseline and 12 month measures, bias from this differential missingness was minimised. While our study design enabled us to conduct a thorough evaluation of the metabolomic impact of the Counterweight-Plus intervention overall, it is challenging to attribute those changes to specific elements of the intervention (e.g. to fat loss per se or ‘upstream’ changes in diet). Results from attempts here to extract the weight-loss effects should be interpreted with caution, especially given that these analytical manoeuvres alter the trial structure and, as such, have the potential to introduce bias.
Characteristic changes in metabolite profile
Many of the metabolites influenced by the intervention have also been identified as potential risk factors for type 2 diabetes development with opposite and proportionate effect sizes. For example, we see decreased concentrations of BCAAs following dietary intervention where plasma concentrations of these BCAAs are frequently elevated in type 2 diabetes [5, 9, 21]. The decrease we observe in BCAAs largely agrees with existing findings from smaller, targeted studies of weight-loss interventions [14, 22, 23]. While not all studies report this decrease in BCAAs after diet-induced weight loss [24], this may be due to a lack of power to discern what is likely to be a smaller effect than that from equivalent analyses considering surgical interventions. By using an untargeted metabolome-wide approach, in this work we were able to further characterise the plasticity of this highly relevant network. We observed concurrent decreases in several γ-glutamyl BCAA dipeptides allocated to the same cluster as the BCAAs themselves; γ-glutamyl amino acids are produced when the enzyme, γ-glutamyl transpeptidase, present mainly in the liver, catalyses the transfer of the γ-glutamyl moiety of glutathione to an amino acid [25].
Similarly to BCAAs, the reduction we see in the levels of several simple sugars, including the monosaccharides fructose, glucose and mannose, are opposite to the elevations seen in levels of these metabolites in the presence of obesity. While structurally similar, the predominant dietary sources, metabolic pathways and biological effects of these simple sugars are quite different though interdependent [26]. Mannose specifically has been associated not only with insulin resistance but also with higher risk of several chronic diseases including type 2 diabetes and CVD [27]. The existing literature concerning the most strongly associated metabolite from the MS dataset, erythronate, is limited; however, further insight into its relevance to type 2 diabetes can be gained by considering its relationship with other measured metabolites. In our data, erythronate sits in a cluster with (i.e. is correlated with) several common sugar alcohols (ribitol, erythritol, arabitol/xylitol) that can be found naturally in fruits but that are also commonly used as artificial sweeteners. Erythritol is predominantly excreted in urine, with the remaining 5–10% being oxidised to erythronate [28]. While designated as a xenobiotic in the Metabolon data and previously thought not to be produced endogenously [29], erythritol may in fact be produced endogenously from glucose [30]. This, together with preliminary evidence showing an association between erythritol and adiposity gain in young adults [30], serves to contextualise our findings of reduced levels of erythronate and related metabolites (ribitol, orotidine and erythritol all had p<0.05 before Holm-correction) in participants in the intervention group.
Participants in the intervention arm saw increases in several lipids previously associated with a favourable metabolic profile. Specifically, increases were seen in concentrations of several (lyso)plasmalogens, a special class of phospholipids characterised by the presence of a vinyl–ether bond at the sn-1 position. In a cross-sectional study of participants with overweight and obesity, plasmalogen levels were found to be inversely correlated with body fat percentage but seemingly not related to BMI or WHR [31]. The lack of association for these commonly used indicators of adiposity may be related to their suboptimal performance as proxies for adiposity in this relatively small sample of individuals all with BMI>25 kg/m2 (n=65). Alternatively, this may point towards a more complex interplay between metabolic health and plasmalogens.
Detecting associations with changes in exogenous factors
While changes to the metabolism can be expected in response to the intervention-induced weight loss experienced by many of those in the intervention group, we also expect the adoption of new dietary patterns and a change in medication regimes. At a metabolomic level, and notwithstanding possible limitations linked to limits of detection, we assume that, where we see high levels of missingness for given metabolites, these patterns are indicative of absence and/or very low concentration. This does mean that naive application of a linear model will be underpowered to detect mean differences in concentrations. However, examining between-group differences in presence/absence can allow detection of meaningful relationships. To this end, the logistic regression analysis here revealed between-group differences in the frequency of detection of both potential dietary biomarkers and medications. For example, S-allylcysteine, a proposed biomarker for garlic consumption [32], was enriched in the intervention group while ethyl glucuronide, a validated urine biomarker for alcohol consumption [33, 34] was depleted. The reduced presence of metformin in the intervention group at 12 months provides a useful positive control as well as offering an opportunity to verify medication usage. In the linear regression analysis, the association of omega-3 (n-3) fatty acids with allocation did not attenuate with additional adjustment for weight change. This suggests that the increased levels of these essential fats in participants from the intervention arm are due to dietary changes (sustained at 12 months) and are not directly related to weight loss.
Metabolite profile variation and clinically relevant biomarkers
Metabolic profile at 12 months, as captured by the intervention-associated metabolites, was strongly correlated with weight change, possibly explaining much of the allocation effect that we observe. Indeed, the changes we see in levels of glucose and BCAAs are characteristic of those seen with weight change in other settings [20, 35, 36]. We see a decrease in the TG/total lipids ratio across LDLs and VLDLs in participants in the intervention group, with what appears to be a corresponding increase in the total cholesterol and/or cholesteryl ester/total lipids ratio in a similar subset of lipoproteins as would be expected given the previously characterised decrease in hepatic production of VLDL TG following dietary weight loss in type 2 diabetes [37]. These effects are in keeping with the proposed mechanism by which excess TG in the circulation triggers the transfer of TGs from the core of TG-rich lipoproteins to LDL in exchange for cholesteryl esters by the cholesteryl ester transfer protein [38].
The metabolic profile at 12 months was also correlated with change in HbA1c, demonstrating the ability of the intervention-associated metabolites identified to capture changes in glycaemic health as expressed by traditional clinical biomarkers. However, we also found evidence of subtle differences in the metabolome of those who achieved type 2 diabetes remission as compared with those that did not despite similar levels of weight loss. For example, among those individuals who lost the most weight (greater than 9.0 kg) during the trial, those who also achieved diabetes remission showed greater decreases in glucose, fructose and mannose, as compared with those who did not achieve remission. To some extent, this likely reflects the diagnostic criteria on which remission status was based; indeed, 1,5-anhydroglucitol (a proposed marker of short-term glycaemic control [39]) also appears in the list of metabolites that showed differential change by remission status. Based on the current analysis, we are unable to determine whether these differences reflect metabolic processes that contribute to remission or are simply a reflection of an individual’s current metabolic health status. Meanwhile, the correlations observed between intervention-associated changes in metabolites and clinical indicators of liver health suggest that by conducting an in-depth analysis of metabolites in the presence of sustained improvements to liver health, as here, we can further investigate proposed biological systems, such as the twin cycle hypothesis [40], including in the context of variable individual response (see ESM Discussion).
Conclusion
In conclusion, we have characterised the impact of weight loss in type 2 diabetes at the level of the metabolome. The changes we observed were evident many weeks after the conclusion of the weight-loss phase of the intervention, indicating sustained benefits to health. Our results suggest that previously described perturbations of metabolite profile in incident type 2 diabetes are reversible with intentional weight loss while there is little evidence for any obvious adverse metabolic signals. The extent to which an individual’s metabolic profile is normalised relative to the level seen in healthy control individuals requires further research. Of the clinical variables tested, weight change was most strongly correlated with the overall change in metabolic profile associated with the intervention. This suggests that weight change is upstream of many disease-associated metabolite alterations, in line with growing consensus of the importance of excess adiposity in the pathogenesis of diabetes and, as a treatment target, as reflected in recent ADA/EASD recommendations [41]. Use of data from an RCT of a clinically proven dietary intervention now adopted by the NHS for patients with type 2 diabetes makes these results both generalisable to the patient population and highly clinically relevant. Validation of our findings in larger studies and, in the case of MS data, the use of methods that allow absolute quantification is warranted. This work provides an opportunity for detailed comparisons of different weight-loss interventions (beyond weight and basic measures) in the future, including consideration of the multiple newly emerging pharmacological therapies.
Abbreviations
- BCAA:
-
Branched-chain amino acid
- DiRECT:
-
Diabetes Remission Clinical Trial
- NHS:
-
National Health Service
- PA:
-
Dataset with data transformed to a presence/absence phenotype with missing values replaced with 0 and non-missing values with 1
- PC:
-
Principal component
- PCA:
-
Principal component analysis
- QC:
-
Quality control
- RNT:
-
Dataset with data transformed using a rank-based inverse normal transformation
- SRR:
-
Summary relative risk
- TG:
-
Triglyceride
References
Jin Q, Ma RCW (2021) Metabolomics in diabetes and diabetic complications: insights from epidemiological studies. Cells 10(11):2832. https://doi.org/10.3390/CELLS10112832
Clish CB (2015) Metabolomics: an emerging but powerful tool for precision medicine. Molecular Case Studies 1(1):a000588. https://doi.org/10.1101/mcs.a000588
Arneth B, Arneth R, Shams M (2019) Metabolomics of type 1 and type 2 diabetes. Int J Mol Sci 20(10):2467. https://doi.org/10.3390/ijms20102467
Roberts LD, Koulman A, Griffin JL (2014) Towards metabolic biomarkers of insulin resistance and type 2 diabetes: progress from the metabolome. Lancet Diabetes Endocrinol 2(1):65–75. https://doi.org/10.1016/S2213-8587(13)70143-8
Morze J, Wittenbecher C, Schwingshackl L et al (2022) Metabolomics and type 2 diabetes risk: an updated systematic review and meta-analysis of prospective cohort studies. Diabetes Care 45(4):1013–1024. https://doi.org/10.2337/DC21-1705
Cirulli ET, Guo L, Leon Swisher C et al (2019) Profound perturbation of the metabolome in obesity is associated with health risk. Cell Metab 29(2):488-500 e2. https://doi.org/10.1016/j.cmet.2018.09.022
Abu Bakar MH, Sarmidi MR, Cheng K-K et al (2015) Metabolomics – the complementary field in systems biology: a review on obesity and type 2 diabetes. Mol Biosyst 11(7):1742–1774. https://doi.org/10.1039/C5MB00158G
Guasch-Ferré M, Hruby A, Toledo E et al (2016) Metabolomics in prediabetes and diabetes: a systematic review and meta-analysis. Diabetes Care 39(5):833–846. https://doi.org/10.2337/dc15-2251
Bell JA, Bull CJ, Gunter MJ et al (2020) Early metabolic features of genetic liability to type 2 diabetes: cohort study with repeated metabolomics across early life. Diabetes Care 43(7):1537–1545. https://doi.org/10.2337/dc19-2348
Liu J, Semiz S, van der Lee SJ et al (2017) Metabolomics based markers predict type 2 diabetes in a 14-year follow-up study. Metabolomics 13(9):104. https://doi.org/10.1007/s11306-017-1239-2
Murphy R, Tsai P, Jüllig M, Liu A, Plank L, Booth M (2017) Differential changes in gut microbiota after gastric bypass and sleeve gastrectomy bariatric surgery vary according to diabetes remission. Obes Surg 27:917–925. https://doi.org/10.1007/s11695-016-2399-2
Xin Y, Davies A, Briggs A et al (2020) Type 2 diabetes remission: 2 year within-trial and lifetime-horizon cost-effectiveness of the Diabetes Remission Clinical Trial (DiRECT)/Counterweight-Plus weight management programme. Diabetologia 63(10):2112–2122. https://doi.org/10.1007/S00125-020-05224-2
Mingrone G, Panunzi S, De Gaetano A et al (2021) Metabolic surgery versus conventional medical therapy in patients with type 2 diabetes: 10-year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 397(10271):293–304. https://doi.org/10.1016/S0140-6736(20)32649-0
Tulipani S, Griffin J, Palau-Rodriguez M et al (2016) Metabolomics-guided insights on bariatric surgery versus behavioral interventions for weight loss. Obesity 24(12):2451–2466. https://doi.org/10.1002/oby.21686
Leslie WS, Ford I, Sattar N et al (2016) The Diabetes Remission Clinical Trial (DiRECT): protocol for a cluster randomised trial. BMC Fam Pract 17(1):20. https://doi.org/10.1186/s12875-016-0406-2
Taylor R, Leslie WS, Barnes AC et al (2018) Clinical and metabolic features of the randomised controlled Diabetes Remission Clinical Trial (DiRECT) cohort. Diabetologia 61(3):589–598. https://doi.org/10.1007/s00125-017-4503-0
Lean ME, Leslie WS, Barnes AC et al (2018) Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391(10120):541–551. https://doi.org/10.1016/S0140-6736(17)33102-1
Hughes DA, Taylor K, McBride N et al (2022) metaboprep: an R package for preanalysis data description and processing. Bioinformatics 38(7):1980–1987. https://doi.org/10.1093/BIOINFORMATICS/BTAC059
Holm S (1979) A simple sequentially rejective multiple test procedure. Scand J Stat 6(2):65–70
Wahl S, Vogt S, Stückler F et al (2015) Multi-omic signature of body weight change: results from a population-based cohort study. BMC Med 13(1):48. https://doi.org/10.1186/s12916-015-0282-y
Suhre K, Meisinger C, Döring A et al (2010) Metabolic footprint of diabetes: a multiplatform metabolomics study in an epidemiological setting. PLoS One 5(11):e13953. https://doi.org/10.1371/journal.pone.0013953
Laferrère B, Reilly D, Arias S et al (2011) Differential metabolic impact of gastric bypass surgery versus dietary intervention in obese diabetic subjects despite identical weight loss. Sci Transl Med 3(80):80–82. https://doi.org/10.1126/scitranslmed.3002043
Shah SH, Crosslin DR, Haynes CS et al (2012) Branched-chain amino acid levels are associated with improvement in insulin resistance with weight loss. Diabetologia 55(2):321–330. https://doi.org/10.1007/s00125-011-2356-5
Lips MA, Van Klinken JB, Van Harmelen V et al (2014) Roux-en-Y gastric bypass surgery, but not calorie restriction, reduces plasma branched-chain amino acids in obese women independent of weight loss or the presence of type 2 diabetes. Diabetes Care 37(12):3150–3156. https://doi.org/10.2337/DC14-0195
Jump RLP, Polinkovsky A, Hurless K et al (2014) Metabolomics analysis identifies intestinal microbiota-derived biomarkers of colonization resistance in clindamycin-treated mice. PLoS One 9(7):e101267. https://doi.org/10.1371/journal.pone.0101267
Alam YH, Kim R, Jang C (2022) Metabolism and health impacts of dietary sugars. J Lipid Atheroscler 11(1):20–38. https://doi.org/10.12997/JLA.2022.11.1.20
Mardinoglu A, Stančáková A, Lotta LA et al (2017) Plasma mannose levels are associated with incident type 2 diabetes and cardiovascular disease. Cell Metab 26(2):281–283. https://doi.org/10.1016/J.CMET.2017.07.006
Swithers SE, Shearer J (2017) Sweetener associated with increased adiposity in young adults. Nat Rev Endocrinol 13:443–444
Hiele M, Ghoos Y, Rutgeerts P, Vantrappen G (1993) Metabolism of erythritol in humans: comparison with glucose and lactitol. Br J Nutr 69(1):169–176. https://doi.org/10.1079/bjn19930019
Hootman KC, Trezzi JP, Kraemer L et al (2017) Erythritol is a pentose-phosphate pathway metabolite and associated with adiposity gain in young adults. Proc Natl Acad Sci U S A 114(21):E4233–E4240. https://doi.org/10.1073/pnas.1620079114
Mousa A, Naderpoor N, Mellett N et al (2019) Lipidomic profiling reveals early-stage metabolic dysfunction in overweight or obese humans. Biochim Biophys Acta Mol Cell Biol Lipids 1864(3):335–343. https://doi.org/10.1016/j.bbalip.2018.12.014
Rosen RT, Hiserodt RD, Fukuda EK et al (2001) Determination of allicin, S-allylcysteine and volatile metabolites of garlic in breath, plasma or simulated gastric fluids. J Nutr Am Inst Nutr 131(3s):968S-971S. https://doi.org/10.1093/jn/131.3.968S
Borucki K, Schreiner R, Dierkes J et al (2005) Detection of recent ethanol intake with new markers: comparison of fatty acid ethyl esters in serum and of ethyl glucuronide and the ratio of 5-hydroxytryptophol to 5-hydroxyindole acetic acid in urine. Alcohol Clin Exp Res 29(5):781–787. https://doi.org/10.1097/01.ALC.0000164372.67018.EA
van de Luitgaarden IAT, Schrieks IC, Kieneker LM et al (2020) Urinary ethyl glucuronide as measure of alcohol consumption and risk of cardiovascular disease: a population-based cohort study. J Am Heart Assoc 9(7):e014324. https://doi.org/10.1161/JAHA.119.014324
Würtz P, Wang Q, Kangas AJ et al (2014) Metabolic signatures of adiposity in young adults: mendelian randomization analysis and effects of weight change. PLoS Med 11(12):e1001765. https://doi.org/10.1371/journal.pmed.1001765
Perez-Cornago A, Brennan L, Ibero-Baraibar I et al (2014) Metabolomics identifies changes in fatty acid and amino acid profiles in serum of overweight older adults following a weight loss intervention. J Physiol Biochem 70(2):593–602. https://doi.org/10.1007/s13105-013-0311-2
Taylor R, Al-Mrabeh A, Zhyzhneuskaya S et al (2018) Remission of human type 2 diabetes requires decrease in liver and pancreas fat content but is dependent upon capacity for β cell recovery. Cell Metab 28(4):547-556.e3. https://doi.org/10.1016/J.CMET.2018.07.003
März W, Scharnagl H, Winkler K et al (2004) Low-density lipoprotein triglycerides associated with low-grade systemic inflammation, adhesion molecules, and angiographic coronary artery disease: the Ludwigshafen Risk and Cardiovascular Health Study. Circulation 110(19):3068–3074. https://doi.org/10.1161/01.CIR.0000146898.06923.80
Kim WJ, Park CY (2013) 1,5-Anhydroglucitol in diabetes mellitus. Endocrine 43(1):33–40. https://doi.org/10.1007/S12020-012-9760-6/TABLES/1
Taylor R (2008) Pathogenesis of type 2 diabetes: tracing the reverse route from cure to cause. Diabetologia 51:1781–1789. https://doi.org/10.1007/s00125-008-1116-7
Davies MJ, Aroda VR, Collins BS et al (2022) Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 45(11):2753–2786. https://doi.org/10.2337/DCI22-0034
RStudio Team (2016) RStudio: integrated development environment. RStudio Inc., Boston, MA, USA
R Core Team (2020) R: a language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
We thank the NHS Primary Care Research Network and North East Commissioning Support for their support and valuable input to recruitment. We thank E. Butler, J. Cooney, S.-J. Duffus and P. Stewart from the University of Glasgow for providing technical assistance, H. Pilkington from the Newcastle upon Tyne Hospitals NHS Foundation Trust for providing research nurse support, and S. Weeden and S. Cadzow from the Robertson Centre for Biostatistics. We thank W. Leslie and research dietitians L. McCombie, G. Thom, N. Brosnahan and A. Barnes for their contributions to the collection and transport of samples. We are enormously grateful to the GP practices, healthcare professionals and volunteers for their participation.
We thank D. Pournaras (Department of Bariatric and Metabolic Surgery, North Bristol NHS Trust) for his contribution to manuscript preparation.
Data availability
The data used for analysis are available on a research data repository (https://researchdata.gla.ac.uk/) with access given to researchers subject to appropriate data sharing agreements. Requests to access data should be made to the Principal Investigators of DiRECT via https://www.directclinicaltrial.org.uk/directstudyteam.html quoting project title ‘What lies behind the causal impact of body mass index (BMI) level and change on human health? Added value from complementary study design and deep metabolic phenotyping’. Metabolite data preparation, data pre-processing, statistical analyses and figure generation were performed in R Studio v.1.0.143 [42] using R v.4.0.2 [43]. The R code for this study has been made publicly available on GitHub at: https://github.com/lauracorbin/metabolomics_of_direct.
Funding
The DiRECT study was funded as a Strategic Research Initiative by Diabetes UK (award no. 13/0004691). The formula diet was donated by Cambridge Weight Plan. Neither organisation had any input into the study design, data analysis or interpretation. Metabolomics analysis was funded by Wellcome Trust (award number 202802/Z/16/Z). NJT is a Wellcome Trust Investigator (202802/Z/16/Z), is the principal investigator of the Avon Longitudinal Study of Parents and Children (MRC & WT 217065/Z/19/Z), is supported by the University of Bristol NIHR Biomedical Research Centre (BRC-1215–2001) and the MRC Integrative Epidemiology Unit (MC_UU_00011/1), and works within the CRUK Integrative Cancer Epidemiology Programme (C18281/A29019). DAH and LJC are supported by NJT’s Wellcome Investigator Award (202802/Z/16/Z). EEV is supported by a Diabetes UK RD Lawrence Fellowship (17/0005587), by Cancer Research UK (C18281/A29019) and by the World Cancer Research Fund (WCRF UK), as part of the World Cancer Research Fund International grant programme (IIG_2019_2009). CJB is supported by EEV’s World Cancer Research Fund grant (IIG_2019_2009). MLS is supported by the Wellcome Trust through a PhD studentship (218495/Z/19/Z). RT is the chief investigator of the study ‘Reversal of Type 2 diabetes Upon Normalisation of Energy intake in non-obese people’ (ReTUNE) funded by Diabetes UK (17/0005645). NS acknowledges funding support from the British Heart Foundation Research Excellence Award (RE/18/6/34217). This research was funded in whole, or in part, by the Wellcome Trust (202802/Z/16/Z).
The study sponsors/funders were not involved in the design of the study; the collection, analysis, and interpretation of data; and writing the report; and did not impose any restrictions regarding the publication of the report.
Authors’ relationships and activities
RT has received lecture honoraria from Eli Lilly, Nestle Health and Janssen. NS has received consulting and/or speaker honoraria from Abbott Laboratories, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Hanmi Pharmaceuticals, Janssen, Merck Sharp & Dohme, Novartis, Novo Nordisk, Pfizer, Roche Diagnostics, and Sanofi, and grant funding support paid to his University from AstraZeneca, Boehringer Ingelheim, Novartis and Roche Diagnostics outside the submitted work. LC is an Associate Editor at Diabetologia. All other authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
NJT, LJC and NS made substantial contributions to the conception or design of the work. NJT, LJC, RT, MEJL, AM, PW and C-MM contributed through acquisition of data and LJC, NJT, NS, MLS, CJB, EEV and DAH through analysis and interpretation of data. LJC, NJT, NS, RT, MEJL, MLS, PW, CJB, AM, C-MM and EEV contributed to the drafting the article and reviewing it critically for important intellectual content. All authors gave final approval of the version to be published. LJC is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Corbin, L.J., Hughes, D.A., Bull, C.J. et al. The metabolomic signature of weight loss and remission in the Diabetes Remission Clinical Trial (DiRECT). Diabetologia 67, 74–87 (2024). https://doi.org/10.1007/s00125-023-06019-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-023-06019-x