Abstract
Aims/hypothesis
Continuous subcutaneous insulin infusion by insulin pump is often superior in improving glycaemic control compared with conventional multiple daily insulin injection (MDI). However, whether pump treatment leads to improved pregnancy outcomes in terms of congenital malformations and perinatal death remains unknown. The present aim was to evaluate the risk of malformations and perinatal and neonatal death in pregnant women with type 1 diabetes treated with pump or MDI.
Methods
We performed a secondary analysis of a prospective multinational cohort of 2088 pregnant women with type 1 diabetes in a real-world setting who were treated by pump (n=750) or MDI (n=1338). ORs for offspring with congenital malformations or perinatal or neonatal death were calculated using crude data and by logistic regression on propensity score-matched data.
Results
At enrolment (gestational week 8; 95% CI 4, 14), pump users had a higher educational level (university degree: 37.3% vs 25.1%; p<0.001) and better glycaemic control (mean HbA1c: 51±10 mmol/mol [6.8±0.9%] vs 54±14 mmol/mol [7.1±1.3%], p<0.001) compared with MDI users. Moreover, a greater proportion of pump users had an HbA1c level below 75 mmol/mol (9%) (97.6% vs 91.9%, p<0.001), and more often reported taking folic acid supplementation (86.3% vs 74.8%; p<0.001) compared with MDI users. All clinically important potential confounders were balanced after propensity score matching, and HbA1c remained lower in pump users. The proportion of fetuses with at least one malformation was 13.5% in pump users vs 11.2% in MDI users (crude OR 1.23; 95% CI 0.94, 1.61; p=0.13; propensity score-matched (adjusted) OR 1.11; 95% CI 0.81, 1.52; p=0.52). The proportion of fetuses with at least one major malformation was 2.8% in pump users vs 3.1% in MDI users (crude OR 0.89; 95% CI 0.52, 1.51; p=0.66; adjusted OR 0.78; 95% CI 0.42, 1.45; p=0.43), and the proportions of fetuses carrying one or more minor malformations (but no major malformations) were 10.7% vs 8.1% (crude OR 1.36; 95% CI 1.00, 1.84; p=0.05; adjusted OR 1.23; 95% CI 0.87, 1.75; p=0.25). The proportions of perinatal and neonatal death were 1.6% vs 1.3% (crude OR 1.23; 95% CI 0.57, 2.67; p=0.59; adjusted OR 2.02; 95% CI 0.69, 5.93; p=0.20) and 0.3% vs 0.3% (n=2 vs n=4, p=not applicable), respectively.
Conclusions/interpretations
Insulin pump treatment was not associated with a lower risk of congenital malformations, despite better glycaemic control in early pregnancy compared with MDI. Further studies exploring the efficacy and safety of pump treatment during pregnancy are needed.
Graphical abstract

Similar content being viewed by others

Introduction
Congenital malformations and perinatal mortality are serious complications for the offspring of women with type 1 diabetes mellitus, related to impaired glycaemic control, and are two to four times more frequent in the offspring of these women compared with the background population [1,2,3,4]. Poor peri-conceptional glycaemic control is strongly associated with the risk of congenital malformations in infants born to women with type 1 diabetes, and is the most important modifiable risk factor [3,4,5]. To a lesser extent, high maternal educational level [6] and folic acid supplementation [7] have been shown to be associated with a lower prevalence of malformations, whereas diabetic complications such as retinopathy and nephropathy are associated with a higher prevalence of malformations [5, 8]. Perinatal mortality risk in women with type 1 diabetes is multifactorial in origin, but poor glycaemic control appears to be a key modifiable factor in placing women at increased risk [9,10,11,12].
Outside pregnancy, several studies have suggested that continuous subcutaneous insulin infusion by insulin pump improves glycaemic control compared with conventional treatment by multiple daily injections (MDI) of insulin [13,14,15,16]. Thus, insulin pump treatment is becoming increasingly used throughout Europe, Canada and the USA, with the aim of improving glycaemic control and quality of life [17]. Despite the expectation that insulin pump treatment will improve glycaemic control and reduce the prevalence of complications in pregnancy [18, 19], the anticipated benefit of using pump treatment during pregnancy has not yet been demonstrated, and papers evaluating the prevalence of congenital malformations and/or perinatal death in women who use pumps compared with MDI treatment are lacking.
The low incidence of malformations and perinatal death invoke the need for large cohort studies to evaluate the risk of congenital malformations and perinatal death in insulin pump users in a real-world setting, as randomised control trials are difficult to perform in this context. We recently established a large, multinational, prospective, non-interventional cohort – the so-called Diabetes Pregnancy Registry – that includes data from more than 2000 pregnant women with pre-existing type 1 diabetes, and assessed the impact of various long-acting insulin analogues on glycaemic control and pregnancy outcome in MDI-treated women in the EVOLVE study [20,21,22]. The Diabetes Pregnancy Registry includes 750 women who use pump treatment, which provides a unique opportunity to test our hypothesis that pump treatment in real-world conditions is associated with a reduced risk of congenital malformations and perinatal death.
The primary aim of this study was to evaluate the risk of having an offspring with congenital malformations or perinatal or neonatal death in women with type 1 diabetes treated using a pump vs MDI before and during pregnancy.
Methods
The present study is an analysis of the participants in the Diabetes Pregnancy Registry including the EValuation Of LeVEmir in Pregnancy (EVOLVE) study cohort [20]. Briefly, the study (ClinicalTrials.gov, number NCT01892319) was a multinational, prospective, non-interventional, multicentre cohort study designed to monitor and assess the safety of insulin detemir in pregnant women with pre-existing diabetes and their offspring. As part of the observational data collection, equivalent data were collected from pregnant women with pre-existing diabetes treated using other injectable glucose-lowering treatment regimens. This international Diabetes Pregnancy Registry is a unique opportunity for large-scale data collection that allows comparisons and analysis between various insulin treatment regimens in pregnant women with diabetes mellitus. The study covered the gestational period of women with pre-existing type 1 or type 2 diabetes, and a follow-up period for their infants to 1 year of age, with the frequency and mode of standard routine visits determined by the individual study site.
In the present analysis of this cohort, we investigated women with type 1 diabetes treated with pump therapy or MDI during pregnancy. Women treated with pump therapy or MDI followed the local routine care without a predefined schedule of study visits during pregnancy. Postpartum follow-up at 1 month and 1 year was performed using questionnaires and telephone interviews, and collected information on neonatal death (yes or no) and congenital malformations that were not detected at delivery or changes in major congenital malformations (see electronic supplementary material [ESM] Table 1).
Recruitment took place between September 2013 and September 2018. During the enrolment visit, signed informed consent was obtained after an eligibility check based on the inclusion criteria, which were: a positive pregnancy test and gestational age ≤16 weeks at enrolment, type 1 diabetes diagnosed prior to conception, and treatment for at least 1 month prior to conception with either pump therapy or MDI. Women were excluded if they withdrew consent or were lost to follow-up prior to the end of their pregnancy. All singleton offspring were investigated; for twin pregnancies, one of the offspring was randomly selected for investigation (Fig. 1).
At the enrolment visit, clinical data were collected by interview or extracted from medical records as previously described [21]. Information included aspects relating to maternal medical history (including the presence of hypertension), diabetes history and diabetes complications (diabetic retinopathy, diabetic neuropathy and diabetic nephropathy), current glucose-lowering treatment, obstetric history, current pregnancy information, folic acid intake before and during the first trimester, socioeconomic status, race, smoking and alcohol intake. At the first visit, BMI, BP (systolic/diastolic) and HbA1c (at maximum 16 weeks’ gestation) were recorded.
All pregnancies ending in spontaneous miscarriage or medically induced termination, or a liveborn or stillborn offspring, were recorded. Offspring were evaluated for any congenital malformations irrespective of whether liveborn or stillborn, as determined by the local practice, up to 1 month of age. Severe cases of malformations leading to medically induced termination of pregnancy were also registered.
All data were collected using electronic case report forms that were completed by physicians or their authorised staff. Major endpoints were verified by a physician.
Endpoints
The primary endpoint was offspring with any congenital malformation (major and/or minor) (yes/no) diagnosed at birth or up to 1 year of age, including fetuses with major congenital malformation leading to medically induced termination of pregnancy. Fetuses with congenital malformations were divided into fetuses with one or more major congenital malformation and fetuses with one or more minor congenital malformation but no major malformation. A major congenital malformation was defined as a life-threatening structural malformation or an abnormality likely to cause significant impairment of health or functional capacity that requires medical or surgical treatment [23]. Minor malformations were defined as malformations that did not fulfil the criteria for a major malformation. The majority of the malformations were present at birth, and the medical records were used for documentation. In addition, any possible changes in the presence of malformations within the first year of life were determined from the medical record. Secondary outcomes included spontaneous miscarriages and medically induced termination of pregnancy before 22 weeks’ gestation, stillbirth (from 22 weeks’ gestation to delivery), perinatal death (from 22 weeks’ gestation to 7 days after birth) or neonatal death (death of a liveborn infant 0–28 days after delivery).
Statistical methods
Data management and statistical analyses were performed using SAS 9.4 M5 (SAS Institute, USA). A p value <0.05 was used to indicate statistical significance. In the case of missing information for required variables, patients were excluded from the respective analysis.
Descriptive analyses were performed to summarise the characteristics of each treatment group at enrolment. For all binary endpoints (yes/no), total numbers and percentages are reported for pump therapy and MDI users. For continuous variables that followed a Gaussian distribution, means and SD are reported. For continuous variables that did not follow a Gaussian distribution, median and IQR are reported. Descriptive data were compared using χ2 or Fisher’s exact tests for categorical variables and Student’s t test, the Wilcoxon test and the Welch–Satterthwaite test for continuous variables as applicable.
For all primary and secondary endpoints, both crude and propensity score-matched (adjusted) analyses were performed to compare the risk between treatment groups. We calculated OR as odds in the pump therapy group/odds in the MDI group using logistic regression. However, linear regression was used for HbA1c, and the results are given as the relative difference as a percentage between the pump therapy group and the MDI group, as HbA1c values were log-transformed before analysis. Because there were relatively few events for several of the outcomes, we used propensity score matching to adjust the estimated OR between groups for potential confounding. Propensity scores were based on the following potential confounders: maternal age, duration of diabetes, history of at least one long-term diabetes complication (diabetic retinopathy, diabetic nephropathy and diabetic neuropathy), folic acid taken before and during the first trimester, history of spontaneous miscarriage, history of major malformations, BMI and education (proportion receiving a university degree). The nearest neighbour pair-matching without replacement, with a calliper width of 0.2 of the standard deviation of the logit of the propensity scores (predicted values), was used. Pump therapy users were matched with MDI users 1:1. For outcomes with fewer than ten events in each treatment group, data were not statistically tested and are summarised descriptively.
A sensitivity analysis was also performed, restricted to offspring of women from countries that contributed at least 30 participants to each treatment group.
Ethics statement
All participants gave written informed consent to participate in the observational cohort study. The study was performed in accordance with the Declaration of Helsinki and the International Society for Pharmaceutical Engineering Guidelines for Good Pharmacoepidemiology Practice, and was approved separately in each of the participating countries by national health authorities, local institutional review boards or independent ethics committees.
Results
Participants
Overall, 2601 women were invited to participate in the study, of whom 155 did not accept the invitation. Of the 2446 possible participants, 331 did not meet the inclusion criteria for the present study. Therefore, 2115 pregnant women with type 1 diabetes were enrolled in early pregnancy, of whom 27 (1%) either withdrew consent or were lost to follow-up prior to the end of pregnancy, resulting in 2088 women being included in this study (Fig. 1). Of these, 750 women were treated with a pump and 1338 women with MDI (Fig. 1). In total, there were 2045 singleton pregnancies (pump 731, MDI 1314) and 43 twin pregnancies (pump 19; MDI 24). A total of 158 pregnancies were lost before 22 weeks’ gestation (pump 58, MDI 100), of which 104 were due to spontaneous miscarriage (pump 31, MDI 73), with the remaining 54 being reported as medically induced termination of pregnancy (pump 27, MDI 27). Of the 54 medically induced terminations of pregnancy, 14 (pump 6, MDI 8) were due to severe malformations present in the fetus. Of the 1930 offspring included in the study, 1908 were liveborn (>22 gestational weeks) and 22 were stillborn (Fig. 1).
The majority of the women were included during early pregnancy (median 8 gestational weeks; IQR 4–14). The participants originated from 15 countries in Europe, Israel and Malaysia. Denmark (n=551), the UK (n=268) and Croatia (n=226) contributed the most participants (ESM Table 2). The baseline characteristics of the women included in the study were comparable between the two treatment groups with a few exceptions (Table 1). Pump users were better educated, i.e. more likely to have a university degree (pump 37.3% vs MDI 25.1%, p<0.001) and had a higher BMI (median [IQR] 25.5 [23.1–28.3] vs 24.3 [22.1–27.6] kg/m2, p<0.001). Pump users also had a longer diabetes duration (mean±SD 18.3±7.8 vs 14.5±8.3 years, p<0.001), with a higher prevalence of retinopathy (35.8% vs 25.0%, p<0.001) but not nephropathy (4.7% vs 4.6%, p=0.93) or neuropathy (3.1% vs 2.9%, p=0.78). A higher proportion of pump users reported having taken folic acid supplementation before and/or during the first trimester of pregnancy (86.3% vs 74.8%, p<0.001) and to be less likely to smoke (4.9% vs 9.0%, p<0.001). Pump-treated women had a lower HbA1c level at enrolment compared with MDI-treated (mean±SD 51±10 mmol/mol [6.8±0.9%] vs 54±14 mmol/mol [7.1±1.3%], p<0.001). Moreover, a greater proportion of pump users had HbA1c level below 75 mmol/mol (9%) (97.6% vs 91.9%, p<0.001). All clinically important potential confounders were balanced after matching, with all standard mean differences less than 0.2 (Table 2). However, the significantly lower HbA1c level in pump users remained at a similar magnitude (51±10 mmol/mol [6.8±0.9%] vs 54±14 mmol/mol [7.1±1.2%], p<0.001) (difference between pump and MDI: 3.2 percentage points; 95% CI 1.6%, 4.8%; p<0.0001). Moreover, the HbA1c levels at enrolment for the subpopulation of 1564 pregnant women from countries contributing with more than 30 women to both treatment groups (ESM Table 3) did not demonstrate any differences from the entire study population, and mean HbA1c levels at enrolment were not different from those of the full cohort (pump 51±10 mmol/mol [6.8±0.9%] vs MDI 54±13.9 mmol/mol [7.1±1.3%], p<0.001).
The majority of the women used insulin aspart in both groups (pump 73.3%, MDI 78.8%), and the most commonly used basal insulins in the MDI group were insulin detemir (45.9%) and insulin glargine (45.4%) (Table 1 and ESM Table 4).
Malformations and mortality risk
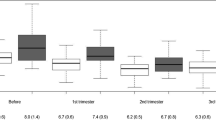
In total, 251 offspring with any malformations were identified, of whom 63 had a least one major congenital malformation. The proportions of offspring with at least one congenital malformation (major and/or minor) were 13.5% in pump users and 11.2% in MDI users (crude OR 1.23; 95% CI 0.94, 1.61; p=0.13; adjusted OR 1.11; 95% CI 0.81, 1.52; p=0.52) (Fig. 2). The proportion of offspring with a least one major congenital malformation was 2.8% vs 3.1% (crude OR 0.89; 95% CI 0.52, 1.51; p=0.66; adjusted OR 0.78; 95% CI 0.42, 1.45; p=0.43) (Fig. 2). A total of 12 offspring had more than one major malformation (0.5% in both groups).
Crude and propensity score-matched analyses of offspring malformations and mortality rate according to maternal type of insulin treatment (pump or MDI). Offspring with malformations and spontaneous miscarriage/medically induced termination were analysed for all fetuses of included women. Stillbirth and perinatal death were analysed for all fetuses born, and neonatal death was analysed for the liveborn population. Any congenital malformations comprise major and/or minor malformations. Major congenital malformation indicates one or more major congenital malformations. Minor congenital malformation indicates one or more minor congenital malformations but no major malformation. Miscarriage and induced termination represent spontaneous miscarriage and medically induced termination of pregnancies that ended before 22 weeks’ gestation. The total numbers included in the analyses differ slightly due to missing information for some of the endpoints
The major congenital malformations across the two groups were most commonly related to the cardiovascular system (n=21), the genitourinary system (n=9) or the nervous system (n=6). Individual details of the type of major malformations and the characteristics of the mothers are presented in ESM Table 5.
Pump users had more offspring with at least one minor malformation but no major malformation compared with MDI users (10.7% vs 8.1%), with a crude OR of 1.36 (95% CI 1.00, 1.84; p=0.05); the adjusted OR was of similar magnitude but was non-significant (OR 1.23;95% CI 0.87, 1.75; p=0.25) (Fig. 2). The minor congenital malformations were mostly related to the cardiovascular system, followed by the genitourinary system.
Crude and propensity score-matched analyses of offspring malformations according to the type of maternal insulin treatment in the subpopulation of 1564 women from the seven countries contributing at least 30 participants to each treatment group are given in ESM Table 3. No obvious differences from the total cohort were identified (ESM Table 3).
Figure 3 shows the prevalence of any congenital malformation (major and/or minor) by category of HbA1c level at enrolment for each treatment group. In women with HbA1c levels above 75 mmol/mol (9%), a numerically increased prevalence (not statistically tested owing to low numbers of participants) of any congenital malformations was observed in MDI-treated women compared to women with lower HbA1c levels. At ‘close to target’ HbA1c levels, pump users had a numerically higher prevalence (not statistically tested owing to low numbers of participants) of any congenital malformations compared to women treated with MDI (Fig. 3).
The proportion of pregnancies resulting in stillbirth (n=9 (1.3%) vs n=13 (1.1%); p=not applicable), perinatal death (n = 11 (1.6%) vs n=16 (1.3%); crude OR 1.23; 95% CI 0.57, 2.67; p=0.59; adjusted OR 2.02; 95% CI 0.69, 5.93; p=0.20) or neonatal death (n=2 (0.3%) vs n=4 (0.3%); p=not applicable) was not different between the two treatment groups.
Discussion
This prospective study of a multinational cohort of 2088 pregnant women with type 1 diabetes revealed that the risks of having an offspring with a congenital malformation was not significantly different for pump treatment compared with MDI treatment. No advantage of pump treatment was demonstrated, either before or after propensity score matching, despite pump users exhibiting better glycaemic control, having a higher educational level, and more frequently reporting supplementation with folic acid.
In the present study, pump-treated women had better glycaemic control at enrolment than the MDI-treated women, in terms of both mean HbA1c level and the percentage without high HbA1c levels, both before and after propensity score matching. This could be anticipated to lead to reduced prevalence of malformations due to the tight relationship between glycaemic control and malformations described in other cohort studies [5, 24, 25]. Therefore, HbA1c was considered as a mediator variable between insulin treatment and prevalence of malformations in the present study.
A recent Danish population-based register study found an adjusted OR of 2.9% for major malformations in women with type 1 diabetes, mainly driven by women with sub-optimal glycaemic control [3]. This is in line with our findings in the few women with HbA1c levels above 75 mmol/mol (9%), with a numerically increased prevalence of any congenital malformations in MDI-treated women with higher HbA1c levels compared to women with lower HbA1c levels. However, in the Danish population study, the risk for major malformations was not significantly greater than for the background population when HbA1c levels were below 48 mmol/mol (6.5%) in early pregnancy [3]. As we observed generally good glycaemic control in both treatment groups in the present study, with most women having an HbA1c level below 75 mmol/mol (9%) and the mean HbA1c being close to 48 mmol/mol (6.5%), we therefore cannot exclude the possibility that the level of glycaemic control in both groups did not leave much room for further reduction in the prevalence of major malformations in the pump users. Baseline HbA1c levels reflect the glycaemic control for the preceding approximately 8 weeks, during which organogenesis of the offspring organs, including the heart, mainly takes place. In this study, the HbA1c levels at baseline, which mainly cover the time before the women recognise their pregnancy, show better glycaemic control in women using an insulin pump compared with MDI. In addition, pump treatment has been reported to reduce glucose fluctuations compared with MDI treatment [26]. Therefore, the numerically higher prevalence of any malformations in the pump users appears not to be related to less optimal glycaemic control. Other factors than glycaemic control are probably involved in the numerically higher prevalence of malformations in pump-treated women, but this remains speculative and needs to be confirmed in other studies.
Supplementation with folic acid [7], a good maternal socioeconomic level, [6] and avoiding smoking [27] are known factors related to a reduced risk of malformations in the healthy population [6, 7]. Interestingly, in the present study, pump users appeared to have higher socioeconomic status (evidenced by a higher maternal educational level) and were more likely to take the recommended folic acid supplementation and be non-smokers. Together, this suggests a healthier lifestyle in the pump users, which is expected to contribute to a lower prevalence of malformations. On the other hand, insulin pump treatment is often initiated in women with inappropriate glycaemic control, and pump users may therefore represent women with more challenging diabetes. Unfortunately, we were only able to report HbA1c levels, and have no data on fluctuation of plasma glucose. The observed higher prevalence of retinopathy in pump users in the present study may be indicative of a history of prolonged poor glycaemic control, which could increase the risk of malformations [5, 8]. However, our propensity score-matched data took these factors into account, and demonstrated that prevalence of malformations was not significantly different regardless of pump treatment or not. It is possible that, as women on pump therapy were better educated, they may have increased diabetes awareness and may adhere to the screening programme for retinopathy more carefully, leading to a higher prevalence of retinopathy being detected compared to women treated with MDI.
The prevalence of stillbirths and neonatal mortality was not numerically different between treatment modalities, but was not statistically tested due to the low number of events in the cohort. The prevalence of perinatal mortality was not significantly different between pump and MDI users. The perinatal mortality risk was mainly driven by stillbirth and is higher than the prevalence of perinatal mortality risk in the Danish background population (approximately 0.4%) [28]. We are not aware of any published data regarding perinatal mortality rate in pump-treated women, but an observational study found that offspring of pump users were more likely to be admitted to neonatal care units for more than 48 h than offspring of MDI users [18].
The present study has several strengths. Data were collected prospectively from early pregnancy, included many relevant clinical variables to adjust for potential confounders, and comprised real-world data from many nationalities and healthcare systems, thereby increasing the generalisability of the findings. One limitation is that the presence of microvascular complications was combined into one variable in the propensity score matching. However, the prevalence of retinopathy was 36% and 25%, respectively, in the pump and MDI groups, while the prevalence of nephropathy was below 5% in both groups. Despite including more than 2000 women, we observed few events for many of the outcomes, resulting in a relatively low statistical power, especially for perinatal death, and the number of offspring with malformations was too small to assess any differences in the various classes of malformations. Even though the presence of congenital malformations was identified through medical records and verified by a physician, it may be possible that the more highly educated pump users were more likely to identify malformations in their offspring and have them reported.
A further limitation is that the women were recruited from selected sites with routine care ensuring relatively good glycaemic control, which may affect the generalisability of the study. Also, that data were collected between 2013 and 2018. Since then, insulin pump technology has improved, and we cannot exclude the possibility that use of more modern insulin pumps may have a different impact on congenital malformations. Studies including newer insulin pumps with closed-loop systems are warranted.
Our finding of no significant difference in the prevalence of malformations in the offspring of women with and without insulin pump treatment despite more appropriate HbA1c level, and even a non-significant higher prevalence of minor malformations in pump users, was surprising, and suggests the need for further studies evaluating the impact of insulin pump use on development of malformations. Population-based studies are required to evaluate the impact of pump treatment on rare events such as malformations and perinatal death. Investigating possible independent predictors of malformations, including HbA1c level, treatment modality, folic acid supplementation and late diabetes complications, is warranted. The prevalence of other poor pregnancy outcomes such as fetal overgrowth, pre-eclampsia and preterm delivery in pump-treated women will be analysed in a separate report based on this real-world cohort.
In conclusion, it was surprising that the risk of congenital malformations was not lower in offspring of women treated with insulin pumps despite better glycaemic control in early pregnancy, when compared with women receiving MDI treatment. Further studies exploring the efficacy and safety of using pump treatment during pregnancy are needed.
Data availability
Source data are available from the corresponding author on written request.
Abbreviations
- EVOLVE:
-
EValuation Of LeVEmir in Pregnancy
- MDI:
-
Multiple daily injections
References
Feig DS, Hwee J, Shah BR, Booth GL, Bierman AS, Lipscombe LL (2014) Trends in incidence of diabetes in pregnancy and serious perinatal outcomes: a large, population-based study in Ontario, Canada, 1996–2010. Diabetes Care 37(6):1590–1596. https://doi.org/10.2337/dc13-2717
Ludvigsson JF, Neovius M, Söderling J et al (2018) Periconception glycaemic control in women with type 1 diabetes and risk of major birth defects: population based cohort study in Sweden. BMJ 362:k2638. https://doi.org/10.1136/bmj.k2638
Arendt LH, Pedersen LH, Pedersen L et al (2021) Glycemic control in pregnancies complicated by pre-existing diabetes mellitus and congenital malformations: a Danish population-based study. Clin Epidemiol 13:615–626. https://doi.org/10.2147/CLEP.S298748
Eriksen NB, Damm P, Mathiesen ER, Ringholm L (2019) The prevalence of congenital malformations is still higher in pregnant women with pregestational diabetes despite near-normal HbA1c: a literature review. J Matern Fetal Neonatal Med 32(8):1225–1229. https://doi.org/10.1080/14767058.2017.1402880
Bell R, Glinianaia SV, Tennant PWG, Bilous RW, Rankin J (2012) Peri-conception hyperglycaemia and nephropathy are associated with risk of congenital anomaly in women with pre-existing diabetes: a population-based cohort study. Diabetologia 55(4):936–947. https://doi.org/10.1007/s00125-012-2455-y
Dolk H, McCullough N, Callaghan S et al (2020) Risk factors for congenital heart disease: The Baby Hearts Study, a population-based case–control study. PLoS One 15(2):e0227908. https://doi.org/10.1371/journal.pone.0227908
De-Regil LM, Peña-Rosas JP, Fernández-Gaxiola AC, Rayco-Solon P (2015) Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst Rev 12(12):CD007950. https://doi.org/10.1002/14651858.CD007950.pub3
Øyen N, Diaz LJ, Leirgul E et al (2016) Prepregnancy diabetes and offspring risk of congenital heart disease: a nationwide cohort study. Circulation 133(23):2243–2253. https://doi.org/10.1161/CIRCULATIONAHA.115.017465
Wardinger JE, Ambati S (2021) Placental insufficiency. StatPearls Publishing, Treasure Island, FL. Available from https://www.ncbi.nlm.nih.gov/books/NBK563171/. Accessed 28 Nov 2022
Wang M, Athayde N, Padmanabhan S, Cheung NW (2019) Causes of stillbirths in diabetic and gestational diabetes pregnancies at a NSW tertiary referral hospital. Aust NZ J Obstet Gynaecol 59(4):561–566. https://doi.org/10.1111/ajo.12936
Mackin ST, Nelson SM, Wild SH, Colhoun HM, Wood R, Lindsay RS (2019) Factors associated with stillbirth in women with diabetes. Diabetologia 62(10):1938–1947. https://doi.org/10.1007/s00125-019-4943-9
Lauenborg J, Mathiesen E, Ovesen P et al (2003) Audit on stillbirths in women with pregestational type 1 diabetes. Diabetes Care 26(5):1385–1389. https://doi.org/10.2337/diacare.26.5.1385
Fatourechi MM, Kudva YC, Murad MH, Elamin MB, Tabini CC, Montori VM (2009) Clinical review: Hypoglycemia with intensive insulin therapy: a systematic review and meta-analyses of randomized trials of continuous subcutaneous insulin infusion versus multiple daily injections. J Clin Endocrinol Metab 94(3):729–740. https://doi.org/10.1210/jc.2008-1415
Feldt-Rasmussen B, Mathiesen ER, Jensen T, Lauritzen T, Deckert T (1991) Effect of improved metabolic control on loss of kidney function in type 1 (insulin-dependent) diabetic patients: an update of the Steno studies. Diabetologia 34(3):164–170. https://doi.org/10.1007/BF00418270
Pickup JC (2012) Management of diabetes mellitus: is the pump mightier than the pen? Nat Rev Endocrinol 8(7):425–433. https://doi.org/10.1038/nrendo.2012.28
Pickup JC (2012) Insulin-pump therapy for type 1 diabetes mellitus. N Engl J Med 366(17):1616–1624. https://doi.org/10.1056/NEJMct1113948
Ringholm L, Damm P, Mathiesen ER (2019) Improving pregnancy outcomes in women with diabetes mellitus: modern management. Nat Rev Endocrinol 15(7):406–416. https://doi.org/10.1038/s41574-019-0197-3
Feig DS, Corcoy R, Donovan LE et al (2018) Pumps or multiple daily injections in pregnancy involving type 1 diabetes: a prespecified analysis of the CONCEPTT randomized trial. Diabetes Care 41(12):2471–2479. https://doi.org/10.2337/dc18-1437
Mukhopadhyay A, Farrell T, Fraser RB, Ola B (2007) Continuous subcutaneous insulin infusion vs intensive conventional insulin therapy in pregnant diabetic women: a systematic review and metaanalysis of randomized, controlled trials. Am J Obstet Gynecol 197(5):447–456. https://doi.org/10.1016/j.ajog.2007.03.062
Mathiesen ER, Andersen H, Kring SII, Damm P (2017) Design and rationale of a large, international, prospective cohort study to evaluate the occurrence of malformations and perinatal/neonatal death using insulin detemir in pregnant women with diabetes in comparison with other long-acting insulins. BMC Pregnancy Childbirth 17(1):38. https://doi.org/10.1186/s12884-016-1177-4
Mathiesen ER, Ali N, Anastasiou E et al (2021) Characteristics of pregnant women with diabetes using injectable glucose-lowering drugs in the EVOLVE study. J Matern Fetal Neonatal Med 35(25):7992–8000. https://doi.org/10.1080/14767058.2021.1940132
Mathiesen ER, Ali N, Alibegovic AC et al (2021) Risk of major congenital malformations or perinatal or neonatal death with insulin detemir versus other basal insulins in pregnant women with preexisting diabetes: the real-world EVOLVE study. Diabetes Care 44(9):2069–2077. https://doi.org/10.2337/dc21-0472
EUROCAT Central Registry (2005) EUROCAT Guide 1.3 and reference documents: Instructions for the Registration and Surveillance of Congenital Anomalies. Available from https://eu-rd-platform.jrc.ec.europa.eu/sites/default/files/EUROCAT-Guide-1.3.pdf. Accessed 12 Nov 2020
Glinianaia SV, Tennant PWG, Bilous RW, Rankin J, Bell R (2012) HbA1c and birthweight in women with pre-conception type 1 and type 2 diabetes: a population-based cohort study. Diabetologia 55(12):3193–3203. https://doi.org/10.1007/s00125-012-2721-z
Ekbom P, Damm P, Feldt-Rasmussen B, Feldt-Rasmussen U, Jensen DM, Mathiesen ER (2008) Elevated third-trimester haemoglobin A1c predicts preterm delivery in type 1 diabetes. J Diabetes Complications 22(5):297–302. https://doi.org/10.1016/j.jdiacomp.2007.03.008
Xiaojuan J, Yunfeng S, Yifa C (2022) Better TIR, HbA1c, and less hypoglycemia in closed-loop insulin system in patients with type 1 diabetes: a meta-analysis. MJ Open Diab Res Care 10(2):e002633. https://doi.org/10.1136/bmjdrc-2021-002633
Leite M, Albieri V, Kjaer SK, Jensen A (2014) Maternal smoking in pregnancy and risk for congenital malformations: results of a Danish register-based cohort study. Acta Obstet Gynecol Scand 93(8):825–834. https://doi.org/10.1111/aogs.12433
Damsted Rasmussen T, Villadsen SF, Kragh Andersen P, Smith Jervelund S, Nybo Andersen A-M (2021) Social and ethnic disparities in stillbirth and infant death in Denmark, 2005–2016. Sci Rep 11(1):8001. https://doi.org/10.1038/s41598-021-87084-3
Acknowledgements
The authors thank all investigators, staff and participants of this study. A list of all investigators involved in the EVOLVE study cohort is listed in the ESM. Parts of this study were presented by Mathiesen et al at the ADA 2020 meeting (poster 172-LB) and by Mathiesen et al at the EASD 2020 meeting (oral presentation 85). Data from this study were presented at the EASD 2022 meeting (short oral presentation 49) by Thorius et al.
Authors’ relationships and activities
IHT, LLNH, RBN, ACA and M-AG are employers of, and hold shares in, Novo Nordisk. ERM has received speaker’s fees from Novo Nordisk, and has participated in steering committee tasks and guidance involving writing protocols for Novo Nordisk. ERM is participating in several multinational clinical studies on the use of insulin in pregnant women with pre-existing diabetes, in collaboration with Novo Nordisk. ERM is a member of the editorial board of Diabetologia. The remaining author (JP) declares that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
The EVOLVE study, including the study design, data collection, analysis and interpretation, was funded by Novo Nordisk.
Author information
Authors and Affiliations
Contributions
IHT, LLNH, ACA, M-AG and ERM conceptualised and designed the study. IHT, LLNH, RBN and JP performed the statistical analyses. IHT and ERM drafted the manuscript. All authors were involved in the interpretation of results, edited the manuscript, and provided input, critical review and approval of the final version of the manuscript. All named authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. IHT and ERM accept responsibility for the overall conduction, integrity and accuracy of the work, had access to the data, and controlled the decision to publish.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM
(PDF 239 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thorius, I.H., Husemoen, L.L.N., Nordsborg, R.B. et al. Congenital malformations among offspring of women with type 1 diabetes who use insulin pumps: a prospective cohort study. Diabetologia 66, 826–836 (2023). https://doi.org/10.1007/s00125-022-05864-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05864-6






