Abstract
Aims/hypothesis
We aimed to investigate the nationwide trends in incidence and associated risk factors, with focus on blood glucose-lowering medication, for the first hypoglycaemic episode leading to hospitalisation in Denmark among people with type 1 and 2 diabetes mellitus.
Methods
A cohort study of all people with diabetes from 1977 to 2018 experiencing hypoglycaemic episodes leading to hospitalisation in 1998–2018 was established. Data were extracted from the Danish National Patient Registry. Trends in incidence rates were investigated with Poisson regression models and linear regressions, and risk factors were investigated with Cox proportional hazards models.
Results
A total of 66,438 hypoglycaemic episodes leading to hospitalisation in 1998–2018 was investigated among 641,402 people with type 1 (mean ± SD age 37 ± 22 years) and type 2 diabetes (mean ± SD age 61 ± 17 years). Between 2003 and 2018, the incidence rate fell by 66% for type 1 diabetes (incidence rate ratio [IRR] 0.34 [95% CI 0.31, 0.36], p < 0.0001) and 61% for type 2 diabetes (IRR 0.39 [95% CI 0.36, 0.42], p < 0.0001). With respect to hypoglycaemic episodes, insulin glargine (HR 1.20 [95% CI 1.05, 1.36], p = 0.0059), insulin detemir (HR 1.18 [95% CI 1.04, 1.32], p = 0.0077) and insulin degludec (HR 1.04 [95% CI 0.81,1.33], p = 0.7706) seemed safer than human insulin (long-acting insulin HR 1.38 [95% CI 1.25, 1.52], p < 0.0001; combination insulins HR 1.84 [95% CI 1.65, 2.05], p < 0.0001) and, especially, sodium–glucose cotransporter 2 inhibitors (HR 0.43 [95% CI 0.33, 0.56], p < 0.0001), glucagon-like peptide 1 receptor agonists (HR 0.51 [95% CI 0.44, 0.58], p < 0.0001) and dipeptidyl peptidase 4 inhibitors (HR 0.44 [95% CI 0.38, 0.49], p < 0.0001) seemed safer than sulfonylureas (HR 2.27 [95% CI 2.18, 2.37], p < 0.0001).
Conclusions/interpretation
Incidence rates of hypoglycaemic episodes leading to hospitalisation are declining in Denmark, and the advent of new treatment alternatives may play a significant role in this decline. From a safety perspective, these findings are important and should be considered by clinicians when assessing treatment options for patients.
Graphical abstract

Similar content being viewed by others

Introduction
Almost one-third of people with diabetes require treatment with insulin [1] and, at some point in disease progression, intensive insulin therapy to maintain tight glycaemic control will be necessary [2]. This comes with the trade-off of an increased risk of developing severe hypoglycaemic episodes, as reported by the DCCT [3]. An analysis of the DCCT/Epidemiology of Diabetes Interventions and Complications (EDIC) type 1 diabetes cohort [4] showed equilibrated rates of severe hypoglycaemic episodes (~40 episodes per 100 person-years) in the intervention group (intensive diabetes therapy) and control group (conventional diabetes therapy) after ~30 years of follow-up. This finding was associated with advanced diabetes and similar HbA1c levels, making severe hypoglycaemic episodes a persistent challenge for people with type 1 diabetes across their life span.
Severe hypoglycaemia is an unpleasant condition for the affected individual; the current definition of an episode includes severe cognitive impairment where the individual requires external assistance [5]. Possibly linked to this effect on the nervous system, several investigations have reported that episodes are associated with increased mortality [6,7,8,9]. Furthermore, severe hypoglycaemic episodes may lead to hospital admission/emergency room attendance. In a study of people with type 1 and type 2 diabetes, Heller et al. found that 12% of 536 individuals experienced severe hypoglycaemic episodes leading to a hospital/emergency room attendance of ≤24 h and 7% required hospital admission (>24 h) [10]. The healthcare cost associated with these admissions/attendances is high, especially, for people with type 2 diabetes [10, 11]. Therefore, severe hypoglycaemic episodes, especially, those that lead to hospitalisations, places a significant burden on patients and society. The primary risk factors for severe hypoglycaemic episodes are use of insulin, use of sulfonylurea, hypoglycaemia unawareness, high age and longer duration of diabetes [12,13,14,15,16].
In this study, our aim was to investigate the nationwide trends in incidence and associated risk factors, with focus on blood glucose-lowering medication, for the first hypoglycaemic episode leading to hospitalisations in Denmark among people with type 1 and 2 diabetes mellitus.
Methods
Study design
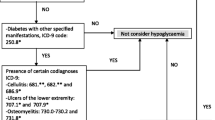
The study was designed as a cohort study with two cohorts of interest extracted from the Danish National Patient Registry. Cohort 1 consisted of all people diagnosed with diabetes in the period 1977–2018 and was used to analyse trends of all hypoglycaemic episodes leading to hospitalisation during the last two decades (i.e. 1998–2018). Cohort 2 consisted of people diagnosed with diabetes in 1998–2018 and was used to analyse risk factors for hypoglycaemic episodes leading to hospitalisation. The reason for restricting cohort 2 to the period 1998–2018 was that relevant medications were only available from 1996. Diabetes cases were identified as people who were admitted to hospital with a primary or secondary diabetes-related ICD-8 or ICD-10 (http://apps.who.int/classifications/icd10/browse/2016/en) system code of 249.XX, 250.XX, 647.74, 761.19, Y6449, E10.X, E11.X, E12.X, E13.X, E14.X, G63.2, H28.0, H36.0, M14.2, O24 or R73 or who had received medicine with an Anatomical Therapeutical Chemical (ATC) classification system code (https://www.whocc.no/atc/structure-and-principles/) of A10 (drugs used in diabetes). The first occurrence of one of the codes defined date of diagnosis. People treated with liraglutide for obesity (ATC A10BJ02) were excluded using the product name. Diabetes cases were further classified as type 1 diabetes if the individual had at least one ICD code of E10 (type 1 diabetes mellitus), at least one ATC code of A10A (insulins and analogues), and no ATC code of A10B (blood glucose-lowering drugs, excluding insulins). Otherwise, they were classified as having type 2 diabetes. Episodes of hypoglycaemia were identified in 1998–2018 from hospital admissions with a primary or secondary ICD-10 code of E159 (hypoglycaemic coma, unspecified), E160 (drug-induced hypoglycaemia without coma), E161 (other hypoglycaemia) or E162 (hypoglycaemia, unspecified) after diabetes diagnosis. These episodes leading to hospitalisation are hereafter denoted as ‘hypoglycaemic episodes’.
Medication was extracted and categorised based on ATC codes. Insulins were included as compounds (ATC level 5), whereas non-insulin glucose-lowering drugs (termed non-insulin antidiabetic drugs [NAIDs] by the WHO) were included in drug classes (ATC level 4) according to the WHO classification. Users of long-acting human insulin (ATC A10AE01) and the combination of insulin degludec and insulin aspart (ATC A10AD06) were excluded due to low numbers. Intermediate-acting isophane human insulin (ATC A10AC01) was categorised as long-acting for simplification of later comparisons. The medication groups, abbreviations and ATC codes are shown in Table 1. Anxiolytics (ATC N05B), antidepressants (ATC N06AA), opioids (ATC N02A), corticosteroids (ATC H02) and drugs used in alcohol dependence (ATC N07BB) were extracted for analyses as well. Women with polycystic ovarian syndrome are often treated with clomifene and metformin and, to avoid the inclusion of these, women who received clomifene (ATC G03GB02) before the age of 40 years were excluded.
Data sources
Diagnoses of diabetes, hypoglycaemia and concomitant illnesses were extracted from the Danish National Patient Registry. The registry was established in 1977 and initially covered information on inpatients in somatic wards. Since then it has been expanded and now includes information on all patients in Danish hospitals. The validity of registrations are in general very high [17,18,19]. Positive predictive values for diabetes-related codes have been reported to >90% on average [20]. Insulin use and concomitant medications were extracted from the National Pharmacological Database of the Danish Medicines Agency. This database is a nationwide register of medicines sold after 1996.
The study has ethics approval from Statistics Denmark to use human data from the Danish registries.
Statistical analyses
Descriptive statistics for cohorts 1 and 2 are presented as mean ± SD or number and percentage of people. Number of episodes are presented as the number of people with one episode, two episodes and more than two episodes. Late-diabetic complications, representing the diabetes severity in the cohorts, were reported as follows: nephropathy (ICD-10 code E102, E112), retinopathy (ICD-10 E103, E113), neuropathy (ICD-10 E104-5, E114-5), multiple (ICD-10 DE107, DE117, or more than one of the mentioned complications) and other (ICD-10 DE106, DE108, DE116, DE118).
Trends in incidence of all hypoglycaemic episodes over the last two decades (1998–2018) were investigated in cohort 1 descriptively as the number of hypoglycaemic episodes and rate of episodes per 100 person-years per calendar year plotted as time series. Furthermore, trends were analysed with Poisson regression models of number of hypoglycaemic episodes with year as a categorical independent variable and the loge of person-years of exposure as offset. The year of highest incidence rate was used as reference. Incidence rate ratios (IRRs) were calculated from the model coefficients. Finally, linear regression models of incidence rates with year as independent variable were applied to specific time periods to underpin trends, and the coefficients and model fits are presented. Dispensing of blood glucose-lowering medications over the two decades are also presented. Trends in incidence of hypoglycaemic episodes and glucose-lowering medication were stratified in type 1 and type 2 diabetes.
To investigate the risk factors of first-experienced hypoglycaemic episode leading to hospitalisation, two Cox proportional hazards models with time-varying covariates were constructed using cohort 2: one for people on insulin and one for people on NIADs. The first model (for insulin) included only people with type 1 diabetes, whereas the second model (for NIADs) included only people with type 2 diabetes. We chose not to include people with type 2 diabetes in the model for insulin, because this would make the patient group very heterogenous and the covariates difficult to interpret. In the first model, time from diabetes diagnosis to first hypoglycaemic episode was modelled as a function of age (0–19, 20–39, 40–49, 50–59, 60–69, 70–79, 80+ years), sex (female/male), diabetes duration (0–1, 2–4, 5–9, 10+ years), alcohol abuse (yes/no), and use of anxiolytics (yes/no), antidepressants (yes/no), opioids (yes/no), corticosteroids (yes/no) and the 12 insulin types (yes/no) shown in Table 1. In the second model, time from diabetes diagnosis to first hypoglycaemic episode was modelled as a function of age (0–39, 40–49, 50–59, 60–69, 70–79, 80+ years), sex (female/male), diabetes duration (0–1, 2–4, 5–9, 10+ years), alcohol abuse (yes/no), and use of anxiolytics (yes/no), antidepressants (yes/no), opioids (yes/no), corticosteroids (yes/no) and the nine NIAD classes (yes/no) shown in Table 1. The dichotomous insulin and NIAD variables were included as time-varying covariates and take the values of ‘Y’ and ‘N’ depending on whether the person took the specific medication in a specific period or not. The other time-dependent variables of age, diabetes duration and other medications were also included as time-varying covariates based on the periods defined by the changes in insulin or NIAD. People were censored at the first date of emigration, death or end of follow-up (31 December 2018).
The descriptive and inferential analyses were conducted in SAS 9.4 (TS1M5; SAS Institute, Cary, NC, USA). The significance level was set at a p value of less than 0.05 for two-sided testing.
Results
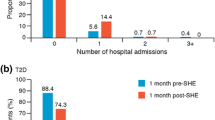
Data for 657,590 people with diabetes-related diagnoses or blood glucose-lowering medication codes in the period 1977–2018 were extracted; 13,581 women possibly with polycystic ovarian syndrome were excluded and 2607 people prescribed liraglutide for obesity were excluded. Cohort 1 consisted of 641,402 people and cohort 2 consisted of 425,200 people (characteristics are shown in Tables 2 and 3, respectively). People in cohort 1 experienced 66,438 hypoglycaemic episodes leading to hospitalisation, whereas people in cohort 2 experienced 19,351 episodes. Figure 1 shows the number and incidence rate of hypoglycaemic episodes during 1998–2018. The incidence rate for people with type 1 diabetes was approximately 8 episodes per 100 person-years in 1998. People with type 2 diabetes had a tenfold lower incidence rate of episodes compared with people with type 1 diabetes. In both series, a peak in incidence rate in 2003 was seen, with a consistent drop thereafter. From the Poisson regression model, the overall effect of year on the number of hypoglycaemic episodes was statistically significant for both type 1 diabetes (χ2 3808, df 20, p < 0.0001) and type 2 diabetes (χ2 2631, df 20, p < 0.0001). Table 4 shows the IRR for each year from the Poisson model. The incidence rate had dropped by 66% for type 1 diabetes (IRR 0.34 [95% CI 0.31, 0.36], p < 0.0001) and 61% for type 2 diabetes (IRR 0.39 [95% CI 0.36, 0.42], p < 0.0001) in 2018 compared with 2003. From linear regression models applied to the calculated crude incidence rates from 2003 to 2018, a decrease of 0.40 episodes per 100 person-years per calendar year for type 1 diabetes (R2 = 0.92, p < 0.0001) and 0.05 episodes per 100 person-years per calendar year for type 2 diabetes (R2 = 0.97, p < 0.0001) was derived.
Figure 2 shows the dispensed medicine during the two decades of follow-up stratified as insulins and NIADs. Human insulin (fast-acting and long-acting) was the primary insulin dispensed in 1998–2007. Around 2002–2004 a drop can be seen in the dispensing of human insulin probably due to the advent of the insulin analogues such as insulin glargine and insulin detemir. Dispensing of insulin degludec began in 2013, with a rapid growth after 2015. With respect to NIADs, sulfonylureas were the primary dispensed medicine from 1998 to 2003 and their use declined after 2008, whereas dispensing of metformin increased steadily from 1998 and plateaued around 2012. In 2007, glucagon-like peptide 1 receptor agonists (GLP-1-RAs) began to be dispensed and a rapid growth was seen in 2009. The remaining medications had a slower uptake.
Dispensing data for blood glucose-lowering medication during the 20 years of follow-up, showing the number of insulin prescriptions dispensed for type 1 diabetes (a) and the number of NIADs dispensed for type 2 diabetes (b). The black lines represent the number of people for whom the prescriptions were dispensed. AGIs, α-glucosidase inhibitors; Comb, combinations; T1D, type 1 diabetes; T2D, type 2 diabetes
Figures 3 and 4 show results from the Cox regression models presented as forest plots. In the model for insulins (n = 18,031, type 1 diabetes only), age was associated with a comparable decrease in risk of hypoglycaemic episodes in all age groups (except 80+ years) compared with 0–19 years. Female sex was associated with a 9% decrease in the risk of hypoglycaemic episodes. Results indicated that a longer diabetes duration is associated with an increase in the risk of hypoglycaemic episodes. Furthermore, alcohol abuse was associated with a 62% increase in risk of hypoglycaemic episodes. For the fast-acting insulins, human (fast) had the highest HR when compared with insulin lispro, aspart and glulisine, although the 95% CIs overlapped. For long-acting insulins, human (long) had the highest HR compared with insulin glargine, detemir and degludec, although 95% CIs overlapped. For the combination insulins, human (comb) had the highest HR compared with insulin lispro and lispro protamine, and insulin aspart and aspart protamine, although CIs overlapped. In general, treatment with human (long), glargine, detemir, human (comb) and a combination of insulin aspart and aspart protamine was associated with a statistically significant increase in risk of hypoglycaemic episodes. Treatment with insulin aspart was associated with a statistically significant decrease in risk of hypoglycaemic episodes. Finally, opioids and corticosteroid use was associated with a decrease in the risk of hypoglycaemic episodes, whereas anxiolytics and antidepressants were not associated with an effect.
Forest plot showing estimated HRs and 95% CIs for the effect of insulins on time to first hypoglycaemic episode for people with type 1 diabetes, adjusted for age, sex, diabetes duration, alcohol abuse and other medications. The estimates are shown on a logarithmic scale (log10). The reference group for age was 0–19 years, the reference for sex was male and the reference for diabetes duration was 0–1 years. Insulins, alcohol abuse and other medications were added as dichotomous yes/no variables to the model. Too few data were available to model the effect of human (long) and degludec and aspart
Forest plot showing estimated HRs and 95% CIs for the effect of NIADs on time to first hypoglycaemic episodes for people with type 2 diabetes, adjusted for age, sex, diabetes duration, alcohol abuse and other medications. The estimates are shown on a logarithmic scale (log10). The reference group for age was 0–39 years, the reference for sex was male and the reference for diabetes duration was 0–1 years. NIADs, alcohol abuse and other medications were added as dichotomous yes/no variables to the model. AGIs, α-glucosidase inhibitors
In the model for NIADs (n = 407,169), age was associated with an increase in risk of hypoglycaemic episodes with three- and fourfold increased risk for the 70–79 years and 80+ years group, respectively, compared with the 0–39 years age group. Female sex was associated with a 6% decrease in risk of hypoglycaemic episodes. Diabetes duration was associated with a comparable increase in risk of hypoglycaemic episodes for all duration groups compared with the 0–1 years group. Alcohol abuse was associated with a 2.3-fold increase in risk of hypoglycaemic episodes. For NIADs, sulfonylureas, α-glucosidase inhibitors and ‘other’ medications (e.g. repaglinide) were associated with an increased risk of hypoglycaemic episodes; notably sulfonylureas posed a 2.3-fold increase in risk. On the other hand, metformin, ‘combinations’ (such as metformin and sulfonylurea), dipeptidyl peptidase 4 inhibitors (DPP-4is), GLP-1-RAs and sodium–glucose cotransporter 2 inhibitors (SGLT2is) were associated with a decreased risk of hypoglycaemic episodes, and an approximately fivefold decrease in risk compared with sulfonylureas. Similarly to the model for insulins, in the model for NIADs, opioids and corticosteroids were associated with a decrease in the risk of hypoglycaemic episodes and anxiolytics were not associated with an alteration in the risk. However, in contrast to the model for insulins, antidepressants were associated with an 11% increase in risk of hypoglycaemic episodes.
Discussion
The incidence rate of hypoglycaemic events leading to hospitalisations has dropped by more than 60% for people with type 1 diabetes and people with type 2 diabetes since 2003 (a decrease of 0.4 and 0.05 episodes per 100 person-years per calendar since 2003, respectively). The estimated HRs from the Cox models indicate that new treatment alternatives, especially for NIADs for type 2 diabetes, may play a significant role in this decline in incidence rates. Sulfonylureas were the primary dispensed medication for type 2 diabetes until 2003, after which metformin was the primary dispensed medication. DDP-4is and GLP-1-RAs came onto the market in 2007 and SGLT2is in 2012 as second-line alternatives to sulfonylureas for the treatment of type 2 diabetes. From the results in this study, these medications seem much safer than sulfonylureas with respect to risk of hypoglycaemic episodes. In addition, insulin analogues seem safer than human insulins for the treatment of type 1 diabetes although CIs overlap. The insulin analogues glargine and detemir were introduced in 2004 and replaced human insulin for many patients; this timing corresponds to the observed decline in the incidence rate of hypoglycaemic episodes.
The rate of eight episodes per 100 person-years in 1998 for people with type 1 diabetes is approximately one-fifth that of the rate reported in the EDIC cohort [4], a fraction similar to that reported in an investigation by Heller et al. [10]. In 2018, the incidence rate for type 1 diabetes presented in our study more than halved (by four episodes per 100 person-years), whereas the rate in the EDIC cohort did not seem to drop over time. The reason for the drop in Denmark might be that the severity of the hypoglycaemic episodes had decreased (i.e. the number of severe hypoglycaemic episodes might be the same but the episodes might lead less frequently to hospital admissions). In a study by Lipska et al. [21], in 1999 the incidence rate in US hospital admissions for diabetes-related hypoglycaemic episodes was 0.68 per 100 person-years, with an increase in incidence rate until 2003 and a subsequent consistent decline, which corresponds to the incidence rate and trend for type 2 diabetes in our study. The incidence rates in Denmark changed more rapidly, which may be explained by several factors, such as changes in pre-hospital care of the patients and new stricter European Union (EU) legislation on driver’s licensing resulting in concealed severe hypoglycaemic episodes [22]. Moreover, the EDIC cohort contained self-reported severe hypoglycaemic episodes, which makes comparison with our results challenging.
In this study, the primary risk factor of duration of diabetes for severe hypoglycaemic episodes leading to hospitalisation was confirmed in the model of insulins, including people with type 1 diabetes only, where estimated HRs increase with increasing duration. It was only partly confirmed in the model of type 2 diabetes, where increments in diabetes duration were associated with increase in HR compared with the 0–1 years group only. Age was also associated with a large increase in HR for higher age intervals for type 2 diabetes. For type 1 diabetes all age groups except 80+ years were associated with reduced HRs compared with the 0–19 years group, which could indicate that especially children, adolescents and young adults are at risk of hypoglycaemic episodes. This is possibly due to difficulties handling a chronic disease for children and risk-taking behaviours for adolescents and young adults including alcohol use. In our study, use of human insulins (fast-acting, long-acting and combination insulins) was associated with higher HRs compared with insulin analogues, indicating decreased safety with respect to hypoglycaemic episodes, and this is confirmed by literature [23,24,25,26]. Use of sulfonylureas was associated with a 2.3-fold increased risk of hypoglycaemic episodes and was, together with α-glucosidase inhibitors and ‘other’ agents (e.g. repaglinide), associated with the highest risk of hypoglycaemic episodes. The high risk of hypoglycaemic episodes associated with sulfonylureas is confirmed in other studies but varies across compounds [15, 27].
The Danish National Patient Registry does not include information on hypoglycaemia awareness, and its association with hypoglycaemic episodes leading to hospitalisation was not explored in this study. A limitation is that women with gestational diabetes were included in the cohort. However, exclusion of these women would result in exclusion of the population of interest as they are predisposed to type 2 diabetes (up to 50% [28]) and may only have the pregnancy as hospital contact if they are well controlled. However, the trends in hypoglycaemic episodes and the risk factors are still deemed valid despite the inclusion of these women in our study. Another limitation is that women with polycystic ovarian syndrome only treated with metformin were included, although we believe this noise is acceptable in light of the >400,000 included people with type 2 diabetes. A further limitation in this study is that only hypoglycaemic episodes leading to hospitalisations were investigated and these constitute only one-fifth of severe hypoglycaemic episodes [10]. Another issue is the lack of information on glycaemic control. Some medications seem safer with respect to hypoglycaemic episodes in this study but if the patients on these medications have a less tight glycaemic control the safety may come at the expense of increased risk of late-diabetic complications. Furthermore, patients’ self-management might improve with age, and glycaemic targets are probably less stringent. A limitation is that we only analysed time to the first hypoglycaemic episode and not recurrent episodes. Given that 2.9% of the individuals with type 1 diabetes and 0.2% with type 2 diabetes experienced more than two hypoglycaemic episodes (Table 3), risk factor analysis on the recurrent episodes could have been applied. However, we wanted to know what the risk factors were for the first hypoglycaemic episode leading to hospitalisation and concluded that analysis of recurrent episodes would be more suitable for another investigation and was out of the scope of this study. Moreover, we believe that adding recurrent episodes could introduce noise and confounding by indication bias would probably increase as both the practitioner and the patient try to avoid future severe episodes. Finally, new technological improvements in the form of insulin pumps and continuous glucose monitoring might also have improved treatment.
A strength of this study is the magnitude of data included. We have included data from more than 640,000 Danish people with diabetes. Furthermore, the quality of data is high due to the validity of the registries and since the primary diagnosis codes of E159–162 are in most cases probably not selected by coincidence.
In conclusion, the incidence rate of hypoglycaemic episodes leading to hospitalisations in Denmark has declined by more than 60% since 2003 for both type 1 and type 2 diabetes. Based on results in this study, the advent of new treatment alternatives, such as, insulin glargine, insulin detemir and insulin degludec compared with human insulins, and especially SGLT2is, GLP-1-RAs and DPP-4is compared with sulfonylureas, may contribute to this decline. From a safety perspective, these findings are important and should be considered by clinicians when assessing treatment options for patients who are still treated with older blood glucose-lowering medications. Other factors, such as improved diabetes technology, care of the patients, and less stringent glycaemic goals for some patient groups, may also play a significant role in reducing the incidence rate of hypoglycaemic episodes leading to hospitalisation.
Abbreviations
- ATC:
-
Anatomical Therapeutical Chemical
- DPP-4i:
-
Dipeptidyl peptidase 4 inhibitor
- GLP-1-RA:
-
Glucagon-like peptide 1 receptor agonist
- IRR:
-
Incidence rate ratio
- NIAD:
-
Non-insulin glucose-lowering drug
- SGLT2i:
-
Sodium–glucose cotransporter 2 inhibitor
References
Selvin E, Parrinello CM, Daya N, Bergenstal RM (2016) Trends in insulin use and diabetes control in the U.S.: 1988-1994 and 1999-2012. Diabetes Care 39(3):e33–e35. https://doi.org/10.2337/dc15-2229
American Diabetes Association (2018) ADA standards of medical care in diabetes 2018. Diabetes Care 41(1):S55–S64
Rogers DG (1994) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. Clin Pediatr (Phila) 33(6):378
Gubitosi-Klug RA, Braffett BH, White NH et al (2017) Risk of severe hypoglycemia in type 1 diabetes over 30 years of follow-up in the DCCT/EDIC study. Diabetes Care 40:1010–1016. https://doi.org/10.2337/dc16-2723
American Diabetes Association (2019) 6. Glycemic targets: standards of medical care in diabetes - 2019. Diabetes Care 42(January):S61–S70
McCoy R, Van Houten H, Ziegenfuss J, Shah N, Wermers R, Smith S (2012) Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care 35(9):1897–1901. https://doi.org/10.2337/dc11-2054
Zoungas S, Patel A, Chalmers J et al (2010) Severe hypoglycemia and risks of vascular events and death. N Engl J Med 363(15):1410–1418. https://doi.org/10.1056/NEJMoa1003795
Zaccardi F, Dhalwani NN, Webb DR, Davies MJ, Khunti K (2018) Global burden of hypoglycaemia-related mortality in 109 countries, from 2000 to 2014: an analysis of death certificates. Diabetologia 61(7):1592–1602. https://doi.org/10.1007/s00125-018-4626-y
Jensen MH, Dethlefsen C, Hejlesen O, Vestergaard P (2019) Association of severe hypoglycemia with mortality for people with diabetes mellitus during a 20-year follow-up in Denmark: a cohort study. Acta Diabetol 57(5):549–558
Heller SR, Frier BM, Hersløv ML, Gundgaard J, Gough SCL (2016) Severe hypoglycaemia in adults with insulin-treated diabetes: impact on healthcare resources. Diabet Med 33(4):471–477. https://doi.org/10.1111/dme.12844
Pedersen-Bjergaard U, Kristensen PL, Nørgaard K et al (2016) Short-term cost-effectiveness of insulin detemir and insulin aspart in people with type 1 diabetes who are prone to recurrent severe hypoglycemia. Curr Med Res Opin 32(10):1719–1725. https://doi.org/10.1080/03007995.2016.1205006
Oyer DS (2013) The science of hypoglycemia in patients with diabetes. Curr Diabetes Rev 9:195–208. https://doi.org/10.2174/15733998113099990059
Morales J, Schneiderb D (2014) Hypoglycemia. Am J Med 127:17–24
Van Dalem J, Brouwers MCGJ, Stehouwer CDA et al (2016) Risk of hypoglycaemia in users of sulphonylureas compared with metformin in relation to renal function and sulphonylurea metabolite group: population based cohort study. BMJ 354:1–8
Jensen MH, Kjolby M, Hejlesen O, Jakobsen PE, Vestergaard P (2020) Risk of major adverse cardiovascular events, severe hypoglycemia, and all-cause mortality for widely used antihyperglycemic dual and triple therapies for type 2 diabetes management: a cohort study of all Danish users. Diabetes Care 43(6):1209–1218. https://doi.org/10.2337/dc19-2535
Pedersen-Bjergaard U, Pramming S, Heller SR et al (2004) Severe hypoglycaemia in 1076 adult patients with type 1 diabetes: influence of risk markerts and selection. Diabetes Metab Res Rev 20(6):479–486. https://doi.org/10.1002/dmrr.482
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish national patient register. Scand J Public Health 39(7):30–33
Mosbech J, Jørgensen J, Madsen M, Rostgaard K, Thornberg K, Poulsen T (1995) The national patient registry. Evaluation of data quality. Ugeskr Laeger 157(26):3741–3745
Vestergaard P, Mosekilde L (2002) Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nationwide follow-up study of 16,416 patients in Denmark. Am J Epidemiol 156(1):8–10
Schmidt M, Alba S, Schmidt J, Sandegaard JL, Ehrenstein V, Pedersen L, Toft Sørensen H (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490. https://doi.org/10.2147/CLEP.S91125
Lipska KJ, Ross JS, Wang Y et al (2014) National trends in US hospital admissions for hyperglycemia and hypoglycemia among medicare beneficiaries, 1999 to 2011. JAMA Intern Med 174(7):1116–1124. https://doi.org/10.1001/jamainternmed.2014.1824
Pedersen-Bjergaard U, Færch L, Allingbjerg ML, Agesen R, Thorsteinsson B (2015) The influence of new European Union driver’s license legislation on reporting of severe hypoglycemia by patients with type 1 diabetes. Diabetes Care 38(1):29–33
Monami M, Marchionni N, Mannucci E (2009) Long-acting insulin analogues vs. NPH human insulin in type 1 diabetes. A meta-analysis. Diabetes Obes Metab 11(4):372–378. https://doi.org/10.1111/j.1463-1326.2008.00976.x
Monami M, Marchionni N, Mannucci E (2008) Long-acting insulin analogues versus NPH human insulin in type 2 diabetes. A meta-analysis. Diabetes Res Clin Pract 81(2):184–189. https://doi.org/10.1016/j.diabres.2008.04.007
Jensen MH, Hejlesen O, Vestergaard P (2020) Association of insulin regimens with severe hypoglycaemia in patients with type 1 diabetes: a Danish case–control study. Br J Clin Pharmacol 86(8):1560–1566. https://doi.org/10.1111/bcp.14263
Kristensen PL, Tarnow L, Bay C et al (2017) Comparing effects of insulin analogues and human insulin on nocturnal glycaemia in hypoglycaemia-prone people with type 1 diabetes. Diabet Med 34:625–631. https://doi.org/10.1111/dme.13317
Andersen SE, Christensen M (2016) Hypoglycaemia when adding sulphonylurea to metformin: a systematic review and network meta-analysis. Br J Clin Pharmacol 82:1291–1302. https://doi.org/10.1111/bcp.13059
Auvinen AM, Luiro K, Jokelainen J et al (2020) Type 1 and type 2 diabetes after gestational diabetes: a 23 year cohort study. Diabetologia 63(10):2123–2128. https://doi.org/10.1007/s00125-020-05215-3
Statistics Denmark. Danish National Patient Registry [Internet]. Statistics Denmark. 2019. Available from: https://www.dst.dk/en/. Accessed 27 May 2021
Authors’ relationships and activities
MHJ is a former employee at Novo Nordisk and holds shares in Novo Nordisk. PV has received unrestricted grants from Merck Sharp & Dohme and Servier and travel grants from Amgen, Eli Lilly and Company, Novartis, Sanofi-Aventis and Servier. OH declares that there are no relationships or activities that might bias, or be perceived to bias, his work.
Author information
Authors and Affiliations
Contributions
MHJ designed the study, carried out the analysis and wrote and approved the manuscript. OH and PV contributed to the design of the study and analysis of data and reviewed, edited and approved the manuscript. MHJ is responsible for the integrity of the work as a whole.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jensen, M.H., Hejlesen, O. & Vestergaard, P. Epidemiology of hypoglycaemic episodes leading to hospitalisations in Denmark in 1998–2018. Diabetologia 64, 2193–2203 (2021). https://doi.org/10.1007/s00125-021-05507-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-021-05507-2