Abstract
Aims/hypothesis
Women with gestational diabetes mellitus (GDM) and obesity experience lower rates of breastfeeding. Little is known about breastfeeding among mothers with type 2 diabetes. Australian Indigenous women have a high prevalence of type 2 diabetes in pregnancy. We aimed to evaluate the association of hyperglycaemia, including type 2 diabetes, with breastfeeding outcomes.
Methods
Indigenous (n = 495) and non-Indigenous (n = 555) participants of the Pregnancy And Neonatal Diabetes Outcomes in Remote Australia (PANDORA) cohort included women without hyperglycaemia in pregnancy (n = 222), with GDM (n = 684) and with type 2 diabetes (n = 144). The associations of hyperglycaemia in pregnancy and breastfeeding at hospital discharge, 6 weeks and 6 months post-partum were evaluated with logistic regression, after adjustment for maternal obesity, ethnicity, maternal and neonatal characteristics.
Results
Indigenous women were more likely to predominantly breastfeed at 6 weeks across all levels of hyperglycaemia. Compared with women with no hyperglycaemia in pregnancy, women with type 2 diabetes had lower odds for exclusive breastfeeding at discharge (adjusted OR for exclusive breastfeeding 0.4 [95% CI 0.2, 0.8] p = 0.006). At 6 weeks and 6 months, the relationship between type 2 diabetes and predominant breastfeeding was not statistically significant (6 weeks 0.7 [0.3, 1.6] p = 0.40, 6 months 0.8 [0.4, 1.6] p = 0.60). Women with gestational diabetes were as likely to achieve predominant breastfeeding at 6 weeks and 6 months as women without hyperglycaemia in pregnancy.
Conclusions/interpretation
Indigenous women had high rates of breastfeeding. Women with type 2 diabetes had difficulty establishing exclusive breastfeeding at hospital discharge. Further research is needed to assess the impact on long-term breastfeeding outcomes.

Graphical abstract
Similar content being viewed by others

Introduction
Breastfeeding has multiple benefits for women, children and the community. Women have a reduced risk of cancers and improved metabolic health, while for children, reduced risk of infection, allergy and adiposity are recognised benefits [1]. Exclusive breastfeeding for 6 months is recommended by WHO to optimise these benefits [2], and is associated with a reduced risk of overweight and obesity in early childhood and adulthood among those born to mothers with gestational diabetes mellitus (GDM) [3]. Additionally, longer duration of breastfeeding may have further benefits for obesity prevention [4, 5].
Despite the protective effect of breastfeeding, women with GDM or pre-existing diabetes requiring insulin may have lower rates of breastfeeding initiation [6] than those without hyperglycaemia in pregnancy. Women who are overweight or obese may also have lower rates of breastfeeding initiation [7, 8], with a possible additive impact for women with GDM [9]. Hyperglycaemia may delay lactogenesis. Delayed lactogenesis is also associated with Caesarean section, and use of artificial feeds, both of which are more commonly experienced in women with hyperglycaemia in pregnancy [10]. Most data relating to breastfeeding in hyperglycaemia in pregnancy relate to GDM, and data relating to breastfeeding initiation for infants born to mothers with pre-existing type 2 diabetes in pregnancy are limited. Some evidence indicates that women with pre-existing diabetes before pregnancy (type 1 or type 2), and those requiring insulin during pregnancy, have lower rates of breastfeeding initiation compared with those without hyperglycaemia in pregnancy. However, studies are based on birth discharge data or clinical audits and did not distinguish between type 2 diabetes and type 1 diabetes [6, 11]. Another small study of 30 women with type 2 diabetes reported reduced breastfeeding initiation in women with type 2 diabetes compared with those with GDM [12], suggesting that more severe hyperglycaemia may present greater challenges for breastfeeding. Longer term breastfeeding outcomes have not been evaluated in women with pre-existing type 2 diabetes in pregnancy.
Cultural practices, support from a partner and social determinants of health may also influence a woman’s choice or ability to breastfeed [13, 14]. First Nations women from many countries have high rates of hyperglycaemia in pregnancy [15]. Historically, Indigenous women in Australia had high rates of breastfeeding, with breastfeeding continuing for at least 2 years [16,17,18]. However, there appears to be variation in current breastfeeding practice for Australian Aboriginal women, largely depending on location of residence and potentially influenced by social factors and connection to traditional culture [19, 20]. Lower rates of breastfeeding in Aboriginal women compared with non-Indigenous women are reported in urban and regional areas [21,22,23]. Reduced breastfeeding initiation is also reported in Canadian and American First Nations mothers [24, 25]. Further evaluation is needed regarding the factors associated with successful continuation of breastfeeding for Australian Aboriginal mothers and First Nations mothers around the world, particularly those with hyperglycaemia in pregnancy.
We hypothesised that increasing levels of hyperglycaemia, particularly maternal pre-existing type 2 diabetes, would be associated with greater difficulty breastfeeding at all time points. We aimed to evaluate the associations of pre-existing type 2 diabetes in pregnancy and GDM, compared with no hyperglycaemia, with exclusive breastfeeding at hospital discharge and predominant breastfeeding at 6 weeks and 6 months in Indigenous and non-Indigenous women, adjusting for maternal and neonatal factors including maternal obesity.
Methods
Design and setting
The Pregnancy And Neonatal Diabetes Outcomes in Remote Australia (PANDORA) study is a longitudinal birth cohort study established to assess outcomes for women with hyperglycaemia in pregnancy and their offspring. The study is based in the Northern Territory (NT) of Australia, a sparsely populated region, where 33% of babies are born to Indigenous mothers who experience high rates of hyperglycaemia, and remoteness [26]. Informed consent was obtained, using interpreters if necessary. The study was approved by the joint Menzies School of Health Research/Northern Territory Department of Health, Human Research Ethics Committee, including the Aboriginal sub-committee and the Central Australian Human Research Ethics Committee.
Data collection
Women with hyperglycaemia in pregnancy were referred to the Northern Territory Diabetes in Pregnancy (NT DIP) clinical register and then invited to participate in PANDORA. To summarise previously published detail, from November 2011 to February 2017, antepartum, peripartum and demographic information were collected for 1170 neonates and their mothers. A non-random convenience sample of women without hyperglycaemia in pregnancy (with normal 75 g OGTT) were recruited from antenatal clinics for the PANDORA study and were similar to women in the NT Midwives Data Collection (a population-based census of all NT births) in 2013 with regard to age and geographic location [27]. Women were then followed up with direct contact at intervals post-birth (6 weeks, 6 months and 24 months). For this analysis, the following infants were excluded: (1) intrauterine fetal death, stillbirth, neonatal or infant death prior to 8 months (n = 10); (2) born to mothers with type 1 diabetes (n = 19); (3) born at less than 34 weeks gestation (given reduced ability to suck feed at this gestational age) (n = 26); (4) born to a multiple pregnancy (n = 32); (5) sibling of previous participant (to ensure unique mother–infant pairs were assessed) (n = 12); or (6) declined follow-up after birth or withdrew from study prior to 12 months post-partum (n = 21) (see electronic supplementary material [ESM] Fig. 1). Thus, 1050 mother and infant pairs were evaluated (ESM Fig. 1).
Maternal measures
Maternal hyperglycaemia in pregnancy was determined from a 75 g OGTT, HbA1c performed in pregnancy, or medical records to confirm previously diagnosed type 2 diabetes. Women were classified as having GDM based on OGTT results consistent with criteria used during recruitment which included: (1) the 1999 Australasian Diabetes in Pregnancy Society guidelines (from 2011 until 2012) [28]; and (2) WHO and International Association of the Diabetes and Pregnancy Study Groups guidelines (from 2012 until 2014) [29]. Pre-existing type 2 diabetes was determined if diagnosed prior to pregnancy and confirmed in medical records. Women with GDM were diagnosed at a median of 28 weeks' gestation by OGTT. Women who had OGTT or HbA1c results consistent with type 2 diabetes criteria outside of pregnancy were included in the GDM group for the primary analysis which is consistent with guidelines regarding diagnosis of GDM in pregnancy. For these women, diagnosis by OGTT occurred at a median of 27 weeks' gestation and diagnosis by HbA1c occurred at a median of 18 weeks' gestation. Maternal obesity was assessed using BMI (calculated from first measured weight and height and adjusted for weeks of gestation at measurement) and defined if the BMI was ≥30 kg/m2. Maternal ethnicity was determined by self-report. Indigenous women were those who identified as Aboriginal, Torres Strait Islander or Aboriginal and Torres Strait Islander. Smoking in pregnancy was determined by self-report; remote (vs urban) locality of residence was determined by the Australian Bureau of Statistics Remoteness Area [30]; and maternal education attainment by completion of 12 years or post-school qualifications vs <12 years of schooling. Nulliparity, mode of delivery (Caesarean section vs vaginal delivery) and instrumental delivery were determined from medical records.
Neonatal measures
Gestational age (in weeks) was determined from the ultrasound assessment recorded in the mother’s medical record. Admission to the neonatal nursery was defined as formal admission to the neonatal nursery including special care or neonatal intensive care unit requiring separation from the mother. Neonatal hypoglycaemia was defined as any recorded blood glucose level less than 2.6 mmol/l, irrespective of whether this required management with i.v. dextrose.
Breastfeeding at hospital discharge
Data on breastfeeding at hospital discharge were obtained from direct questioning of mothers by the research team at the postnatal assessment within 72 h of birth, often on day of discharge. The outcome was exclusive breastfeeding. Exclusive breastfeeding was defined as only human milk being given to the infant since birth.
Breastfeeding at 6 weeks and 6 months
Direct contact either by telephone or email was attempted with all women at 6 to 8 weeks post-partum for the 6 week follow-up, and again at 6 to 8 months for the 6 month follow-up, with the same survey on breastfeeding administered by phone or online. In those for whom direct contact could not be established, data on breastfeeding were obtained through data linkage to electronic medical records of primary healthcare at 4–10 weeks post-partum for the 6 week follow-up (200 women) and between 4 and 7 months post-partum for the 6 month follow-up (183 women). The ‘Healthy Under 5’ schedule guides assessment for infants in remote communities at 4 weeks, 8 weeks, 4 months and 6 months [31]. Standardised questions are asked of caregivers at these time points regarding breastmilk intake, breastfeeding and use of infant formula. If data were obtained from both sources, data from direct contact were used preferentially. Concordance between data obtained from both sources was evaluated for a subset of participants. Predominant breastfeeding was defined as an infant being fed human milk as the only form of milk (until 6 weeks of age or at least 5 months of age for the two time points) consistent with the WHO definition [32], which allows oral intake of water and is consistent with the mother’s report of ‘full breastfeeding’. Detail regarding exclusive breastfeeding was missing from the electronic medical record and hence could not be reported. Outcomes at 6 weeks and 6 months are discrete with no influence of previous breastfeeding outcomes.
Statistical analysis
Differences in maternal and neonatal characteristics by ethnicity within each of the maternal glycaemic status groups were assessed. Continuous variables were analysed using unpaired two sample t tests for normally distributed data and the Wilcoxon rank sum test for non-normally distributed data (maternal BMI). Pearson’s χ2 test was used for categorical variables. A p value of <0.05 was considered statistically significant. Logistic regression models were developed to assess the association of GDM and pre-existing type 2 diabetes compared with no hyperglycaemia in pregnancy with breastfeeding outcomes at birth, 6 weeks and 6 months. Univariate analysis was performed for the following covariates: ethnicity, nulliparity, BMI/obesity, smoking, instrumental delivery, Caesarean section, admission to neonatal nursery, neonatal hypoglycaemia, maternal education, and location of residence. Multivariable models were separately developed to evaluate the influence of covariates, particularly maternal obesity and Indigenous ethnicity, on the association between breastfeeding outcomes and maternal hyperglycaemia. Initially models were adjusted for maternal age, neonatal sex and gestational age at birth, and these variables were included in all multivariable models. Model 2 also adjusted for demographic factors significantly associated with breastfeeding (p < 0.1 on univariable analysis); model 3 adjusted for factors in model 2 plus maternal, birth and neonatal factors (p < 0.1 on univariable analysis); model 4 additionally adjusted for maternal obesity; and model 5 additionally adjusted for ethnicity. Models were developed using participants with complete data for each variable in the final model.
Tests for interactions between maternal hyperglycaemia and ethnicity, and hyperglycaemia and maternal obesity, were performed using the Wald test. Sensitivity analyses were undertaken: (1) obesity replaced with BMI as a continuous variable; (2) stratification by neonatal hypoglycaemia (to assess the influence of early management of neonatal hypoglycaemia including provision of infant formula on relationships between maternal hyperglycaemia and breastfeeding outcomes); and (3) maternal hyperglycaemia categories redefined according to insulin use, with no hyperglycaemia in pregnancy remaining the referent, to further assess the impact of severity of hyperglycaemia. Concordance between the two sources of breastfeeding data was evaluated by assessment of the proportion of matched outcomes from the two data sources. Statistical analysis was performed using Stata version 15 (Stata Corporation, College Station, TX, USA).
Results
Maternal and neonatal characteristics
Indigenous women were younger and more likely to smoke than non-Indigenous women. Indigenous women were less likely to have 12 years of education, and more likely to live in a remote area than non-Indigenous women irrespective of glycaemic status (Table 1). Indigenous women with GDM had a higher BMI than non-Indigenous women with GDM, whereas Indigenous women without hyperglycaemia in pregnancy had a lower BMI than non-Indigenous women without hyperglycaemia in pregnancy. Offspring of Indigenous mothers with GDM were more likely to have admission to the neonatal nursery than non-Indigenous offspring of mothers with GDM. At 6 weeks and 6 months, women followed up by electronic record only were more likely to be Indigenous, of younger age and have type 2 diabetes than those followed up by survey alone (ESM Tables 1,2).
Breastfeeding outcomes – proportions in Indigenous and non-Indigenous women across the glycaemic spectrum
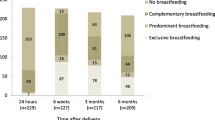
When comparing Indigenous to non-Indigenous women, the proportions exclusively breastfeeding at hospital discharge were similar in those with GDM (77% vs 75%) and in those without hyperglycaemia in pregnancy (85% vs 84%), respectively (Table 2). Among those with pre-existing type 2 diabetes, Indigenous women were more likely to exclusively breastfeed on discharge compared with non-Indigenous women (52% vs 29%, p = 0.047).
At 6 weeks, Indigenous women across the glycaemic spectrum were more likely to predominantly breastfeed than non-Indigenous women (no hyperglycaemia in pregnancy 82% vs 66%, p = 0.02; GDM 81% vs 57%, p < 0.001 and type 2 diabetes 61% vs 33%, p = 0.03). At 6 months, Indigenous women with GDM were more likely to predominantly breastfeed than non-Indigenous women (68% vs 46%, p < 0.001). However, at 6 months, there was no significant difference in predominant breastfeeding between Indigenous and non-Indigenous women with pre-existing type 2 diabetes in pregnancy (58% vs 40%, p = 0.20), or for women without hyperglycaemia in pregnancy (71% vs 60%, p = 0.13).
Age and sex adjusted associations between maternal hyperglycaemia in pregnancy and breastfeeding outcomes for Indigenous and non-Indigenous women
Indigenous and non-Indigenous women with GDM, compared with women without hyperglycaemia in pregnancy, were as likely to achieve exclusive breastfeeding, predominant breastfeeding at 6 weeks or 6 months, after adjustment for maternal age, gestational age and neonatal sex (Table 2). Indigenous and non-Indigenous women with pre-existing type 2 diabetes were significantly less likely to exclusively breastfeed at hospital discharge, compared with those without hyperglycaemia in pregnancy. Pre-existing type 2 diabetes was associated with an OR less than 1 for all other breastfeeding outcomes, however, confidence intervals were wide and included 1 (Table 2). There were no significant interactions between Indigenous status and glycaemic status or between obesity and glycaemic status for all breastfeeding outcomes (data not shown). As such, data from Indigenous and non-Indigenous women were considered together in subsequent multivariable models.
Multivariable models
Exclusive breastfeeding at hospital discharge
Figure 1 outlines multivariable models, showing that Indigenous ethnicity and greater gestational age were associated with greater odds of exclusive breastfeeding at hospital discharge, and pre-existing type 2 diabetes, Caesarean birth and admission to the neonatal nursery were associated with lower odds of exclusive breastfeeding at hospital discharge. Model building (ESM Table 3) demonstrates that type 2 diabetes remained associated with lower odds of exclusive breastfeeding at hospital discharge after adjusting for maternal obesity and neonatal/delivery factors.
Multivariable model of breastfeeding outcomes. (a) Exclusive breastfeeding on hospital discharge (n = 984). (b) Predominant breastfeeding at 6 weeks (n = 504). (c) Predominant breastfeeding at 6 months (n = 722). The models include maternal ethnicity, maternal GDM/type 2 diabetes (T2D) status, gestational age at birth, maternal age, and covariates significantly associated with the outcome on univariable analysis
Predominant breastfeeding at 6 weeks and 6 months
Women with GDM were as likely to predominantly breastfeed at 6 weeks and 6 months compared with women with no hyperglycaemia in pregnancy after adjusting for important covariates (ESM Table 3). Pre-existing type 2 diabetes was associated with lower odds of predominant breastfeeding at 6 weeks and 6 months, but confidence intervals were wide and include unity. Adjusting models for maternal obesity further attenuated associations between type 2 diabetes and breastfeeding (ESM Table 3). In the final multivariable model at 6 weeks (Fig. 1), Indigenous ethnicity and remote residence were associated with greater odds of predominantly breastfeeding, whereas maternal obesity was associated with lower odds of predominantly breastfeeding. These variables were also associated with predominant breastfeeding at 6 months, with the addition that women who delivered via Caesarean section were less likely to predominantly breastfeed.
Sensitivity testing
The strength of the associations between maternal hyperglycaemia and breastfeeding outcomes remained similar when maternal obesity was replaced with BMI measured on a continuous scale and when analyses were repeated among those neonates with and without neonatal hypoglycaemia (data not shown). Categorisation of maternal hyperglycaemia by insulin use attenuated results, with ORs closer to 1.0 for all breastfeeding outcomes (data not shown). Concordance of results between two data sources (direct contact and electronic medical record) for breastfeeding data was adequate with agreement between data sources in 86% (n = 83/96) of women at 6 weeks and 96% (n = 73/76) at 6 months.
Discussion
This study reports four major findings in this population of women and infants. First, Indigenous women had high rates of breastfeeding at hospital discharge and were more likely to predominantly breastfeed at 6 weeks and at 6 months than non-Indigenous women across the spectrum of glucose tolerance. Second, independent of maternal obesity and birth factors, women with pre-existing type 2 diabetes were less likely to exclusively breastfeed at discharge. Third, women with GDM were as likely to breastfeed at discharge and at follow-up compared with women without hyperglycaemia in pregnancy. Finally, there was a strong association between maternal obesity in pregnancy and reduced breastfeeding.
In our study, Indigenous women achieved high rates of breastfeeding at hospital discharge and predominant breastfeeding to 6 months. Australian Aboriginal women have historically had high rates of breastfeeding, however recent studies involving Aboriginal women around Australia suggest that breastfeeding practices have changed. In urban populations of Australian Aboriginal women, lower rates of predominant breastfeeding at hospital discharge have been reported compared with non-Indigenous women [21, 22, 33]. In an urban population in Western Australia, only 43.8% of infants were exclusively breastfed at 6–12 weeks, in contrast to historical reports of sustained breastfeeding as part of the pre-colonial diet for Aboriginal infants [16, 34]. In a retrospective cohort study, predominant breastfeeding in hospital was reduced in Indigenous women with GDM, compared with non-Indigenous women with GDM [35]. Our study reports high rates of breastfeeding in Indigenous women, many of whom have experienced hyperglycaemia in pregnancy. Additionally, remote residence was associated with successful predominant breastfeeding at 6 weeks and 6 months. Greater residential isolation was similarly found to be protective in a cross-sectional survey in Aboriginal infants in Western Australia [23]. Exploration of the impact of cultural and family connection associated with remoteness would be vital in the context of understanding the high rates of breastfeeding for Aboriginal women. Across multiple countries, First Nations women are reported to have reduced rates of breastfeeding compared with non-First Nations women [24, 25, 36]. Several studies have demonstrated a reduced risk of diabetes in First Nations women who breastfeed and their offspring [24, 37], however, research has yet to determine factors that support these women to breastfeed. Additionally, until now, there has been little research into the impact of maternal obesity and severity of hyperglycaemia on continuation of breastfeeding in this population.
Our study reports that women with pre-existing type 2 diabetes, compared with those without hyperglycaemia in pregnancy, were less likely to establish exclusive breastfeeding at hospital discharge, irrespective of maternal, birth or neonatal factors. There are few studies evaluating the impact of pre-existing maternal type 2 diabetes on success of exclusive breastfeeding at hospital discharge, particularly taking into consideration complex deliveries. One cross-sectional study reported that delayed lactogenesis was more likely in women with GDM requiring insulin during pregnancy [38] suggesting that severity of hyperglycaemia in pregnancy may impact the ability to establish early breastfeeding. Another cross-sectional study reported reduced breastfeeding initiation in women with pre-gestational diabetes (which included type 1 and type 2 diabetes) compared with women without hyperglycaemia in pregnancy [11], however this study did not adjust for potential confounders such as maternal BMI, education or delivery mode.
In our study, at 6 weeks and 6 months, women with GDM were as likely as women without hyperglycaemia in pregnancy to achieve predominant breastfeeding. Although women with pre-existing type 2 diabetes were less likely to achieve predominant breastfeeding, we did not observe a significant association in our study. The relationship between type 2 diabetes and long-term predominant breastfeeding was attenuated by maternal obesity, which was independently associated with reduced long-term predominant breastfeeding. A survey study including 17 women with type 2 diabetes reported that 64% of these women achieved any breastfeeding at 3 months, however no comparison was made across the glycaemic spectrum [39]. No other studies have evaluated breastfeeding beyond 3 months in women with type 2 diabetes. Multiple studies have reported an association between maternal obesity and reduced success in breastfeeding initiation and continuation in the general population [8], however few studies have evaluated the relationship between obesity and hyperglycaemia in pregnancy and their impact on breastfeeding success. One study reported an additive interaction between maternal pre-pregnancy obesity and GDM on delayed breastfeeding initiation [9], while another reported that women who were overweight with GDM were equally likely to breastfeed compared with those of normal weight [40]. Matias et al. reported maternal obesity to be a key factor associated with delayed lactogenesis in women with GDM [38]. Our finding contrasts with previously published findings regarding breastfeeding in women with GDM. We propose that the high rates of breastfeeding in Indigenous women, with remote residence as a further protective factor, may have contributed to our findings. Furthermore, women with GDM may receive additional postnatal support to breastfeed.
Strengths of our study include that it is a large prospective birth cohort with detailed evaluation of maternal and neonatal variables at birth. This cohort represents a unique population, enabling evaluation of factors associated with breastfeeding success in a population with high risk for maternal and offspring type 2 diabetes. The following limitations of this study should be considered. First, loss to follow-up at 6 weeks and 6 months may have affected the representativeness of the cohort, however, the study population at follow-up was representative of the larger baseline cohort in terms of maternal and neonatal factors. Nevertheless, loss to follow-up likely reduced statistical power leading to some uncertainty about the associations between type 2 diabetes and predominant breastfeeding observed at later time points. Additionally, as the study sample size was not calculated for the purpose of addressing differences in breastfeeding outcomes, it may have been underpowered for some of the comparisons presented. Second, information on breastfeeding was more likely to be obtained from the electronic medical record for Indigenous women than non-Indigenous women. Findings from the electronic medical record relied on the interpretation and recording of breastfeeding behaviours by healthcare providers which may contain inaccuracies, however, concordance between the two methods of data collection was high at both 6 weeks and 6 months with data from both sources resulting in similar findings. Nevertheless, we acknowledge that reporting bias may persist and could provide an explanation for the failure to find a strong association between hyperglycaemia and breastfeeding. Third, women with hyperglycaemia in pregnancy may be more likely to report breastfeeding, particularly if they received breastfeeding education regarding potential benefits. Lastly, this is an observational study and, as such, unmeasured confounding may have influenced findings.
Our study showed that women with pre-existing type 2 diabetes in pregnancy had greater risk of not exclusively breastfeeding at hospital discharge, however the association of type 2 diabetes in pregnancy and predominant breastfeeding at 6 weeks and 6 months after birth was inconclusive. To some extent the association between type 2 diabetes and predominant breastfeeding was attenuated by maternal obesity, although the smaller number of women with pre-existing type 2 diabetes in pregnancy in the study likely contribute to uncertainty regarding this relationship. Increased breastfeeding support practices and awareness of in-hospital challenges for women with type 2 diabetes in pregnancy are needed as rates of type 2 diabetes in pregnancy increase. Maternal obesity is a known challenge to establishing breastfeeding, and this study adds further evidence that women with obesity, regardless of glycaemic status, require increased support with breastfeeding. Long-term evaluation of the impact of breastfeeding on growth and metabolic outcomes for the offspring of women, particularly those with hyperglycaemia in pregnancy, will be important. Further detailed evaluation regarding factors contributing to successful breastfeeding in Indigenous women may inform policy and interventions and result in increased breastfeeding success for all women.
Conclusion
We report a key positive finding that Indigenous women across the glycaemic spectrum in pregnancy have higher rates of breastfeeding than non-Indigenous women. We also report that women with pre-existing type 2 diabetes in pregnancy have greater difficulty establishing exclusive breastfeeding at hospital discharge. Awareness of in-hospital breastfeeding challenges for women with type 2 diabetes are needed in addition to guidance for women with type 2 diabetes within national and international breastfeeding policies. Maternal obesity has a negative impact on breastfeeding, independent of hyperglycaemia in pregnancy.
Data availability
Data are available on request to the Partnership Steering Committee. They are not included in the ESM or available on an online repository.
Abbreviations
- GDM:
-
Gestational diabetes mellitus
- NT:
-
Northern Territory
- PANDORA:
-
Pregnancy And Neonatal Diabetes Outcomes in Remote Australia
References
Victora CG, Bahl R, Barros AJ et al (2016) Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 387(10017):475–490. https://doi.org/10.1016/S0140-6736(15)01024-7
World Health Organization (2014) Global nutritional targets 2025: Breastfeeding policy brief. WHO, Geneva, pp8
Crume TL, Ogden L, Maligie M et al (2011) Long-term impact of neonatal breastfeeding on childhood adiposity and fat distribution among children exposed to diabetes in utero. Diabetes Care 34(3):641–645. https://doi.org/10.2337/dc10-1716
Harder T, Bergmann R, Kallischnigg G, Plagemann A (2005) Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol 162(5):397–403. https://doi.org/10.1093/aje/kwi222
Al Mamun A, O'Callaghan MJ, Williams GM, Najman JM, Callaway L, McIntyre HD (2015) Breastfeeding is protective to diabetes risk in young adults: A longitudinal study. Acta Diabetol 52(5):837–844. https://doi.org/10.1007/s00592-014-0690-z
Finkelstein SA, Keely E, Feig DS, Tu X, Yasseen AS 3rd, Walker M (2013) Breastfeeding in women with diabetes: lower rates despite greater rewards. A population-based study. Diabet Med 30(9):1094–1101. https://doi.org/10.1111/dme.12238
Kachoria R, Moreland JJ, Cordero L, Oza-Frank R (2015) Trends in breastfeeding initiation, continuation, and exclusivity by maternal prepregnancy weight: 2004-2011. Obesity (Silver Spring) 23(9):1895–1902. https://doi.org/10.1002/oby.21151
Amir LH, Donath S (2007) A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy Childbirth 7:9. https://doi.org/10.1186/1471-2393-7-9
Pinheiro TV, Goldani MZ, IVAPSA group (2018) Maternal pre-pregnancy overweight/obesity and gestational diabetes interaction on delayed breastfeeding initiation. PLoS One 13(6):e0194879. https://doi.org/10.1371/journal.pone.0194879
De Bortoli J, Amir LH (2016) Is onset of lactation delayed in women with diabetes in pregnancy? A systematic review. Diabet Med 33(1):17–24. https://doi.org/10.1111/dme.12846
Oza-Frank R, Chertok I, Bartley A (2015) Differences in breast-feeding initiation and continuation by maternal diabetes status. Public Health Nutr 18(4):727–735. https://doi.org/10.1017/S1368980014000792
Simmons D, Conroy C, Thompson CF (2005) In-hospital breast feeding rates among women with gestational diabetes and pregestational type 2 diabetes in South Auckland. Diabet Med 22(2):177–181. https://doi.org/10.1111/j.1464-5491.2004.01379.x
Baerug A, Laake P, Loland BF, Tylleskar T, Tufte E, Fretheim A (2017) Explaining socioeconomic inequalities in exclusive breast feeding in Norway. Arch Dis Child 102(8):708–714. https://doi.org/10.1136/archdischild-2016-312038
Rempel LA, Rempel JK, Moore KCJ (2017) Relationships between types of father breastfeeding support and breastfeeding outcomes. Matern Child Nutr 13(3). https://doi.org/10.1111/mcn.12337
Porter C, Skinner T, Ellis I (2012) The current state of indigenous and aboriginal women with diabetes in pregnancy: a systematic review. Diabetes Res Clin Pract 98(2):209–225. https://doi.org/10.1016/j.diabres.2012.07.006
Eades SJ, Read AW, McAullay D, McNamara B, O'Dea K, Stanley FJ (2010) Modern and traditional diets for Noongar infants. J Paediatr Child Health 46(7–8):398–403. https://doi.org/10.1111/j.1440-1754.2010.01752.x
Gracey M (2000) Historical, cultural, political, and social influences on dietary patterns and nutrition in Australian aboriginal children. Am J Clin Nutr 72(5 Suppl):1361S–1367S. https://doi.org/10.1093/ajcn/72.5.1361s
Scott JA, Binns C (2011) Infant feeding in indigenous Australian communities. In: Liamputtong P (ed) Infant feeding practices. Springer, New York
Amir LH, Donath SM (2008) Socioeconomic status and rates of breastfeeding in Australia: evidence from three recent national health surveys. Med J Aust 189(5):254–256
Craig PL, Knight J, Comino E, Webster V, Pulver LJ, Harris E (2011) Initiation and duration of breastfeeding in an aboriginal community in south western Sydney. J Hum Lact 27(3):250–261. https://doi.org/10.1177/0890334411402998
McLachlan HL, Shafiei T, Forster DA (2017) Breastfeeding initiation for aboriginal and Torres Strait islander women in Victoria: Analysis of routinely collected population-based data. Women Birth 30(5):361–366. https://doi.org/10.1016/j.wombi.2017.02.011
Hayman N, Kanhutu J, Bond S, Marks GC (2000) Breast-feeding and weaning practices of an urban community of indigenous Australians. Asia Pac J Clin Nutr 9(3):232–234. https://doi.org/10.1046/j.1440-6047.2000.00193.x
Cromie EA, Shepherd CC, Zubrick SR, Oddy WH (2012) Breastfeeding duration and residential isolation amid aboriginal children in Western Australia. Nutrients 4(12):2020–2034. https://doi.org/10.3390/nu4122020
Martens PJ, Shafer LA, Dean HJ et al (2016) Breastfeeding initiation associated with reduced incidence of diabetes in mothers and offspring. Obstet Gynecol 128(5):1095–1104. https://doi.org/10.1097/AOG.0000000000001689
Louis-Jacques A, Deubel TF, Taylor M, Stuebe AM (2017) Racial and ethnic disparities in U.S. breastfeeding and implications for maternal and child health outcomes. Semin Perinatol 41(5):299–307. https://doi.org/10.1053/j.semperi.2017.04.007
Hall J, O'Neil L (2016) Northern Territory midwives' collection: Mothers and babies 2014. Department of Health, Darwin
Cheng E, Longmore DK, Barzi F et al (2019) Birth outcomes in women with gestational diabetes managed by lifestyle modification alone: The PANDORA study. Diabetes Res Clin Pract 157:107876. https://doi.org/10.1016/j.diabres.2019.107876
Hoffman L, Nolan C, Wilson JD, Oats JJ, Simmons D (1998) Gestational diabetes mellitus--management guidelines. The Australasian diabetes in pregnancy society. Med J Aust 169(2):93–97
International Association of Diabetes, Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG et al (2010) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682. https://doi.org/10.2337/dc09-1848
Australian Bureau of Statistics (2018) Australian Statistical Geography Standard (ASGS): Volume 5 - Remoteness structure, July 2016. In: Australian Bureau of Statistics (ed) Australian Statisitical Geography Standard (ASGS). Vol 5. ABS, Canberra
Kruske SD, Donovan J, McKinnon T, Nuttall L (2009) Healthy Under 5 Kids Program: education package. Department of Health and Families, Northern Territory. Northern Territory Government, Darwin, p 226
World Health Organization (2003) Global strategy for infant and young child feeding. World Health Organization, Geneva
Taylor LK, Lim K, Neville SE (2009) Newborn feeding practices at the time of discharge from hospital in NSW in 2007: a descriptive study. N S W Public Health Bull 20(11–12):177–181. https://doi.org/10.1071/NB09024
Helps C, Barclay L (2015) Aboriginal women in rural Australia; a small study of infant feeding behaviour. Women Birth 28(2):129–136. https://doi.org/10.1016/j.wombi.2014.12.004
Chamberlain CR, Wilson AN, Amir LH et al (2017) Low rates of predominant breastfeeding in hospital after gestational diabetes, particularly among indigenous women in Australia. Aust N Z J Public Health 41(2):144–150. https://doi.org/10.1111/1753-6405.12629
Veile A, Kramer K (2015) Birth and breastfeeding dynamics in a modernizing indigenous community. J Hum Lact 31(1):145–155. https://doi.org/10.1177/0890334414557177
Pettitt DJ, Knowler WC (1998) Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima Indians. Diabetes Care 21(Suppl 2):B138–B141
Matias SL, Dewey KG, Quesenberry CP Jr, Gunderson EP (2014) Maternal prepregnancy obesity and insulin treatment during pregnancy are independently associated with delayed lactogenesis in women with recent gestational diabetes mellitus. Am J Clin Nutr 99(1):115–121. https://doi.org/10.3945/ajcn.113.073049
Rasmussen B, Nankervis A, Skouteris H et al (2019) Factors associated with breastfeeding to 3 months postpartum among women with type 1 and type 2 diabetes mellitus: an exploratory study. Women Birth. https://doi.org/10.1016/j.wombi.2019.06.008
Kachoria R, Oza-Frank R (2014) Factors associated with breastfeeding at discharge differ by maternal diabetes type. Diabet Med 31(10):1222–1229. https://doi.org/10.1111/dme.12442
Institute of Medicince (US), National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines (2009) Weight gain during pregnancy: Reexamining the guidelines. In: Rasmussen KM, Yaktine AL (eds) The National Academies Collection: Reports funded by National Institutes of Health. National Academies Press, Washington
Acknowledgements
We gratefully acknowledge all PANDORA participants and staff including S. Svenson, L. Davis and V. Hampton, in addition to the NT DIP investigators, Indigenous Reference Group, Clinical Reference Group, NT health professionals from NT department of health hospitals, remote primary healthcare, Healthy Living NT and Aboriginal Community Controlled Health Organisations. NT DIP investigators in addition to those listed as author include E. Moore, G. Dent, M. Stone, M. Harris, C. Inglis, K. Dempsey, S. Thomas, S. Chitturi, S. Eades, S. Corpus, M. Lynch and Z. Lu.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
The PANDORA study was funded by National Health and Medical Research Council of Australia (NHMRC Partnership Project Grant #1032116, NHMRC #1078333). DKL was supported by an NHMRC scholarship (#1038372) and LJMB was supported by an NHMRC fellowship (#605837) and NHMRC Practitioner fellowship (#1078477). ELMB was supported by a National Heart Foundation post-doctoral fellowship (#101291). ILL was supported by an Australian Postgraduate award and Menzies scholarship. ADHB was supported by an NHMRC Senior Research fellowship (#1137563) and a Sylvia and Charles Viertel Senior Medical Research fellowship. JES was supported by an NHMRC fellowship (#1079438). This paper reflects the views of the authors and not the NHMRC.
Author information
Authors and Affiliations
Contributions
DKL was involved in the study design, literature search, data analysis, data interpretation, and drafted the manuscript. ELMB was involved in interpreting the data and writing of the manuscript. FB was involved in data analysis, data interpretation and writing of the manuscript. ANW was involved in data collection, data analysis and writing of the manuscript. MK, PVD and AS were involved in study design, acquisition of data, coordination of the project and writing of the manuscript. EH was involved in the interpretation of data and writing of the manuscript. ILL, KOD, CC, JAB, ADHB, PZ, JO, HDM and JES were involved in the study conception and design and writing of the manuscript. LJMB led the study design, supervision of data collection, data interpretation, and writing of the manuscript and is the guarantor for the study. All authors approved the final manuscript.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM
(PDF 309 kb)
Rights and permissions
About this article
Cite this article
Longmore, D.K., Barr, E.L.M., Wilson, A.N. et al. Associations of gestational diabetes and type 2 diabetes during pregnancy with breastfeeding at hospital discharge and up to 6 months: the PANDORA study. Diabetologia 63, 2571–2581 (2020). https://doi.org/10.1007/s00125-020-05271-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-020-05271-9