Abstract
Purpose
After laparoscopic cholecystectomy patients have moderate pain in the early postoperative period. According to several studies an erector spinae plane (ESP) block can be a valuable part of multimodal analgesia. Our intention was to evaluate how ESP block influences postoperative pain scores and opioid consumption after laparoscopic cholecystectomy.
Methods
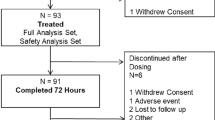
This single-blinded, prospective, randomized study included 60 patients undergoing laparoscopic cholecystectomy to receive either bilateral ESP block at the Th 7 level (n = 30) with 20 ml of 0.25% levobupivacaine plus dexamethasone 2 mg per side, or standard multimodal analgesia (n = 30). Patients from the standard multimodal analgesia group received tramadol 100 mg at the end of the procedure. Postoperative analgesia for both groups was acetaminophen 1 g/8 h i.v. and ketorolac 30 mg/8 h. Tramadol 1 mg/kg was a rescue treatment for pain breakthrough (numeric rating scale/NRS ≥ 6) in both groups. Pain at rest was recorded at 10 min, 30 min, 2 h, 4 h, 8 h, 12 h and 24 h after surgery using NRS (0–10).
Results
An ESP block significantly reduced postoperative pain scores compared to standard multimodal analgesia after 10 min (p = 0.011), 30 min (p = 0.004), 2 h (p = 0.011), 4 h (p = 0.003), 8 h (p = 0.013), 12 h (p = 0.004) and 24 h (p = 0.005). Tramadol consumption was significantly lower in the ESP group 25.02 ± 56.8g than in the standard analgesia group 208.3 ± 88.1g (p < 0.001).
Conclusion
An ESP block can provide superior postoperative analgesia and reduction in opioid requirement after laparoscopic cholecystectomy
Zusammenfassung
Ziel
Nach einer laparoskopischen Cholezystektomie haben Patienten in der frühen postoperativen Phase mäßige Schmerzen. Mehreren Studien zufolge kann der Erector-spinae-plane-Block (ESP) zum wertvollen Bestandteil der multimodalen Analgesie werden. Ziel dieser Arbeit war es, zu untersuchen, wie der ESP-Block den postoperativen Schmerzscore und den Opioidverbrauch nach einer laparoskopischen Cholezystektomie beeinflusst.
Methoden
Die einzelverblindete, prospektive, randomisierte Studie schloss 60 Patienten ein, die sich einer laparoskopischen Cholezystektomie unterzogen, um entweder einen bilateralen ESP-Block in Höhe des Th 7 (n = 30) mit 20 ml 0,25 % Levobupivacain plus Dexamethason 2 mg pro Seite oder eine standardmäßige multimodale Analgesie (n = 30) zu erhalten. Die Patienten der multimodalen Standardanalgesiegruppe erhielten am Ende des Eingriffs Tramadol 100 mg. Die postoperative Analgesie für beide Gruppen war Paracetamol 1 g/8 h i.v. und Ketorolac 30 mg/8 h. Tramadol 1 mg/kg war eine Rescue-Therapie bei Schmerzdurchbruch (NRS ≥ 6) in beiden Gruppen. Der Ruheschmerz wurde 10 min, 30 min, 2 h, 4 h, 8 h, 12 h und 24 h nach der Operation aufgezeichnet, wobei eine NR-Skala (0–10) verwendet wurde.
Ergebnisse
Der ESP-Block reduzierte deutlich die postoperativen Schmerzscores (NRS) im Vergleich zur multimodalen Standardanalgesie nach 10 min (p = 0,011), 30 min (p = 0,004), 2h (p = 0,011), 4h (p = 0,003), 8 h (p = 0,013), 12 h (p = 0,004) und 24 h (p = 0,005). Der Tramadolverbrauch war in der ESP-Gruppe mit 25,02 ± 56,8 g deutlich niedriger als in der Standardanalgesie-Gruppe mit 208,3 ± 88,1 g (p < 0,001).
Schlussfolgerung
Der ESP-Block kann eine überlegene postoperative Analgesie und eine Reduzierung des Opioidbedarfs nach laparoskopischer Cholezystektomie bieten

Similar content being viewed by others
References
Bisgaard T (2006) Analgesic treatment after laparoscopic cholecystectomy: a critical assessment of the evidence. Anesthesiology 104:835–846
Barazanchi AWH, MacFater WS, Rahiri JI, Tutone S, Hill AG, Joshi GP (2018) Evidence-based management of pain after laparoscopic cholecystectomy: a PROSPECT review update. Br J Anaesth 121(4):787–803
Jesus RR, Leite AM, Leite SS, Vieira MC, Villela NR (2018) Anesthetic therapy for acute pain relief after laparoscopic cholecystectomy: systematic review. Rev Col Bras Cir 45(4):1885
Sinha S, Munikrishnan V, Montgomery J, Mitchell SJ (2007) The impact of patient-controlled analgesia on laparoscopic cholecystectomy. Ann R Coll Surg Engl 89(4):374–378
Lledó HB, Castro PB, Gavara IG, Cirión JLI, Andújar RL, Granero EG (2016) Twenty-five years of ambulatory laparoscopic. Cir Esp 94(8):429–441
Zhao J, Peters L, Gelzinnis S, Carroll R, Nolan J, Di Sano S, Pockney P, Smith S (2020) Post-discharge opioid prescribing after laparoscopic appendicectomy and cholecystectomy. ANZ J Surg 90:1014–1018. https://doi.org/10.1111/ans.15882
Tolchard S, Davies R, Martindale S (2012) Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: comparison with conventional port-site infiltration. J Anaesthesiol Clin Pharmacol 28:339–343
Peng K, Ji FH, Liu HY, Wu SR (2016) Ultrasound-guided transversus abdominis plane block for analgesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Med Princ Pract 25:237–246
Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ (2016) The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med 41(5):621–627
Kot P, Rodriguez P, Granell M, Cano B, Rovira L, Morales J, Broseta A, Andrés J (2019) The erector spinae plane block: a narrative review. Korean J Anesthesiol 72(3):209–220
Kadam VR, Wahba M (2018) Use of erector spinae plane block in open abdominal surgery and cancer pain. J Anaesthesiol Clin Pharmacol 34(4):564–567
Hannig KE, Jessen C, Soni UK, Børglum J, Bendtsen TF (2018) Erector spinae plane block for elective laparoscopic cholecystectomy in the ambulatory surgical setting. Case Rep Anesthesiol 2018:5492527
Chin KJ, Malhas L, Perlas A (2017) The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. Reg Anesth Pain Med 42(3):372–376
De Cassai A, Bonvicini D, Correale C, Sandei L, Tulgar S, Tonetti T (2019) Erector spinae plane block: a systematic qualitative review. Minerva Anestesiol 85(3):308–319
Tulgar S, Kapakli MS, Senturk O, Selvi O, Serifsoy TE, Ozer Z (2018) Evaluation of ultrasound-guided erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical trial. J Clin Anesth 49:101–106
Altiparmak B, Korkmaz Toker M, Uysal AI, Kuşçua Y, Gümüş Demirbilek S (2019) Efficacy of ultrasound-guided erector spinae planeblock for analgesia after laparoscopiccholecystectomy: a randomized controlled trial. Braz J Anesthesiol 69(6):561–568
Tulgar S, Kapakli MS, Kose HC, Senturk O, Selvi O, Serifsoy TE et al (2019) Evaluation of ultrasound-guided erector spinae plane block and oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: randomized, controlled, prospective study. Anesth Essays Res 13:50–56
Altıparmak B, Korkmaz Toker M, Uysal AI, Kuşçu Y, Gümüş Demirbilek S (2019) Ultrasound-guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: Randomized, controlled trial. J Clin Anesth 57:31–36
Niraj G, Zubair T (2018) Continuous erector spinae plane (ESP) analgesia in different open abdominal surgical procedures: a case series. J Anesth Surg 5(1):57–60
Vrsajkov V, Mančić N, Mihajlović D, Milićević ST, Uvelin A, Vrsajkov JP (2018) Subcostal transversus abdominis plane block can improve analgesia after laparoscopic cholecystectomy. Rev Bras Anestesiol 68(2):149–153
Loizides S, Gurusamy KS, Nagendran M, Rossi M, Guerrini GP, Davidson BR (2014) Wound infiltration with local anaesthetic agents for laparoscopic cholecystectomy. Cochrane Database Syst Rev 3:CD7049
Guo Q, Li R, Wang L, Zhang D, Ma Y (2015) Transversus abdominis plane block versus local anaesthetic wound infiltration for postoperative analgesia: a systematic review and meta-analysis. Int J Clin Exp Med 8(10):17343–17352
Kwon H, Kim D, Jeong S et al (2020) Does erector spinae plane block have a visceral analgesic effect?: A randomized controlled trial. Sci Rep 10:8389
Bisgaard T, Rosenberg J, Kehlet H (2005) From acute to chronic pain after laparoscopic cholecystectomy: a prospective follow-up analysis. Scand J Gastroenterol 40(11):1358–1364
Blichfeldt-Eckhardt MR, Ording H, Andersen C, Licht PB, Toft P (2014) Early visceral pain predicts chronic pain after laparoscopic cholecystectomy. Pain 155(11):2400–2407
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
V. Vrsajkov, N. Ilić, A. Uvelin, R. Ilić, M. Lukić-Šarkanović and A. Plećaš-Đurić declare that they have no competing interests.
Ethical standards.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Vrsajkov, V., Ilić, N., Uvelin, A. et al. Erector spinae plane block reduces pain after laparoscopic cholecystectomy. Anaesthesist 70 (Suppl 1), 48–52 (2021). https://doi.org/10.1007/s00101-021-01015-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-021-01015-5