Abstract
Background
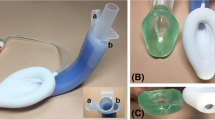
The LMA SupremeTM (LMA-S) and i-gelTM are two of the most commonly used supraglottic airway devices (SADs) with an inbuilt drain channel. These devices are particularly indicated for performing certain procedures accompanied by high peak airway pressure, such as laparoscopy. This study compared the devices regarding efficacy, safety, ease of use and incidence of adverse events, focusing on the postoperative rate of sore throat, dysphagia or dysphonia and development with time, in patients undergoing laparoscopic cholecystectomy procedures under general anesthesia.
Methods
This was a prospective, randomized, controlled clinical study including 140 patients randomized into 2 groups undergoing elective laparoscopic cholecystectomy to use either i-gel or LMA-S. After the general anesthesia procedure, the speed of insertion, success rates, ease of insertion of the drain tube, leak pressure and tidal volume achieved by the devices were evaluated. The postoperative oropharyngeal discomfort (POPD) during the period of stay of the patients in the recovery room was also recorded.
Results
The mean leak pressure was comparable between the two groups (i-gel 28.18 ± 3.90 cmH2O and LMA-S 27.50 ± 4 cmH2O, p = 0.09), as well as maximum expiratory tidal volume provided (i-gel 559.60 ± 45.25 ml and LMA-S 548.95 ± 56.18 ml, p = 0.12). Insertion times were lower for the i-gel (10 ± 1.62 s) compared with the LMA-S (11.31 ± 2.85 s, p = 0.008). Insertion success rate at the first attempt was higher for the LMA-S (95 % compared with i-gel 79 %, p = 0.007). Drain tubes were easier to insert in the LMA-S group (p < 0.001). No differences were found between groups relating to intraoperative complications. Frequency of coughing and visible blood on removal of the device were low and comparable in both groups (p = 0.860 and p = 0.623, respectively). There were no differences relating to the incidence of sore throat, dysphagia or hoarseness at 10 min postoperatively between groups (p = 0.088). The i-gel group complained about a higher sore throat score at 2 h postoperatively (p = 0.009), specifically patients receiving i-gel suffered more from sore throats with 0.24 more points on the visual analog scale (VAS) than patients from the LMA-S group. The i-gel group also reported a lower POPD drop during the first 2 h (p < 0.001).
Conclusion
No differences were found between i-gel and LMA-S regarding leak pressure in the groups of anesthetized patients undergoing laparoscopic cholecystectomy. The LMA-S was easier to insert than the i-gel (based on its better first time success rate) and this device showed better ease of drain tube insertion, although the i-gel was quicker to insert than the LMA-S. The i-gel resulted in higher sore throat scores at 2 h postoperatively and lower POPD reduction during the 2 h period studied in the recovery room was reported.
Zusammenfassung
Hintergrund
LMA SupremeTM (LMA-S) und i-gelTM sind 2 der am häufigsten verwendeten supraglottischen Beatmungsgeräte mit eingebautem Magensaftablaufkanal. Sie sind besonders indiziert bei Interventionen, bei denen es zu hohen Spitzen im Atemwegsdruck kommt, etwa bei Laparoskopien. In der Studie wurden Wirksamkeit, Sicherheit, Benutzerfreundlichkeit und die Inzidenz von unerwünschten Ereignissen verglichen. Besondere Beachtung erfuhren dabei die Raten an postoperativ auftretenden Halsschmerzen, Dysphagie oder Dysphonie und der Entwicklung im zeitlichen Verlauf bei Patienten nach laparoskopischer Cholezystektomie in Allgemeinnarkose.
Methoden
In die prospektive, kontrollierte klinische Studie wurden 140 Patienten aufgenommen, die sich einer elektiven laparoskopischen Cholezystektomie unterzogen; sie wurden randomisiert auf 2 Gruppen und mit i-gel oder LMA-S intubiert. Nach Allgemeinanästhesie wurden evaluiert: Geschwindigkeit der Einführung, Erfolgsraten, Benutzerfreundlichkeit hinsichtlich der Einführung der Magensonde über den Ablaufkanal, Dichtheitsdruck und Atemvolumen. Darüber hinaus wurden postoperative oropharyngeale Beschwerden („postoperative oropharyngeal discomfort“, POPD) der Patienten während des Aufenthalts im Aufwachraum dokumentiert.
Ergebnisse
Dichtheitsdruck (i-gel 28,18 ± 3,90; LMA-S 27,50 ± 4 cm H2O, p = 0,09) und maximales exspiratorisches Atemvolumen (i-gel 559,60 ± 45,25; LMA-S 548,95 ± 56,18 ml, p = 0,12) waren in beiden Gruppen vergleichbar. Die Einführungszeiten waren beim i-gel niedriger als beim LMA-S (10 ± 1,62 vs. 2,85 ± 11,31 s, p = 0,008). Die Einführungerfolgsquote beim ersten Versuch war höher beim LMA-S (95 % vs. i-gel: 79 %, p = 0,007). Die Platzierung einer Magensonde über den Ablaufkanal wurde als einfacher in der LMA-S-Gruppe (p < 0,001) beurteilt. Hinsichtlich intraoperativer Komplikationen wurden keine Gruppenunterschiede beobachtet. Husten und Blutspuren bei Entfernung der Geräte waren selten und in beiden Gruppen vergleichbar (p = 0,860 bzw. p = 0,623). Zehn Minuten postoperativ gab es keine Gruppenunterschiede (p = 0,088) in der Inzidenz von Halsschmerzen, Dysphagie und Heiserkeit. In der i-gel-Gruppe zeigten sich höhere Werte in den Angaben zu Halsschmerzen 2 h postoperativ (p = 0,009), vor allem litten die i-gel-Patienten mehr an Halsschmerzen (0,24 mehr auf der visuellen Analogskala, VAS) als die Patienten der LMA-S-Gruppe. In der i-gel-Gruppe verringerten sich die POPD in den ersten 2 postoperativen Stunden weniger (p < 0,001).
Schlussfolgerungen
Zwischen i-gel und LMA-S wurden im Hinblick auf den Dichtheitsdruck keine Unterschiede gefunden. LMA-S war leichter einzuführen als i-gel (auf der Basis der besseren initialen Erfolgsrate), und bei diesem Geräte war das Einführen der Magensonde leichter, auch wenn i-gel schneller einzusetzen waren als LMA-S. Nach i-gel wurden 2 h postoperative höhere Halsschmerzenscores angegeben und eine geringere POPD-Verringerung während der 2 h im Aufwachraum.


Similar content being viewed by others
References
O’Connor CJ Jr, Stix MS, Valade DR (2005) Glottic insertion of the ProSeal LMA occurs in 6 % of cases: a review of 627 patients. Can J Anaesth 52(2):199–204
Maltby JR, Beriault MT, Watson NC et al (2003) LMA-Classic™ and LMA-ProSeal™ are effective alternatives to endotracheal intubation for gynecologic laparoscopy. Can J Anaesth 50:71–77
Natalini G, Lanza G, Rosano A et al (2003) Standard Laryngeal Mask Airway™ and LMA-ProSeal™ during laparoscopic surgery. J Clin Anesth 15:428–432
Lee AK, Tey JB, Lim Y, Sia AT (2009) Comparison of the single-use LMA Supreme with the reusable Proseal LMA for anaesthesia in gynaecological laparoscopic surgery. Anaesth Intensive Care 37:815–819
Teoh WH, Lee KM, Suhitharan T et al (2010) Comparison of the LMA Supreme vs i-gel in paralysed patients undergoing gynaecological laparoscopic surgery with controlled ventilation. Anaesthesia 65:1173–1179
Yao T, Yang XL, Zhang F et al (2010) The feasibility of Supreme laryngeal mask airway in gynaecological laparoscopy surgery. Zhonghua Yi Xue Za Zhi 90:2048–2051
Beleña JM, Nuñez M, Anta D et al (2013) Comparison of LMA Supreme™ and LMA Proseal™ with respect to oropharyngeal leak pressure in patients undergoing anaesthesia during laparoscopic cholecystectomy: a randomized controlled trial. Eur J Anaesthesiol 30:119–123
Sharma B, Sehgal R, Sahai C, Sood J (2010) PLMA vs. I-gel: a comparative evaluation of respiratory mechanics in laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol 26:451–457
Woo JJ, Sang YC, Seong JB, Kyoung HK (2012) Comparison of the Proseal LMA and Intersurgical I-gel during gynaecological laparoscopy. Korean J Anesthesiol 63:510–514
Keller C, Brimacombe JR, Keller K, Morris R (1999) Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth 82:286–287
Russo SG, Cremer S, Galli T et al (2012) Randomized comparison of the i-gel™, the LMA Supreme™ and the Laryngeal Tube Suction-D using clinical and fibreoptic assessment in elective patients. BMC Anesthesiol 12:18
Beleña JM, Gracia JL, Ayala JL et al (2011) The Laryngeal Mask Airway Supreme for positive pressure ventilation during laparoscopic cholecystectomy. J Clin Anesth 23:456–460
Gatward JJ, Cook TM, Seller C et al (2008) Evaluation of the size 4 i-gel airway in one hundred non-paralysed patients. Anaesthesia 63(10):1124–1130
Timmermann A, Cremer S, Eich C et al (2009) Prospective clinical and fiberoptic evaluation of the Supreme Laryngeal Mask Airway™. Anesthesiology 110:262–265
Fernández A, Pérez A, Bermejo JC, Marcos JM (2009) Supreme Laryngeal Mask Airway vs the I-gel Supraglottic Airway in patients under general anesthesia and mechanical ventilation with no neuromuscular block: a randomized clinical trial. Rev Esp Anestesiol Reanim 56:474–478
Theiler LG, Kleine-Brueggeney M, KaiserD et al (2009) Crossover comparison of the laryngeal mask supreme and the i-gel in simulated difficult airway scenario in anesthetized patients. Anesthesiology 111:55–62
Ragazzi R, Finessi L, Farinelli I et al (2012) LMA Supreme™ vs i-gel™: a comparison of insertion success in novices. Anaesthesia 67:384–388
Acknowledgements
The authors would like to thank Sebastian Fairhurst for help and support in translating the English abstract text into German.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.M. Beleña, M. Núñez, A. Vidal, C. Gasco, A. Alcojor, P. Lee and J.L. Pérez state that there are no conflicts of interest. All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Disclosure of funding
No funds were received for the study from any of the following organizations: National Institutes of Health (NIH), Spanish Society of Anaesthesiology (SSAR), Regional Government of Madrid (RGM), neither from other organization, including departmental or institutional funding.
Clinical trial registry
This trial was not registered in any public registry due to the starting date for patient enrolment (September 2009).
Additional information
Author contributions:
J.M. Beleña: study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript and critical revision.
M. Nuñez: study conception and design, acquisition of data, drafting of manuscript and critical revision.
A. Vidal: study conception and design, analysis and interpretation of data, drafting of manuscript and critical revision.
C. Gasco: study conception and design, drafting of manuscript and critical revision.
A. Alcojor: acquisition of data, drafting of manuscript and critical revision.
P. Lee: analysis and interpretation of data, drafting of manuscript and critical revision.
Rights and permissions
About this article
Cite this article
Beleña, J., Núñez, M., Vidal, A. et al. Randomized comparison of the i-gelTM with the LMA SupremeTM in anesthetized adult patients. Anaesthesist 64, 271–276 (2015). https://doi.org/10.1007/s00101-015-0020-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-015-0020-z