Abstract
Purpose
Chest trauma is a severe and frequent cause of admission to the emergency department (ED). The serratus anterior plane (SAP) block seems to be an effective method of pain management; however, data on efficacy and safety of a single SAP block performed in the ED by emergency physicians (EP) are limited. This study aimed to compare SAP block performed by the EP in the ED plus standard therapy to standard therapy alone in terms of pain severity at 0-3-6-12-18 and 24 h, total opioid consumption (milligrams of morphine equivalents, MME), respiratory function (SpO2/FiO2 ratio), and adverse events (i.e. pneumothorax, infections in the site of injection, or Local Anaesthetic Systemic Toxicity syndrome due to SAP block) in the first 24 h.
Methods
This retrospective, monocentric study included adult patients admitted to the Sub-intensive Care Unit (SICU) of the ED with multiple rib fractures between 01/2022 and 03/2023.
Results
156 patients (65.4% male; median age 62 years; median injury severity score 16; median thoracic trauma severity score 8) were included. 75 (48.2%) underwent SAP block. Patients undergoing SAP block showed significantly less pain 3–6–18 h after a single block, required less MME (0 [0–20] vs. 20 [0–40], p < 0.001), showed higher SpO2/FiO2 ratio, and no adverse events were reported.
Conclusion
The SAP block, in combination with standard therapy, appeared to be more effective in providing pain relief than standard therapy alone in patients admitted to the SICU for traumatic rib fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blunt chest trauma is a serious presentation to the emergency department (ED) that can lead to acute impairment of respiratory function, including respiratory failure and death, due to acute damage to the thoracic structures or worsening of pre-existing pathological conditions [1]. Multiple rib fractures play a significant role in blunt chest trauma and are associated with a high risk of morbidity and mortality, particularly in elderly patients [2, 3]. In the early stages, pneumothorax, haemothorax, and lung contusions are the most frequently observed injuries in chest trauma [2], which can lead to acute respiratory failure and respiratory arrest. In the late stages, uncontrolled severe pain leads to (i) reduced thoracic excursion with reduced functional residual respiratory capacity [4] and (ii) impaired cough with reduced secretion clearance [5, 6], secondary atelectasis, and a higher risk of infection. Secondary pneumonia is one of the principal risk factors for in-hospital death due to subsequent hypoxemia and an inflammatory systemic response affecting multiple organ functions [7], possibly leading to admission to the intensive care unit and death [8]. Therefore, effective pain management should be considered a fundamental step in the treatment of chest trauma, which should be achieved as soon as possible [7, 9] to promote pulmonary ventilation and good respiratory rehabilitation [10,11,12,13] and to improve the patient’s overall outcome [3, 5, 11, 14].
Various analgesic methods and combinations have been evaluated for rib fracture-related pain treatment, including paracetamol and non-steroidal anti-inflammatory drugs, systemic opioids, patient-controlled analgesia, lidocaine patches, and regional analgesia techniques such as thoracic epidural and paravertebral catheters, and intercostal and paravertebral blocks [5, 15, 16]. However, the use of traditional regional analgesia techniques may be limited because of underlying injuries (e.g., spinal injuries), contraindications (e.g., trauma-related coagulopathy and anticoagulant medications), multimorbidity (especially in elderly trauma patients), and inability to position the patient during the acute phase [17]. In the last decade, interest in chest wall fascial blocks, such as the serratus anterior plane block (SAP block), erector spine plane block, and rhomboid intercostal block, has increased [4, 15]. The SAP block [18,19,20] is a fascial block traditionally used for surgical anaesthesia and postoperative analgesia in thoracic procedures as an alternative to more invasive paravertebral and epidural blocks. It involves injecting a long-acting local anaesthetic, such as ropivacaine, bupivacaine, or levobupivacaine, into a virtual anatomical space between two fasciae, one surrounding the latissimus dorsi muscle and the other covering the serratus anterior muscle. The injection of the local anaesthetic in this virtual space, distant from both the pleural cavity and the major nerve or vascular branches, and the use of ultrasound for real-time guidance of the technique significantly reduce the likelihood of complications such as thoracic injury (pneumothorax), neurovascular damage, and systemic complications in comparison to other techniques [21, 22].
Injecting the local anaesthetic into this space at the level of the 5th intercostal space on the midaxillary line (or between the 3rd and 7th ribs) allows the anaesthetic to reach the nerve fibres of the cutaneous lateral branch of the intercostal nerves of the hemithorax [23]. It is particularly effective in controlling pain in the anterior and lateral chest areas between T2 and T9 [18], while its efficacy in managing pain in more posterior regions is questionable [24]. The local anaesthetic is also capable of blocking nerve conduction of the branches innervating the ribs, rib-sternal joints, and cartilage-rib muscles and is potentially extremely helpful in controlling pain following thoracic trauma [23].
Despite increasing evidence regarding the efficacy and safety of fascial nerve blocks, this novel technique is largely underutilised. A report from the U.S. National Trauma Database indicates that only 3 per cent of patients with thoracic trauma eligible for fascial nerve blocks have access to this treatment [25].
The objective of this study was to investigate the efficacy and safety of SAP block performed by emergency physicians in the ED and sub-intensive care unit (SICU) compared with standard care alone in terms of pain control, opioid consumption, and adverse events in the first 24 h after admission in adult patients with multiple rib fractures.
Methods
This is a retrospective observational study based on electronic medical records of adult patients admitted to the SICU of the ED of the “M. Bufalini” Hospital in Cesena, Italy, from January 2022 to March 2023, with multiple rib fractures due to traumatic injuries, regardless of the presence of other traumatic injuries. Patients (i) admitted to other hospital care units, (ii) dismissed at home, (iii) lost to follow-up or with a lack of data in the first 24 h, or (iv) with contraindications to opioids were excluded from the study.
The “M. Bufalini” hospital in Cesena is a level I trauma centre designated as an integrated system for caring for trauma patients of the Emilia Romagna Regional Health Service in northern Italy and treats approximately 65,000 patients annually. The ED of the “M. Bufalini” Hospital in Cesena is equipped with four physicians 24 h a day, seven days a week, and provides unscheduled care for patients whose condition requires immediate treatment, including patients with hemodynamic instability and multiple traumas. The ED has seven monitored beds available for prolonged observation (up to 24 h) and a 24-bed Sub-Intensive Care Unit (SICU), eight of which are monitored and provide the ability to perform invasive and non-invasive ventilation, invasive and non-invasive blood pressure monitoring, and treatment of patients with clinical and hemodynamic instability. The SICU is managed by an emergency physician who works alternately in the ED and the SICU.
From June 2022, the emergency physicians working in the ED and the SICU of the “M. Bufalini” Hospital received a theoretical course and practical training for the ultrasound-guided (USG) SAP block procedure, as the SAP block procedure was introduced in emergency care for the treatment of blunt chest trauma.
The SAP block course was organised as follows: each emergency physician took part in an 8-hour theoretical course and 4-hour practical training at the bedside, conducted by hospital anaesthetists experienced in the SAP block technique. USG-SAP block procedures were performed at the bedside in the ED or immediately after hospitalisation in the SICU. The SAP block was proposed to patients in the following cases: (i) patients aged > 18 years with chest trauma and severe pain, expressed as an NRS > 6; (ii) spontaneous breathing; (iii) more than two rib fractures; (iv) no haemodynamic instability; and (v) Glasgow Coma Scale > 13. Contraindications to SAP block were considered: (i) allergy to amide-type local anaesthetics, (ii) history of peripheral neuropathy, (iii) severe hepatic or renal insufficiency and (iv) infection at the injection site. During the SAP block, the patients were placed in supine or lateral positions. They underwent standard multiparametric monitoring, including non-invasive blood pressure, a three-lead electrocardiogram, and peripheral pulse oximetry. Sterile USG was performed using a portable ultrasound system (SonoSite M-Turbo; SonoSite Inc., WA, USA). A linear high-frequency probe (6–13 MHz) was placed in the midaxillary line to identify and scan the target ribs, latissimus dorsi, and serratus anterior muscles in the sagittal plane. A 50 mm long 22-gauge needle (Echoplex+, Vygon, Ecouen-France) was inserted into the fascial plane, and 70–100 mg of 7.5% ropivacaine (1-1.5 mg/kg) plus 0.9% saline up to 30 ml of total volume of was injected under direct vision. The linear spread of the local anaesthetic between the serratus anterior muscle and ribs (in case of deep SAP block) or between latissimus dorsi and serratus anterior muscles (in case of superficial SAP block) was directly observed to confirm the procedure. For bilateral rib fractures, SAP block was performed only on the most injured side. See Figs. 1, 2, 3, 4 and 5 for a detailed explanation of the technique.
The technique is performed by two operators: the first operator controls the ultrasound probe and the position of the needle within the fascial planes via ultrasound guidance, and the second operator alternately injects diluted saline or ropivacaine according to the first operator’s instructions. The saline is injected to confirm the correct position of the needle in the fascial space; once the proper location of the needle is confirmed, the injection of ropivacaine is performed
Image obtained with a high-frequency linear probe positioned as in Fig. 2: The red line indicates the thickness of the skin and subcutis; the yellow line indicates the thickness of the latissimus dorsi muscle; the green lines identify the serratus anterior muscle, which lies on the ribs; the blue line identifies the intercostal muscles; the white stars identify the ribs; the yellow arrow identifies the fascial plane between the latissimus dorsi and the serratus anterior, site of the superficial SAP block; the green arrow identifies the fascial plane between the serratus anterior muscle and the rib, site of the deep SAP block; the black star identifies presence of emphysema which prevents visualisation of deeper structures
illustrates the deep SAP block, in which the local anaesthetic is injected into the fascia below the serratus anterior muscle and the ribs. The red lines indicate the thickness of the skin and subcutis; the yellow lines indicate the thickness of the latissimus dorsi muscle; the green line identifies the serratus anterior muscle; the blue line identifies the intercostal muscles; the white star identifies the rib; the green arrow identifies the fascial plane between the serratus anterior muscle and the rib, site of the deep SAP block; the green star indicates the hydrodissection of the fascia below the serratus anterior, showing the spreading of the local anaesthetic between the serratus anterior and the rib; the black star identifies presence of emphysema which prevents visualisation of deeper structures
All patients were treated with analgesic therapy according to the World Health Organisation analgesic ladder for nociceptive pain: mild pain (level 1), non-opioids (paracetamol, non-steroidal anti-inflammatory drugs [NSAIDs]) ± adjuvants; moderate pain (level 2), weak opioids (tramadol) ± non-opioids ± adjuvants; and severe pain (level 3), strong opioids (morphine, fentanyl) ± non-opioids ± adjuvants [26]. Patients with pain due to rib fracture(s) who received analgesic therapy in combination with an SAP block were included in the SAP block group. In contrast, patients who received only analgesic treatment were included in the standard therapy alone group.
The primary endpoint of this study was the NRS pain score at 3, 6, 12, 18, and 24 h in the SAP block group compared to the standard therapy alone group. The secondary endpoints were (i) total opioid consumption in the first 24 h, (ii) pulmonary function expressed by SpO2/FiO2 ratio, and (iii) occurrence of adverse events in the USG SAPB plus standard therapy group compared to the standard therapy group alone.
Pain and opioid therapy were monitored and recorded in patients in the control group during the first 24 hours after admission to the ED and in patients in the SAP block group 24 hours after the SAP block was performed. Each patient’s 24-hour opioid consumption was converted to equivalent doses of intravenous morphine using an opioid conversion Table [27]. Pain was measured using an 11-point numerical rating scale (NRS), with 0 representing ‘no pain’ and 10 representing ‘worst pain ever”. Comorbidities were recorded using the Charlson Comorbidity Index (CCI) [28], trauma severity using the Injury Severity Score (ISS) [29], and Thoracic Trauma Severity Score (TTSS) [30]. Adverse events evaluated were: occurrence of pneumothorax due to SAP block; infections in the site of injection of the local anaesthetic, and occurrence of any sign or symptom compatible with the local Anaesthetic Systemic Toxicity (LAST) syndrome, including metallic taste, tremor, restlessness or drowsiness, seizures, cardiac arrhythmias, or cardiac arrest. The vital signs recorded were respiratory rate (RR), peripheral oxygen saturation (SpO2), SpO2/FiO2 ratio [31,32,33], systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) on admission and after 3, 6, 12, 18, and 24 hours. The decision to initiate oxygen therapy, high-flow nasal cannula oxygen therapy (HFNC), continuous positive airway pressure (CPAP) oxygen therapy, noninvasive ventilation (NIV), or orotracheal intubation was based on individual clinical judgment.
Continuous data are expressed as median and interquartile range; differences between two independent groups were compared using the Mann-Whitney U test, while the Wilcoxon test was used to compare two paired groups. Categorical data are expressed as absolute numbers and percentages; differences between two independent groups were compared using the Pearson chi-square test. Statistical analyses were performed using IBM SPSS version 25 (IBM Corp.) and MedCalc version 17.6 (MedCalc Software).
This study was conducted following the current Helsinki Declaration and approved by the local ethics committee, the “CET-CEROM—Comitato etico della Romagna”, dated December 13, 2023, approval code: 7379/2023. The STROBE checklist was used to prepare this manuscript [34].
Results
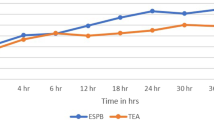
During the study period, 191 patients with chest trauma were admitted to the ED. However, 35 patients were excluded because they were admitted to the intensive care unit (ICU), 8 were sent home from the ED, 5 were admitted to the internal medicine department, and 3 were lost to follow-up (two patients were transferred to the surgical care unit, one after 6 h from admission and the other after 12 h, one patient was transferred to another hospital, and none of them underwent SAP block). Finally, 156 patients were included in the study, 102 of whom were male (65.4%), with a median age of 62 years (IQR 52–74) and a median CCI of 3 (IQR 1–5). In addition, 32 patients had bilateral rib fractures (20.5%), with a median of 6 fractured ribs (IQR 4–7), 4 (IQR 0–5) on the right side, and 4 (IQR 0–6) on the left side, with a median TTSS of 8 (IQR 6–9) and a median ISS of 16 (IQR 9–18). A total of 75 patients (48.2%) underwent USG SAP block in the ED. Patients who underwent SAP block had lower TTSS (7 [IQR 6–8] vs. 8 [7,8,9,10], p = 0.026) and higher NRS on admission (8 [8–9] vs. 7 [5,6,7,8], p < 0.001) than those who did not undergo the procedure. There were no differences in sex, median age, median CCI, ISS, vital signs, or the number of fractured ribs. Two patients developed severe respiratory failure during their stay in the SICU and underwent orotracheal intubation (1 in the SAP block group and 1 in the standard therapy group); two patients developed pneumonia (1 in the SAP block group and 1 in the standard therapy group); and no patient underwent IHM. Patients who underwent SAP block received a median dose of 80 mg ropivacaine (IQR 80–100), and none of the patients experienced a specific complication due to the administration of the local anaesthetic. Regarding the primary endpoint, patients who underwent SAP block had significantly less pain in the first 24 h than patients who underwent standard therapy only. As reported in Table 1; Fig. 6, at each time point considered, NRS was significantly lower in the SAP group than in the standard therapy-only group, except for NRS at 12 (p = 0.059) and 24 h (p = 0.458). Regarding the secondary endpoint, patients who underwent SAP block received significantly lower opioid doses (0 [0–20] MME vs. 20 [0–40] MME, p < 0.001). (see Fig. 6).
According to the respiratory function, patients who did not undergo SAP block showed a significant decrease in respiratory function during the first 24 h with an SpO2/FiO2 ratio of 392 [IQR 335–457] at admission vs. 325 [271–452] at 24 h, p 0.001, while those who underwent SAP block showed a stable SpO2/FiO2 ratio (412 [IQR 355–457] at admission vs. 457 [331–461] at 24 h, p 0.326), showing a higher SpO2/FiO2 ratio at each subsequent time point evaluated and requiring less frequent use of HFNC (3 [4] vs. 32 [39.5], p < 0.001). Evaluating only patients with bilateral rib fractures, the SAP block group showed a significant reduction in pain perception after 6 h (NRS = 4 [IQR 1–4], vs. NRS = 4 [IQR 3–5], p = 0.034) and after 12 h (median NRS = 4 [IQR 2–4], vs. median NRS = 4 [IQR 2–5], p = 0.045), whereby less MME was administered (median MME = 10 [IQR 0–20] vs. 20 [IQR 0–40], p < 0.001). For the general characteristics of the population included, see Table 1.
Discussion
The present study suggests that in adult traumatic patients with a median TTSS of 8 and a median ISS of 16 admitted to the SICU of the ED, USG SAP block, associated with standard therapy, is more effective than standard therapy alone in reducing pain during the first 24 h after block execution and at each time point, except at 12 and 24 h after enrolment. Moreover, SAP block was associated with a significantly lower dose of opioids administered and significantly better respiratory function, without differences in terms of adverse events compared to standard therapy alone. Although the 2011 Montreal Declaration [35] recognises the identification and treatment of pain as a fundamental human right, inadequate analgesia is a significant problem in the emergency department. Pain is the leading cause of admission to the ED, being associated with the main reason for admission in 61% of cases and the main reason for admission in up to 52.2% of cases [36]. Nevertheless, it is often underestimated and undertreated. In 1989, the term “oligoanalgesia” was introduced, which accurately describes how pain is frequently not adequately treated [37, 38]. As shown in the present study, a high proportion of admitted patients experience moderate to severe pain. In patients with rib fractures, the presence of pain severely restricts thoracic excursion and the ability to excrete secretions, leading to alveolar collapse and pulmonary atelectasis and increasing the risk of bacterial over-infection and patient death.
Traditional analgesics, such as paracetamol, NSAIDs, and opioids, are used to treat pain. However, paracetamol is only effective to a limited extent and is mainly used for mild pain. NSAIDs have numerous contraindications and adverse effects that are more common in elderly patients (renal insufficiency, concomitant treatment with antiplatelet agents or anticoagulants, and previous gastrointestinal bleeding). In contrast, opioids can lead to sedation, especially in frail patients. The use of low-dose ketamine (LDK) for analgesia is widespread [39], and there is also evidence for its use in trauma [40]. The SAP block has been successfully used to treat acute pain in multiple rib fractures [41]. In the current study, patients in the SAP block group achieved faster pain control than those in the standard therapy group (Fig. 1). They showed significantly better pain control at all time intervals except the 12- and 24-hour marks.
Although patients who underwent SAP block reported higher pain scores on admission, the patients in the SAP block group had significantly less pain just 3 h after admission. Achieving optimal pain control is essential for providing high-quality care to patients. The 2020 European Society of Emergency Medicine guidelines on managing acute pain in the emergency department recommend that no more than 25 min should be allowed for pain relief (if appropriate) [42]. Despite this, in the ED, pain management takes an average of 90 min [43], only 14–32% of patients receive adequate pain relief [41], and in 41% of patients, pain remains unchanged during the ED stay [43].
The SAP block is effective in less than 60 min [44]. However, recent studies have shown that the SAP block can reduce perceived pain by an average of 5 points (IQR ± 4) after 30 min [45], from 8/10 to 0/10 within 30 min [46], to 2/10 after 15 min [47], and a mean reduction in pain score of 6.8 within 10 min. The positive effect lasts up to 30 h and is contextually significant in improving respiratory function [48].
The SAP block provides analgesia while avoiding the systemic effects of other drugs, with an exclusively local effect [19, 49], greater efficacy than the traditional pharmacological approach [50], and a significant reduction in opioid consumption [51, 52]. It is worth noting that although performing a bilateral SAP block may be the better choice for patients with fractures of both ribs, patients with bilateral rib fractures also experienced better pain management and a reduced amount of medication for pain control despite a unilateral SAP block.
In addition, the SAP block has also been reported to be effective in allowing early and safe discharge of patients in whom hospitalisation would have been indicated only for pain control [53] and in reducing chronic pain after rib fractures [54]. Multimodal analgesic therapy based on both traditional approaches and local anaesthesia ensures the best outcome, especially in multiple rib fractures with secondary respiratory dysfunction [9, 55, 56], by significantly improving diaphragmatic excursion [57] and global pulmonary ventilatory function [45]. In the present study, patients who underwent SAP block showed a significantly higher SpO2/FiO2 ratio at each time point than those who did not undergo SAP block, in whom the SpO2/FiO2 ratio decreased significantly, requiring HFNC in a higher percentage of cases. As illustrated in Table 1, patients who did not undergo SAP block had a substantially higher proportion of pneumothorax and a higher TTSS, which can significantly affect the SpO2/FiO2 ratio and the need for respiratory support. However, no differences in the rates of pneumonia, orotracheal intubation, or in-hospital mortality were found between patients receiving SAP block and standard therapy and those receiving standard therapy alone. The effect of SAP block on pulmonary function needs further studies to be fully established. Moreover, the present study was not designed to show differences in the rates of these adverse events, and the lack of differences is likely due to the small number of patients included.
In addition, the use of fascial blocks in the ED may be particularly beneficial in different populations, including the elderly, where it has been shown to reduce the incidence of delirium in hospitals by up to 35 per cent [58], herpes zoster-related pain [59], burns [60], and thoracostomy [61].
The SAP block relies on detecting anatomical structures that are easily recognisable in ultrasound, as they are superficial structures, and these characteristics make the SAP block a straightforward fascial block to perform [62]. Two different approaches to performing the SAP block have been described: the superficial and deep approaches [18]. In the superficial approach, the local anaesthetic is injected into the virtual space between the serratus anterior and latissimus dorsi muscles. In contrast, in the deep approach, the local anaesthetic is injected into the space between the rib and serratus anterior. Theoretically, the superficial SAP block can be advantageous because the long thoracic nerve innervating the serratus anterior muscle is on its surface. Therefore, superficial SAP blocks can potentially block this nerve completely while also blocking the anterior branches of the intercostal nerves, as can deep SAP blocks. In contrast, deep SAP blocks cannot block the long thoracic nerve [63]. The superficial SAP block appears to have better analgesic efficacy in terms of pain scores, opioid consumption, time to first analgesic rescue and dermatomal spread in patients who have undergone mastectomy with axillary clearance [64] and in patients undergoing thoracoscopic surgery [63]. However, the clinical advantages of one approach over another are still controversial. Edwards et al. [65] and Piracha et al. [66] have demonstrated the superior efficacy of the deep SAP block. This is probably because it is easier to accurately locate the virtual space when the needle tip is placed above the ribs than the challenge of identifying the interfascial space between the latissimus dorsi and the serratus anterior to administer the local anaesthetic correctly.
Furthermore, the efficacy and safety of a fascial block depends on the specific type and dosage of the long-acting local anaesthetic used and the volume administered. The choice of local anaesthetic depends on factors such as the onset of action, duration of action, and the extent of motor blockade required. Rosenblatt et al. recommended 20 ml of 0.25% bupivacaine or 0.2% ropivacaine [67]. However, in the present study, the SAP blocks were performed with 30 ml of 0.23–0.33% ropivacaine. Ropivacaine is a longer-acting local anaesthetic that is less toxic than bupivacaine [68,69,70]. Although the recommended concentration is 0.2%, 0.33% allows for a faster onset of action [71].
Biswas et al. [72] showed that injecting a larger total volume of local anaesthesia leads to a broader and more consistent spread of anaesthesia, irrespective of the area injected. However, the clinical significance of these differences should be better clarified. In their randomised controlled trial, Kunigo et al. [73] demonstrated that the time until patients required the first analgesic rescue dose was comparable between patients receiving a total volume of 40 ml and those receiving a total volume of 20 ml, although a volume of 40 ml produced a greater area of sensory loss in the craniocaudal direction.
While this study highlights the efficacy of 30 ml of 0.23–0.33% ropivacaine for deep SAP block, further research is required to determine the effectiveness of using different volumes of long-acting local anaesthetic and the role of superficial or deep SAP blocks in the treatment of pain following rib fractures.
The SAP block is a relatively safe procedure. A recent meta-analysis by Jack et al. reported that SAP blocks did not result in adverse events compared to the control groups. In particular, no pneumothorax, nerve damage, hemorrhagic complications, infections, or Local Anaesthetic Systemic Toxicity (LAST) syndromes were noted, even in cases where they were performed in patients on anticoagulant therapy [74]. However, most of the studies included in the meta-analysis by Jack et al. investigated the role of the SAP block during thoracotomy or video-assisted thoracoscopic surgery, and the evidence for thoracic trauma included only case series and reports. The present retrospective study suggests that SAP block can be introduced into clinical practice after only a single theoretical and practical course. It appears to be a safe manoeuvre even in ED patients with multiple thoracic rib fractures [43, 60, 75]. Although the study was not designed to demonstrate the safety of SAP block due to the rare occurrence of local anaesthetics system toxicity (LAST) syndrome [71, 76], no adverse events were reported that could be associated with the administration of ropivacaine at the fascial site.
Recently, the SABRE randomised clinical trial confirmed the efficacy and safety of SAP block performed in the ED in terms of pain control, opioid reduction, and SAP block-related adverse events. Despite the trial reporting no data on the effect of SAP block on respiratory function, no significant differences were noted regarding secondary pneumonia, length of stay, or 30-day mortality. However, the trial was not conceived to detect differences in these important outcomes, and subsequent studies are needed to explore these crucial aspects [77].
This study has several limitations, including a non-randomised design in a single trauma centre, recruitment limited by exclusion criteria, and the availability of an emergency physician able to perform the SAP block. Moreover, formal sample size was not calculated, and the lack of differences between the two groups may be related to the small number of patients included. The time study was limited to the first 24 h. It included patients regardless of the thoracic region in which the fractures were localised (including unilateral and bilateral rib fractures) and irrespective of the presence of other injured areas. Despite these data showing an improvement in pain perception with less need for MME, the results may differ in cases of bilateral USG-SAP blocks or patients with only thoracic injuries, especially regarding MME required to achieve adequate pain management and overall complications. The control group had a higher TTSS, and the SAP block group had significantly higher pain scores (NRS) at baseline. Still, despite this data, patients treated with SAP block significantly improved their pain scores.
Moreover, the administration of prehospital analgesia was not reported, which may have influenced the NRS reported at admission and 3 h after inclusion and the total dose of opioids administered in both groups. The present study is also limited to controlling for the placebo effect of the SAP block. In addition to the inclusion and exclusion criteria, several other factors may have influenced the selection of patients who underwent SAP block. These factors could include patient preferences and the emergency physician’s experience level, potentially introducing selection bias. Additional randomised prospective studies are necessary to establish definitive conclusions regarding the efficacy and safety of SAP block. This study reflects the experience of a single centre, in which patients were treated by different emergency physicians after a single course. Despite the safety and relative ease with which the manoeuvres can be performed, continuous training is essential for maintaining and improving skills. Subsequently, various studies are required to determine the best training system and ability to perform the SAP block over time.
Conclusions
Serratus anterior plane block, or SAP block, performed by emergency physicians in the emergency department in conjunction with standard therapy in patients with severe pain due to traumatic rib fractures, appeared to be more effective than standard therapy alone in relieving pain at 3, 6, and 18 h after a single block, with a significantly lower amount of opioid required to achieve adequate analgesia, allowing for better respiratory function, and no adverse events reported.
In conclusion, integrating the SAP block into multimodal analgesic therapy in the emergency department could be a safe and efficient approach for pain management in patients with multiple rib fractures.
Data availability
No datasets were generated or analysed during the current study.
References
1, Easter A. Management of patients with multiple rib fractures. Am J Crit Care. 2001;10(5):320–7. quiz 328-9. PMID: 11548565.
Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients-still a relevant problem? Scand J Trauma Resusc Emerg Med. 2017;25(1):1–6.
Coary R, Skerritt C, Carey A, Rudd S, Shipway D. New horizons in rib fracture management in the older adult. Age Ageing. 2020;49(2):161–7. https://doi.org/10.1093/ageing/afz157.
Simon B, Ebert J, Bokhari F, et al. Management of pulmonary contusion and flail chest: an Eastern Association for the surgery of trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S351–61. https://doi.org/10.1097/TA.0b013e31827019fd.
Karmakar MK, Ho AM. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54(3):615– 25. https://doi.org/10.1097/01.TA.0000053197.40145.62. PMID: 12634549.
Unsworth A, Curtis K, Asha SE. Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scand J Trauma Resusc Emerg Med. 2015;23:17. https://doi.org/10.1186/s13049-015-0091-5. PMID: 25887859; PMCID: PMC4322452.
Bouzat P, Raux M, David JS, Tazarourte K, Galinski M, Desmettre T, Garrigue D, Ducros L, Michelet P; Expert’s group;, Freysz M, Savary D, Rayeh-Pelardy F, Laplace C, Duponq R, Monnin Bares V, D’Journo XB, Boddaert G, Boutonnet M, Pierre S, Léone M, Honnart D, Biais M, Vardon F. Chest trauma: First 48hours management. Anaesth Crit Care Pain Med. 2017;36(2):135–145. doi: 10.1016/j.accpm.2017.01.003. Epub 2017 Jan 16. PMID: 28096063.
Battle CE, De Iaco H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury. 2012;43:8–17.
Galvagno SM Jr, Smith CE, Varon AJ, Hasenboehler EA, Sultan S, Shaefer G, To KB, Fox AD, Alley DE, Ditillo M, Joseph BA, Robinson BR, Haut ER. Pain management for blunt thoracic trauma: a joint practice management guideline from the Eastern Association for the surgery of Trauma and Trauma Anesthesiology Society. J Trauma Acute Care Surg. 2016;81(5):936–51. https://doi.org/10.1097/TA.0000000000001209. PMID:27533913.
Moon MR, Luchette FA, Gibson SW, Crews J, Sudarshan G, Hurst JM, et al. Prospective randomised comparison of epidural versus parenteral opioid analgesia in thoracic trauma. Ann Surg. 1999;229:684–91.
Bulger EM, Edwards T, Klotz P, Jurkovich GJ. Epidural analgesia improves outcome after multiple rib fractures. Surgery. 2004;136:426–30.
Mackersie RC, Karagianes TG, Hoyt DB, Davis JW. Prospective evaluation of epidural and intravenous administration of fentanyl for pain control and restoration of ventilatory function following multiple rib fractures. J Trauma. 1991;31:443–9.
Ullman DA, Fortune JB, Greenhouse BB, Wimpy RE, Kenedy TM. The treatment of patients with multiple rib fractures using continuous thoracic epidural narcotic infusion. Reg Anesth. 1989;14:43–7.
Brasel KJ, Moore EE, Albrecht RA, et al. Western Trauma Association Critical Decisions in trauma: management of rib fractures. J Trauma Acute Care Surg. 2017;82(1):200–3. https://doi.org/10.1097/TA.0000000000001301.
Simon JB, Wickham AJ. Blunt chest wall trauma: an overview. Br J Hosp Med (Lond). 2019;80(12):711–715. https://doi.org/10.12968/hmed.2019.80.12.711. PMID: 31822181.
Ingalls NK, Horton ZA, Bettendorf M, Frye I, Rodriguez C. Randomized, double-blind, placebo-controlled trial using lidocaine patch 5% in traumatic rib fractures. J Am Coll Surg. 2010;210(2):205–9.
Shams D, Sachse K, Statzer N, Gupta RK. Regional Anesthesia complications and contraindications. Clin Sports Med. 2022;41(2):329–43. https://doi.org/10.1016/j.csm.2021.11.006.
Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107–13. https://doi.org/10.1111/anae.12344.
Southgate SJ, Herbst MK. Ultrasound-guided Serratus Anterior blocks. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 25, 2022.
Helander EM, Webb MP, Kendrick J, et al. PECS, serratus plane, erector spinae, and paravertebral blocks: a comprehensive review. Best Pract Res Clin Anaesthesiol. 2019;33(4):573–81. https://doi.org/10.1016/j.bpa.2019.07.003.
Mayes J, Davison E, Panahi P, et al. An anatomical evaluation of the serratus anterior plane block. Anaesthesia. 2016;71(9):1064–9. https://doi.org/10.1111/anae.13549.
Kim DH, Kim SJ, Liu J, Beathe J, Memtsoudis SG. Fascial plane blocks: a narrative review of the literature. Reg Anesth Pain Med. 2021;46(7):600–17. https://doi.org/10.1136/rapm-2020-101909.
Chin KJ, Versyck B, Pawa A. Ultrasound-guided fascial plane blocks of the chest wall: a state-of-the-art review. Anaesthesia. 2021;76(Suppl 1):110–26. https://doi.org/10.1111/anae.15276.
Almeida CR. Serratus anterior plane block for posterior rib fractures: why and when may it work? Reg Anesth Pain Med. 2021;46(9):835–6. https://doi.org/10.1136/rapm-2020-102098.
Cheema FA, Chao E, Buchsbaum J, et al. State of Rib Fracture Care: a NTDB Review of Analgesic Management and Surgical stabilization. Am Surg. 2019;85(5):474–8.
Anekar AA, Hendrix JM, Cascella M. WHO Analgesic Ladder. [Updated 2023 Apr 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK554435/.
De Iaco F, Mannaioni G, Serra S, Finco G, Sartori S, Gandolfo E, Sansone P, Marinangeli F. Equianalgesia, opioid switch and opioid association in different clinical settings: a narrative review. Eur Rev Med Pharmacol Sci. 2022;26(6):2000–17. doi: 10.26355/eurrev_202203_28349. PMID: 35363351.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Daurat A, Millet I, Roustan JP, et al. Thoracic trauma severity score on admission allows to determine the risk of delayed ARDS in trauma patients with pulmonary contusion. Injury. 2016;47(1):147–53. https://doi.org/10.1016/j.injury.2015.08.031.
Babu S, Abhilash KP, Kandasamy S, Gowri M. Association between SpO2/FiO2 ratio and PaO2/FiO2 ratio in different modes of Oxygen Supplementation. Indian J Crit Care Med. 2021;25(9):1001–5. https://doi.org/10.5005/jp-journals-10071-23977.
Catoire P, Tellier E, de la Rivière C, et al. Assessment of the SpO2/FiO2 ratio as a tool for hypoxemia screening in the emergency department. Am J Emerg Med. 2021;44:116–20. https://doi.org/10.1016/j.ajem.2021.01.092.
Bonaventura A, Mumoli N, Mazzone A, et al. Correlation of SpO2/FiO2 and PaO2/FiO2 in patients with symptomatic COVID-19: an observational, retrospective study. Intern Emerg Med. 2022;17(6):1769–75. https://doi.org/10.1007/s11739-022-02981-3.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008.
https://www.apsoc.org.au/PDF/Publications/DeclarationOfMontreal_IASP.pdf.
Cordell WH, Keene KK, Giles BK, Jones JB, Jones JH, Brizendine EJ. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20(3):165–9. https://doi.org/10.1053/ajem.2002.32643.
Calil AM, Pimenta CA, Birolini D. The oligoanalgesia problem in the emergency care. Clin (Sao Paulo). 2007;62(5):591–8. https://doi.org/10.1590/s1807-59322007000500010.
Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department. Am J Emerg Med. 1989;7(6):620–3. https://doi.org/10.1016/0735-6757(89)90286-6.
Riccardi A, Guarino M, Serra S, et al. Narrative review: low-dose ketamine for Pain Management. J Clin Med. 2023;12(9):3256. https://doi.org/10.3390/jcm12093256. Published 2023 May 2.
Fabbri A, Voza A, Riccardi A, Serra S, Iaco F, Study and Research Center of the Italian Society of Emergency Medicine (SIMEU). The Pain Management of Trauma patients in the Emergency Department. J Clin Med. 2023;12(9):3289. https://doi.org/10.3390/jcm12093289. Published 2023 May 5.
Southgate SJ, Herbst MK. Ultrasound guided serratus anterior blocks. [Updated 2019 Mar 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019. https://www.ncbi.nlm.nih.gov/books/NBK538476/. [Last accessed on 2019 Aug 04].
Hachimi-Idrissi S, Coffey F, Hautz WE, et al. Approaching acute pain in emergency settings: European Society for Emergency Medicine (EUSEM) guidelines-part 1: assessment. Intern Emerg Med. 2020;15(7):1125–39. https://doi.org/10.1007/s11739-020-02477-y.
Todd KH, Ducharme J, Choiniere M, et al. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8(6):460–6. https://doi.org/10.1016/j.jpain.2006.12.005.
Schnekenburger M, Mathew J, Fitzgerald M, Hendel S, Sekandarzad MW, Mitra B. Regional anaesthesia for rib fractures: a pilot study of serratus anterior plane block. Emerg Med Australas. 2021;33(5):788–93. https://doi.org/10.1111/1742-6723.13724.
Paul S, Bhoi SK, Sinha TP, Kumar G. Ultrasound-guided Serratus Anterior Plane Block for Rib Fracture-Associated Pain Management in Emergency Department. J Emerg Trauma Shock. 2020;13(3):208–12. https://doi.org/10.4103/JETS.JETS_155_19.
Durant E, Dixon B, Luftig J, Mantuani D, Herring A. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med. 2017;35(1):197e. 3-197.e6.
Jadon A, Jain P, Sinha N, Agrawal A. Serratus anterior plane block for pain relief in multiple fractured ribs (MFRs); injection of local anesthetic above the serratus or below the serratus anterior muscle– a case report. Anesth Med Pract J. 2016:G103.
Schettino F, Coletta F, Sala C, Tomasello A, De Simone A, Santoriello E, Mainini M, Cotena S, Di Bari S, Villani R. Serratus plane block and erector spinae plane block in the management of pain associated with rib fractures in chest trauma: a brief report from a single-center. Acute Care Med Surg Anesth. 2023;1(1). https://doi.org/10.4081/amsa.2023.11.
Thiruvenkatarajan V, Cruz Eng H, Adhikary SD. An update on regional analgesia for rib fractures. Curr Opin Anaesthesiol. 2018;31(5):601–7. https://doi.org/10.1097/ACO.0000000000000637.
Ho AM, Karmakar MK, Critchley LA. Acute pain management of patients with multiple fractured ribs: a focus on regional techniques. Curr Opin Crit Care. 2011;17(4):323–7. https://doi.org/10.1097/MCC.0b013e328348bf6f.
Kring RM, Mackenzie DC, Wilson CN, Rappold JF, Strout TD, Croft PE. Ultrasound-guided Serratus Anterior Plane Block (SAPB) improves Pain Control in patients with Rib fractures. J Ultrasound Med. 2022;41(11):2695–701. https://doi.org/10.1002/jum.15953.
Abdelhamid K, ElHawary H, Turner JP. The Use of the Erector Spinae Plane Block to decrease Pain and Opioid Consumption in the Emergency Department: A literature review. J Emerg Med. 2020;58(4):603–9. https://doi.org/10.1016/j.jemermed.2020.02.022.
Lee JB, Nelson A, Lahham S. Serratus anterior plane block as a bridge to outpatient management of severe rib fractures: a case report. Clin Exp Emerg Med. 2022;9(2):155–9. https://doi.org/10.15441/ceem.20.087.
Tekşen Ş, Öksüz G, Öksüz H, et al. Analgesic efficacy of the serratus anterior plane block in rib fractures pain: a randomized controlled trial. Am J Emerg Med. 2021;41:16–20. https://doi.org/10.1016/j.ajem.2020.12.041.
Martin TJ, Eltorai AS, Dunn R, et al. Clinical management of rib fractures and methods for prevention of pulmonary complications: a review. Injury. 2019;50(6):1159–65. https://doi.org/10.1016/j.injury.2019.04.020.
De Iaco F, Gandolfo E, Guarino M, Riccardi A, Serra S. Terapia Del Dolore in Urgenza E Sedazione Procedurale: Manuale SAU, 2022.
El Malla DA, Helal RAEF, Zidan TAM, El Mourad MB. The Effect of Erector Spinae Block versus Serratus Plane Block on Pain scores and diaphragmatic excursion in multiple Rib fractures. A prospective Randomized Trial. Pain Med. 2022;23(3):448–55. https://doi.org/10.1093/pm/pnab214.
O’Connell KM, Patel KV, Powelson E, et al. Use of regional analgesia and risk of delirium in older adults with multiple rib fractures: an Eastern Association for the surgery of Trauma multicenter study. J Trauma Acute Care Surg. 2021;91(2):265–71. https://doi.org/10.1097/TA.0000000000003258.
Goldsmith AJ, Liteplo AS, Shokoohi H. Ultrasound-guided Serratus Anterior Plane Block for intractable herpes Zoster Pain in the Emergency Department. J Emerg Med. 2020;59(3):409–12. https://doi.org/10.1016/j.jemermed.2020.04.053.
Benesch T, Mantuani D, Nagdev A. Case Report: bilateral ultrasound-guided Serratus Anterior Plane blocks for a chest wall burn. Clin Pract Cases Emerg Med. 2021;5(1):117–20. https://doi.org/10.5811/cpcem.2020.12.50184.
Lin J, Hoffman T, Badashova K, Motov S, Haines L. Serratus Anterior Plane Block in the Emergency Department: a Case Series. Clin Pract Cases Emerg Med. 2020;4(1):21–5. https://doi.org/10.5811/cpcem.2019.11.44946. Published 2020 Jan 21.
Xie C, Ran G, Chen D, Lu Y. A narrative review of ultrasound-guided serratus anterior plane block. Ann Palliat Med. 2021;10(1):700–6. https://doi.org/10.21037/apm-20-1542.
Qiu L, Bu X, Shen J, et al. Observation of the analgesic effect of superficial or deep anterior serratus plane block on patients undergoing thoracoscopic lobectomy. Med (Baltim). 2021;100(3):e24352. https://doi.org/10.1097/MD.0000000000024352.
Tan KW, Sayed Masri SNN, Musthafa QA, et al. Analgesic efficacy of the superficial versus deep serratus plane blocks for mastectomy with axillary clearance: a randomized controlled trial. Med (Baltim). 2022;101(35):e30515. https://doi.org/10.1097/MD.0000000000030515.
Edwards JT, Langridge XT, Cheng GS, McBroom MM, Minhajuddin A, Machi AT. Superficial vs. deep serratus anterior plane block for analgesia in patients undergoing mastectomy: a randomized prospective trial. J Clin Anesth. 2021;75:110470. https://doi.org/10.1016/j.jclinane.2021.110470.
Piracha MM, Thorp SL, Puttanniah V, Gulati A. A tale of two Planes: deep versus superficial Serratus Plane Block for Postmastectomy Pain Syndrome. Reg Anesth Pain Med. 2017;42(2):259–62. https://doi.org/10.1097/AAP.0000000000000555.
Rosenblatt M. Thoracic nerve block techniques. In: UpToDate, Post TW, editorAccessed December 30, UpToDate, Waltham, MA. (2023).
Scott DB, Lee A, Fagan D, Bowler GM, Bloomfield P, Lundh R. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg. 1989;69(5):563–9.
Knudsen K, Beckman Suurküla M, Blomberg S, Sjövall J, Edvardsson N. Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78(5):507–14. https://doi.org/10.1093/bja/78.5.507.
Guinet P, Estebe JP, Ratajczak-Enselme M, et al. Electrocardiographic and hemodynamic effects of intravenous infusion of bupivacaine, ropivacaine, levobupivacaine, and lidocaine in anesthetized ewes. Reg Anesth Pain Med. 2009;34(1):17–23. https://doi.org/10.1097/AAP.0b013e31819338e2.
Warren L, Pak A. Local anesthetic systemic toxicity. In: UpToDate, Post TW, editorAccessed December 30, UpToDate, Waltham, MA. (2023).
Biswas A, Castanov V, Li Z, et al. Serratus Plane Block: a cadaveric study to evaluate optimal Injectate Spread. Reg Anesth Pain Med. 2018;43(8):854–8. https://doi.org/10.1097/AAP.0000000000000848.
Kunigo T, Murouchi T, Yamamoto S, Yamakage M. Injection volume and Anesthetic Effect in Serratus Plane Block. Reg Anesth Pain Med. 2017;42(6):737–40. https://doi.org/10.1097/AAP.0000000000000649.
Jack JM, McLellan E, Versyck B, Englesakis MF, Chin KJ. The role of serratus anterior plane and pectoral nerves blocks in cardiac surgery, thoracic surgery and trauma: a qualitative systematic review. Anaesthesia. 2020;75(10):1372–85. https://doi.org/10.1111/anae.15000.
Martinez T, Belveyre T, Lopez A, et al. Serratus Plane Block is effective for Pain Control in patients with Blunt chest trauma: a Case Series. Pain Pract. 2020;20(2):197–203. https://doi.org/10.1111/papr.12833.
Wolfe JW, Butterworth JF. Local anesthetic systemic toxicity: update on mechanisms and treatment. Curr Opin Anaesthesiol. 2011;24(5):561–6. https://doi.org/10.1097/ACO.0b013e32834a9394.
Partyka C, Asha S, Berry M, et al. Serratus Anterior Plane blocks for Early Rib Fracture Pain Management: the SABRE Randomized Clinical Trial. JAMA Surg Published Online May. 2024;1. https://doi.org/10.1001/jamasurg.2024.0969.
Acknowledgements
The authors want to thank the Study and Research Center of the Italian Society for Emergency Medicine (SIMEU), Italy for their support and involvement in this study, and for their collaboration in the infrastructures, consumables and inventoriable material necessary to carry out the study.
Funding
This research received no external funding.
Open access funding provided by Università degli Studi di Ferrara within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Conceptualization, Sossio Serra, Domenico Pietro Santonastaso and Giuseppe Romano; Data curation, Michele Domenico Spampinato; Formal analysis, Michele Domenico Spampinato; Investigation, Sossio Serra, Giuseppe Romano, Stefano Geniere Nigra, Emanuele Russo and Mario Angelini; Methodology, Michele Domenico Spampinato; Project administration, Sossio Serra; Resources, Raffaella Francesconi and Fabio De Iaco; Software, Michele Domenico Spampinato; Supervision, Raffaella Francesconi and Fabio De Iaco; Validation, Alessandro Riccardi, Emanuele Russo, Mario Angelini and Vanni Agnoletti; Visualization, Fabio De Iaco; Writing– original draft, Sossio Serra, Domenico Pietro Santonastaso, Giuseppe Romano and Mario Angelini; Writing– review & editing, Alessandro Riccardi, Mario Guarino, Claudia Sara Cimmino and Michele Domenico Spampinato. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Raffella Francesconi and Fabio De Iaco Co-last authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Serra, S., Santonastaso, D.P., Romano, G. et al. Efficacy and safety of the serratus anterior plane block (SAP block) for pain management in patients with multiple rib fractures in the emergency department: a retrospective study. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02597-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02597-6