Abstract
Purpose
Sarcopenia, defined as the loss of muscle mass and strength, can hinder postoperative recovery and raise mortality rates. However, the current evidence on the harmful effects of sarcopenia in older patients in orthopedic and trauma care is unclear. This scoping review investigates different definitions that were used for the diagnosis of sarcopenia in older patients in orthopedic and trauma care and what adverse consequences have been examined.
Methods
We performed a comprehensive literature search in PubMed and Embase, following the PRISMA guidelines. We included original studies that examined clinical outcomes (such as length of hospital stay, rate of non-home discharge, rate of subsequent falls, rate of refractures, mortality, and functional outcome/quality of life) in older patients in orthopedic and trauma care (aged 65 years and above) with diagnosed sarcopenia (S) compared to a group without sarcopenia (NS).
Results
Our search identified 2,748 publications. Out of these, 23 articles met the inclusion criteria. Most publications were from Asia (n = 13). A total of 6174 patients were examined, with a prevalence of sarcopenia in 14–92%. 11 articles focused on patients with hip joint pathologies. Most studies diagnosed sarcopenia according to the Asian Working Group on Sarcopenia (AWGSOP1 or AWGSOP2) definitions (n = 10). Length of hospital stay was investigated in 13 studies. Seven studies assessed rates of non-home discharge rates. Subsequent falls were not investigated in any of the studies. 1 study reported the overall refracture rate (S: 10.4%; NS: 5.8%). Mortality was assessed in 11 studies (S: 1–60.5%; NS: 0–39.5%). The functional outcome/quality of life was investigated by 17 studies (Barthel Index decline S: -4.5 to -15.3 points; NS: -11.7 to -54.7 points).
Conclusion
Sarcopenia has been increasingly studied in older patients in orthopedic and trauma care but there is a lack of consistent definition criteria. This scoping review suggests that sarcopenia may be associated with prolonged length of stay, higher rates of non-home discharge, and increased mortality among older patients in orthopedic and trauma care. However, prospective studies are necessary to establish the relationship between sarcopenia and refractures, falls, and functional outcome/quality of life among older patients in orthopedic and trauma care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcopenia is characterized by a decline of muscle mass and strength and is prevalent in 10–27% of individuals over 60 years old [1]. Despite the heightened interest in sarcopenia research, as illustrated by the annual increase of 18% in the global literature since 2000, the diagnosis of sarcopenia is still highly inconsistent and underestimated [2, 3]. At regular intervals, international consortia have proposed and updated different definitions and reference values of sarcopenia for American (Foundation for the National Institutes of Health, FNIH1/2), Asian (Asian working group for sarcopenia, AWGS1/2), and European (European working group for sarcopenia, EWGSOP1/2) populations (Table 1) [4,5,6]. However, the fundamental criterion shared among these definitions is the presence of both low muscle mass (e.g., skeletal muscle mass assessed using bioelectric impedance analysis) and strength (e.g., handgrip strength assessed using a dynamometer). A recent systematic review found that orthopedic patients with low muscle mass and strength experience hindered recovery and heightened postoperative mortality, particularly in cases requiring emergency surgery [7]. Concordantly, in the orthogeriatric context, sarcopenia has been recently shown to be a univariate predictor of survival [8]. Yet, the global evidence regarding functional decline, rates of institutionalizations, subsequent falls, fractures, and mortality specifically in geriatric patients in orthopedic and trauma care suffering from sarcopenia is currently unclear. Consequentially, the purpose of our study was to conduct a scoping review to investigate the diagnostic definitions and adverse outcomes of sarcopenia, specifically in the field of orthogeriatrics.
Methods
Prior to undertaking this review, an a priori research protocol was developed. The scoping review was performed according to the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews guidelines’ (PRISMA-SCr) [9]. Two reviewers (JG and SK) independently screened the literature in a systematic approach to filter relevant articles for this scoping review. Discrepancies were resolved by discussion and involvement of a third party where necessary.
The databases of PubMed and Embase were searched using the dedicated search string ‘sarcopen* AND orthop* OR sarcopen* AND fracture’ up to 2023–08-20. We included original articles investigating patients aged ≥ 65 years (acutely) hospitalized with an orthopedic (trauma) diagnosis. We included studies with and without orthogeriatric co-management. Included articles had to report on at least one sarcopenic (sub-) group and one control group. A diagnostic definition of sarcopenia had to be outlined. Articles were included if they investigated adverse outcomes associated to sarcopenia according to the paper by Stuck AK et al. [10] including length of hospital stay, the rate of non-home discharge (nursing home, long-term care), the rate of subsequent falls, the rate of subsequent refractures, functional outcome/quality of life, or mortality. Only original articles published in English, French, or German were considered in this review.
Reviews, meta-analyses, animal studies, editorials, comments, and letters were excluded as well as studies in languages other than English, French, or German. Studies investigating cohorts with specific underlying diseases such as malignancy, rheumatoid arthritis, M. Parkinson, or HIV were also excluded.
Data was extracted from full-text assessment and from published supplemental material whenever available. Data extraction covered information on the study population (origin of the study, existence of orthogeriatric co-management, injury localization, demographic parameters), definition criteria for sarcopenia (methods and reference values), and outcome parameters (length of hospital stay, rate of non-home discharge, rate of subsequent falls, rate of refractures, mortality, functional outcome/quality of life).
Statistical analyses and graphing were performed using ‘R’ (R Core Team, Version 4.1.0; R Foundation for Statistical Computing, Vienna, Austria) and GraphPad Prism (Version 9.5 (2023); GraphPad Software, La Jolla, CA, USA). Descriptive statistics were obtained for relevant items. Odds ratios and 95% confidence intervals (CI) were calculated for sarcopenic and non-sarcopenic subgroups.
Results
Literature search and study characteristics
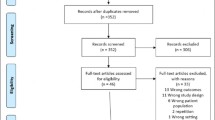
Our literature search identified 3183 records. After duplicate removal, 2748 records were screened. Of these, 221 full-text articles were assessed for eligibility leaving 23 studies with a cumulative number of 6174 patients included in this scoping review (Fig. 1). Included study types were 10 prospective and 13 retrospective case control, cohort, and cross-sectional studies. Three studies reported an orthogeriatric co-management. All studies were published between 2016 and 2020. Follow up time of included studies ranged from 6 to 48 months.
Flow diagram indicating the literature identification pathway resulting in the inclusion of 23 original articles according to the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’(PRISMA) guidelines. *—Investigations into sarcopenia within cohorts affected by specific underlying diseases (e.g., malignancy, rheumatoid arthritis, Parkinson's disease, HIV), studies in basic science, and studies that were not pertinent to the research inquiries
Study populations
Studies investigating adverse outcomes associated to sarcopenia in orthopedics primarily originated from Asia (n = 13), followed by Europe (n = 8) and the US (n = 2) (Fig. 2a). Cohort sizes ranged between 36 and 661 patients (Fig. 2b). The mean age of the underlying populations ranged between 68 and 88 years. In 20 studies, a predominantly female population was investigated (54–80%). Nine studies recorded the pre-hospitalization residential status (0–29% institutionalized before hospital admission). The injury/disease localization was predominantly the hip region (n = 11 studies), followed by the spine (n = 8) (Table 2). Most studies evaluated traumatic injuries (n = 17). Patients undergoing elective surgery without prior trauma were investigated in five studies in knee and spine patients, respectively.
Diagnostic criteria of sarcopenia
Overall, the prevalence of sarcopenia ranged between 14 and 92% (Fig. 2a). Assessment criteria, methodological approaches, and reference values to diagnose sarcopenia varied between studies (Tables 1 and 2). Most studies (n = 10) defined sarcopenia relying on one single parameter, of which low muscle mass was the most used criterion (n = 6). Sarcopenia was defined according to the criteria of AWGS1 in 10 studies, followed by the EWGSOP1 (n = 4), EWGSOP2 (n = 3), and AWGSOP2 (n = 2; Fig. 3). Four studies did not adhere to the working group consensus criteria for diagnosing sarcopenia (Table 2).
Length of stay
Length of hospital stay was evaluated in 13 studies (Fig. 4). The average length of stay ranged between 5.6 and 35.3 days in sarcopenic patients (Table 3). In the non-sarcopenic study groups, the average length of stay ranged between 5.2 and 32.5 days. Ten of 13 studies evaluating length of stay reported a trend towards a prolonged stay in the sarcopenic group compared to the non-sarcopenic group (Table 3). However, only four studies showed significant differences (p < 0.05).
Rate of non-home discharge
Seven studies assessed the discharge destination (Table 3). Non-home discharge (re- institutionalization to nursing home, rehabilitation unit or long-term care) was necessary in 12 to 79% of patients with sarcopenia with an odds ratio ranging between 1.1 and 3.2 compared to patients without sarcopenia (17–68% non-home discharge). Gonzalez-Montalvo et al. had an in-depth look at the discharge destination in older patients in orthopedic and trauma care sustaining hip fractures [13]. Prior to the injury, patients with sarcopenia were more likely to live in nursing homes. However, discharge destinations were similar and rates of re-institutionalization nursing home, rehabilitation unit, long-term care were high in both, sarcopenic and non-sarcopenic groups (77% and 68%, respectively).
Rate of subsequent falls
Subsequent falls have not been assessed by any of the studies reviewed.
Rate of refractures
The overall refracture rate was assessed in only one publication (Table 3). Among 201 sarcopenic patients with hip fractures, Steihaug et al. detected an overall refracture rate of 10% (OR: 1.9; CI 0.66 – 5.12) [30]. Two studies reported on specific refractures: Chen et al. reported on vertebral refractures among 214 sarcopenic patients after percutaneous kyphoplasty and found a vertebral refracture rate of 84% (OR: 42.5; 95%CI 18 – 95.2) [12]. In addition, Ohayama et al. investigated the risk of adjacent vertebral fractures in patients suffering an osteoporotic spinal fracture [25]. They report on a prevalence of 39% of adjacent vertebral fractures (OR: 0.83; CI: 0.29 – 2.5).
Mortality
Seven of eleven publications assessing overall mortality reported on one-year mortality (Table 3) ranging between 1 and 46%. Corresponding Odds ratios ranged between 1 (0.5–1.4) and 6.87 (2.2–19.2) with a higher risk of one-year mortality for sarcopenic patients.
Functional outcome and quality of life
The functional outcome/quality of life has been described in 14 articles (Table 3). The Barthel Index was the most frequently used score (n = 5). Compared to the non-sarcopenic groups, four articles reported decline of function in the sarcopenic groups (Barthel Index -4.5 to -15.3 points).
Besides the Barthel Index, a variety of patient related outcome measurements (PROMs) were examined in the included studies (Table 3): Two out of three studies examining gait speed demonstrated slower gait in their sarcopenic subgroups. All three studies assessing the Japanese Orthopaedic Association Score showed inferior results in their sarcopenic subgroups. Two studies evaluated the EQ-5D score, with one indicating poorer values in the sarcopenic subgroup. Similarly, two studies investigated the 36-Item Short Form Health Survey score, with one revealing lower values in the sarcopenic subgroup. One of the two studies investigating the New Mobility Score reported worse outcomes in the sarcopenic subgroup, while both studies noted a similar change in NMS from pre- to postoperatively. One study found no difference in Activities of Daily Living scores between sarcopenic and non-sarcopenic groups. Another study explored the rate of patients regaining prefracture walking ability and identified a lower rate in the sarcopenic subgroup.
Discussion
This scoping review provides a reconnoitering mapping of the available original literature elaborating on clinical outcome categories in defined sarcopenic and orthogeriatic patients. Through our investigation, we have identified several research gaps related to geographic and demographic subpopulations, the assessment and definition of sarcopenia, and the adverse events associated with sarcopenia in orthogeriatrics.
To the best of our knowledge, this study is the first scoping review conducted to investigate the available evidence on the assessment of sarcopenia and comprehensive evaluation of adverse outcomes in older patients in orthopedic and trauma care who are hospitalized. Previous systematic reviews on sarcopenia in orthopedic patients have included younger patients and focused on mortality or postoperative functional recovery after hip, spine, or distal radius surgeries [7, 33,34,35,36,37,38,39].
More than half of the current body of research on sarcopenia in older patients in orthopedic and trauma care is derived from populations in eastern Asia. Thus, according to the origin of most of the studies included, it is not surprising that the assessment criteria and reference values of the AWGS were used in most of the studies included in this review.
The published working group consensus criteria exhibit notable discrepancies. For instance, the EWGSOP2 algorithm requires the presence of both low muscle strength and low muscle mass for a sarcopenia diagnosis, while the EWGSOP1 criteria consider either low muscle mass or low muscle strength. Moreover, there are variations in the reference values across the working group criteria. For example, in women, low muscle strength according to the FNIH2 criteria corresponds to only 80% of the low muscle strength defined by the EWGSOP1 criteria (Table 1). Consequently, Stuck et al. demonstrated that the prevalence of sarcopenia varies significantly (1%—17%) in a cohort of 1495 community-dwelling participants based on the sarcopenia definition employed [40]. Similarly, Kim et al. reported a disparity in sarcopenia prevalence (2%—28%) depending on the underlying definition [41]. As highlighted by Bischoff-Ferrari et al., these discrepancies in prevalence may introduce biases in causal relationship analyses, as different sarcopenia definitions do not equally predict sarcopenia-related complications [42]. Considering the diverse age groups, procedural interventions (trauma vs. elective cases), anatomical regions assessed, and the geographic diversity of study populations, the heterogeneous nature of sarcopenia diagnostics precludes a robust meta-analysis.
Interestingly, despite well-established elements for sarcopenia assessments, four studies did not use such consensus criteria. Instead, three studies calculated a psoas vertebral muscle index. The ratio of patients identified with sarcopenia in these studies was similar compared to those using consensus criteria (24–51%). In their study of 450 older trauma patients, Kaplan et al. used the total cross-sectional psoas muscle area at the L3 level and used reference values to define sarcopenia (male < 52.4 cm2/m2; female < 38.6 cm2/m2) [19]. Similarly, among 196 spine patients, Pernik et al. assessed a psoas lumbar vertebral index (cross-sectional area of the psoas muscle on axial CT images at L3 versus area of the L3 vertebra on axial CT images)), based on which patients were divided into quartiles [26]. The patients ranging in the lowest psoas lumbar vertebral index quartile were defined as sarcopenic. Sim et al. used a psoas lumbar vertebral index at the L4 level and assigned patients according to the median to a ‘low’ or ‘high’ group among 615 patients with hip fractures [28]. Wiedl et al. measured the maximum calf circumference and defined 83% of their patients with less than 33 cm calf circumference as sarcopenic [8]. In summary, the heterogeneity of the underlying sarcopenia definitions precludes from a meta-analysis of outcome parameters.
Previous studies have demonstrated a clear association between sarcopenia and prolonged length of hospital stay, particularly in individuals below the age of 65 [43]. Our review indicates a potential trend towards prolonged hospital stays in orthogeriatric patients with sarcopenia. Nevertheless, the clinical relevance of this extension is uncertain, given that only four studies reported statistically significant findings and most of the differences were only marginal. Only Gonzalez-Montalvo et al. found a slightly shorter hospital stay in sarcopenic patients with hip fractures compared to non-sarcopenic patients [13]. However, this study was conducted in a specialized orthogeriatric unit providing a high standard of care including nutrition and physical exercise aimed at reducing length of hospital stay and may therefore not be comparable to studies conducted in other environments.
Non-home discharge may reflect negative outcomes such as declining overall health, which can be caused by conditions like delirium, dementia, or secondary diseases such as pneumonia. In addition, it may be secondary to (surgical) treatment failure, inadequate pain management, and the inability to walk independently. The potential link between institutionalization and sarcopenia in geriatric patients receiving orthopedic and trauma care could not be substantiated in this scoping review as the literature indicated high rates of re-institutionalization to nursing homes, rehabilitation units, and long-term care for both sarcopenic and non-sarcopenic groups (77% and 68%, respectively).However, in the orthogeriatric population specifically, the acute hospitalization may simply reveal an existing inability to live independently for both patients and their families. Therefore, non-home discharge may be seen as a symptom associated with the progression of sarcopenia rather than a direct consequence.
In their systematic review on sarcopenia and its correlation with falls and fractures in older adults, Yeung et al. found a heightened risk of falls in sarcopenic individuals (OR 1.60; 95%CI 1.37–1.86) [39]. While their study encompassed older adults without a lower age limit but with a mean or median age of over 65 years, it did not specifically focus on patient populations undergoing orthopedic or trauma surgeries. In the context of orthopedic and trauma care, patients are often instructed to adhere to postoperative weight-bearing restrictions, sometimes necessitating the use of assistive devices for walking. Despite efforts by orthopedic and trauma surgeons to minimize these restrictions in older patients, they may be unavoidable in certain cases. In addition to factors such as coordination ability, cognitive function, and physical decline, older patients undergoing orthopedic and trauma care may have to significantly higher rates of falls and subsequent fractures compared to non-orthopedic patient populations.
Refracture rates within a time frame of 12 to 36 months following hip fracture have been documented to vary between 6 and 15% [44]. The observed 10% overall refracture rate after hip fractures among sarcopenic older patients in orthopedic and trauma care does not indicate an elevated refracture risk in this population [13]. After percutaneous vertebroplasty of spine fractures, there is a possibility of spinal refractures occurring in up to 52% of patients within a period of 7 years [45]. Chen et al. conducted a multivariate analysis to account for confounding variables and determined that sarcopenia was associated with a significantly increased risk of spinal refracture following kyphoplasty, with a prevalence rate of 84% [12]. They attribute this finding to the reduction in stability and the increase in pressure on the vertebral body as a result of muscle atrophy and degeneration associated with sarcopenia.
Multiple systematic reviews portray sufficient evidence regarding the association of sarcopenia and mortality in orthopedic patients [7, 34, 37]. Our scoping review suggests such a similarly consistent association between sarcopenia and mortality in the orthogeriatric population. The wide range of the published 1-year mortality rates (1–73%) may be secondary to the respective studies’ study populations and sarcopenia assessment criteria. Such heterogeneity precludes from a meta-analysis based on the existing literature.
Using various tools (patient related outcome measurement, PROMs), many studies evaluated the quality of life among their patients. Our review suggests that sarcopenia is associated with a decreased general functional outcome and quality of life compared to non-sarcopenic orthogeriatric populations. However, it is important to note that the heterogeneity of the PROMs used in these studies makes it difficult to determine the exact extent of this association.
Our scoping review reveals that the rates of refractures and subsequent falls have been insufficiently investigated in older patients in orthopedic and trauma care. The possible association of refractures and subsequent falls to sarcopenia can neither be expected nor excluded.
One major drawback of the literature review approach is always the potential for incomplete retrieval of relevant studies. However, this risk is mitigated by the involvement of two independent reviewers who conducted the systematic literature screening. Further limitations of this review’s methodology include language and age restrictions. This may explain some of the low variation regarding the geographic distribution of the included studies. Although we only included studies investigating patients over the age of 65 years, the mean age varied significantly among the different studies. This may be an important confounder regarding some of the results presented in our review. However, by exclusively including patients aged 65 years and above, we ensure a specific focus on the orthogeriatric population. In conclusion, caution should be exercised in all interpretations and deductions due to the heterogeneity of study populations, sarcopenia definitions, injury and disease modalities and localizations, follow-up periods, and outcome assessment tools discussed in this review.
Conclusion
This scoping review found that sarcopenia has been increasingly studied in older patients in orthopedic and trauma care. However, various definitions of sarcopenia were applied not permitting pooling of data in a meta-analytical approach. In summary, there is an ongoing need for an international consensus on a universally accepted definition of sarcopenia. This scoping review suggests that sarcopenia may be linked to greater length of hospital stay, higher rates of non-home discharge, and increased mortality. In specific, prospective studies should be conducted in order to understand the causal relationship between sarcopenia and refractures, falls, and functional outcome/quality of life among older patients in orthopedic and trauma care. Additionally, the establishment of large registers might help to identify patients at increased risk for negative outcomes and contribute to implement preventive measures.
References
Petermann-Rocha F, et al. Global prevalence of sarcopenia and severe sarcopenia: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2022;13(1):86–99.
Shafiee G, et al. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord. 2017;16:21.
Yang J, et al. Bibliometrics Analysis and Visualization of Sarcopenia Associated with Osteoporosis from 2000 to 2022. J Pain Res. 2023;16:821–37.
Studenski SA, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69(5):547–58.
Cruz-Jentoft AJ, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31.
Chen LK, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020;21(3):300-307.e2.
Brzeszczynski F, et al. The effect of sarcopenia on outcomes following orthopaedic surgery : a systematic review. Bone Joint J. 2022;104-b(3):321–30.
Wiedl A, et al. Prognostic value of orthogeriatric assessment parameters on mortality: a 2-year follow-up. Eur J Trauma Emerg Surg. 2022;48(4):2905–14.
Tricco AC, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Stuck AK, et al. Predictive validity of current sarcopenia definitions (EWGSOP2, SDOC, and AWGS2) for clinical outcomes: A scoping review. J Cachexia Sarcopenia Muscle. 2023;14(1):71–83.
Bermejo-Bescós P, et al. Peripheral IL-6 Levels but not Sarcopenia Are Predictive of 1-Year Mortality After Hip Fracture in Older Patients. J Gerontol A Biol Sci Med Sci. 2020;75(10):e130–7.
Chen Q, et al. Relationship between sarcopenia/paravertebral muscles and the incidence of vertebral refractures following percutaneous kyphoplasty: a retrospective study. BMC Musculoskelet Disord. 2022;23(1):879.
González-Montalvo JI, et al. Prevalence of sarcopenia in acute hip fracture patients and its influence on short-term clinical outcome. Geriatr Gerontol Int. 2016;16(9):1021–7.
He Z, et al. Clinical and functional outcomes of total knee arthroplasty in sarcopenia: a case-control retrospective cohort study. J Knee Surg. 2023;36(6):631–6.
Iida H, et al. Sarcopenia affects conservative treatment of osteoporotic vertebral fracture. Osteoporos Sarcopenia. 2018;4(3):114–7.
Iida H, et al. Low muscle mass affect hip fracture treatment outcomes in older individuals: a single-institution case-control study. BMC Musculoskelet Disord. 2021;22(1):259.
Inose H, et al. The impact of sarcopenia on the results of lumbar spinal surgery. Osteoporosis and Sarcopenia. 2018;4(1):33–6.
Jiang S, Ding Y, Kang L. Impact of sarcopenia on intertrochanteric femoral fracture in the elderly. PeerJ. 2022;10:e13445.
Kaplan SJ, et al. Association of Radiologic Indicators of Frailty With 1-Year Mortality in Older Trauma Patients: Opportunistic Screening for Sarcopenia and Osteopenia. JAMA Surg. 2017;152(2):e164604.
Kristensen MT, et al. Knee Extension Strength Measures Indicating Probable Sarcopenia Is Associated with Health-Related Outcomes and a Strong Predictor of 1-Year Mortality in Patients Following Hip Fracture Surgery. Geriatrics (Basel). 2021;6(1):8.
Landi F, et al. The association between sarcopenia and functional outcomes among older patients with hip fracture undergoing in-hospital rehabilitation. Osteoporos Int. 2017;28(5):1569–76.
Liao CD, et al. Impact of Sarcopenia and Obesity on Gait Speed After Total Knee Replacement. J Am Med Dir Assoc. 2022;23(4):631–7.
Lim SK, et al. Functional Outcomes of Fragility Fracture Integrated Rehabilitation Management in Sarcopenic Patients after Hip Fracture Surgery and Predictors of Independent Ambulation. J Nutr Health Aging. 2019;23(10):1034–42.
Malafarina V, et al. Factors Associated with Sarcopenia and 7-Year Mortality in Very Old Patients with Hip Fracture Admitted to Rehabilitation Units: A Pragmatic Study. Nutrients. 2019;11(9):2243.
Ohyama S, et al. Presence of sarcopenia does not affect the clinical results of balloon kyphoplasty for acute osteoporotic vertebral fracture. Sci Rep. 2021;11(1):122.
Pernik MN, et al. Psoas muscle index as a predictor of perioperative outcomes in geriatric patients undergoing spine surgery. Global Spine J. 2023;13(7):2016–24.
Sakai Y, et al. Surgical results in older patients with lumbar spinal stenosis according to gait speed in relation to the diagnosis for sarcopenia. J Orthop Surg (Hong Kong). 2020;28(2):2309499020918422.
Sim JH, et al. Low psoas lumbar vertebral index is associated with mortality after hip fracture surgery in elderly patients: A retrospective analysis. J Personalized Med. 2021;11(7):673.
Steihaug OM, et al. Sarcopenia in patients with hip fracture: A multicenter cross-sectional study. PLoS ONE. 2017;12(9):e0184780.
Steihaug OM, et al. Does sarcopenia predict change in mobility after hip fracture? a multicenter observational study with one-year follow-up. BMC Geriatr. 2018;18(1):65.
Takahashi K, et al. Correlation among sarcopenia, malnutrition and activities of daily living in patients with vertebral compression fractures: a comparison based on admission and discharge parameters evaluating these conditions. J Phys Ther Sci. 2018;30(12):1401–7.
Toyoda H, et al. Impact of Sarcopenia on Clinical Outcomes of Minimally Invasive Lumbar Decompression Surgery. Sci Rep. 2019;9(1):16619.
Longo UG, et al. The Effects of Sarcopenia on Hip and Knee Replacement Surgery: A Systematic Review. Medicina (Kaunas). 2023;59(3):524.
Chiang MH, Kuo YJ, Chen YP. The Association Between Sarcopenia and Postoperative Outcomes Among Older Adults With Hip Fracture: A Systematic Review. J Appl Gerontol. 2021;40(12):1903–13.
Artiaco S, et al. Sarcopenia in distal radius fractures: systematic review of the literature and current findings. Eur J Orthop Surg Traumatol. 2020;30(7):1251–5.
Testa G, et al. Diagnosis, treatment and prevention of sarcopenia in hip fractured patients: Where we are and where we are going: A systematic review. J Clin Med. 2020;9(9):1–13.
Moskven E, et al. The impact of frailty and sarcopenia on postoperative outcomes in adult spine surgery. A systematic review of the literature. Spine J. 2018;18(12):2354–69.
Knoedler S, et al. Impact of sarcopenia on outcomes in surgical patients: a systematic review and meta-analysis. Int J Surg. 2023;109(12):4238–62.
Yeung SSY, et al. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J Cachex Sarcopenia Muscle. 2019;10(3):485–500.
Stuck AK, et al. Comparing Prevalence of Sarcopenia Using Twelve Sarcopenia Definitions in a Large Multinational European Population of Community-Dwelling Older Adults. J Nutr Health Aging. 2023;27(3):205–12.
Kim H, et al. Sarcopenia: Prevalence and associated factors based on different suggested definitions in community-dwelling older adults. Geriatr Gerontol Int. 2016;16(Suppl 1):110–22.
Bischoff-Ferrari HA, et al. Comparative performance of current definitions of sarcopenia against the prospective incidence of falls among community-dwelling seniors age 65 and older. Osteoporos Int. 2015;26(12):2793–802.
Sousa AS, et al. Sarcopenia and length of hospital stay. Eur J Clin Nutr. 2016;70(5):595–601.
Roux C, et al. Refracture and mortality following hospitalization for severe osteoporotic fractures: The Fractos Study. JBMR Plus. 2021;5(7):e10507.
Grados F, et al. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford). 2000;39(12):1410–4.
Funding
Open access funding provided by University of Bern
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Jan Gewiess and Sebastian Kreuzer. The first draft of the manuscript was written by Jan Gewiess and Sebastian Kreuzer. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gewiess, J., Kreuzer, S., Eggimann, A.K. et al. Definitions and adverse outcomes of sarcopenia in older patients in orthopedic and trauma care: A scoping review on current evidence. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02541-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02541-8