Abstract
Purpose
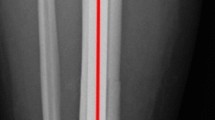
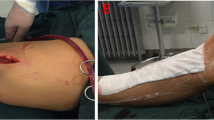
Intramedullary nailing of tibial fractures is one of the most common procedures in orthopedic surgery. It can be technically demanding in proximal or distal fractures, which may be facilitated using semi-extended approaches. The aim of this study is to identify outcomes and their predictors using a semi-extended suprapatellar approach for tibial fracture nailing.
Methods
This is a retrospective cohort of 293 patients who underwent intramedullary nail fixation of a tibial fracture through a suprapatellar approach, considering a postoperative follow-up of 1 year. Data on patient’s baseline characteristics, injuries, treatments, and outcomes regarding alignment, fracture union, and complications were recorded. For multivariable analysis, hierarchical binary (logistic) regression analysis was performed.
Results
The mean patient age was 47.7 years (SD 18.9), with 42A1 the most frequent fracture pattern (n = 98, 33.5%). Correct or anatomical alignment (≤ 5º in both planes) was achieved in 272 (92.8%) of the patients. On multivariate analysis, surgical delay ≥ 7 days (OR = 1.3, 95% CI = 1.3–8.1) and age over 50 years (OR = 3.2, 95% CI = 1.2–8.3) were found as predictors of fracture malalignment. Fracture healing was achieved in 97.6%, and reoperation rate was 6.14%. Overall complication’s predictors were proximal fracture (OR = 2.8, 95% CI = 1.1–7.2), temporary external fixation (OR = 2.4, 95% CI = 1.2–4.9), and fracture malalignment (OR = 2.9, 95% CI = 1.1–7.9).
Conclusion
The suprapatellar approach is a safe and useful technique for treating tibial fractures, leading to no less than correct reduction in almost all patients and achieving a high fracture healing rate, at very low rates of complications. Pre- and postoperative predictors identified must be taken into account to improve outcomes while treating these fractures.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, JVAP, upon reasonable request.
References
Wennergren D, Bergdahl C, Ekelund J, Juto H, Sundfeldt M, Möller M. Epidemiology and incidence of tibia fractures in the Swedish Fracture Register. Injury. 2018;49:2068–74.
Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop. 1995;64–74. https://doi.org/10.1097/00003086-199506000-00008.
Tejwani N, Polonet D, Wolinsky PR. Controversies in the intramedullary nailing of proximal and distal tibia fractures. J Am Acad Orthop Surg. 2014;22:665–73.
Cinats DJ, Perey B, Moola F, Boyer D, Lemke HM, Stone T, et al. Plate-assisted intramedullary nailing of proximal third tibia fractures. J Orthop Trauma. 2020;34:321–6.
Wysocki RW, Kapotas JS, Virkus WW. Intramedullary nailing of proximal and distal one-third tibial shaft fractures with intraoperative two-pin external fixation. J Trauma. 2009;66:1135–9.
Sanders RW, DiPasquale TG, Jordan CJ, Arrington JA, Sagi HC. Semiextended intramedullary nailing of the tibia using a suprapatellar approach: radiographic results and clinical outcomes at a minimum of 12 months follow-up. J Orthop Trauma. 2014;28:245–55.
Tornetta P, Collins E. Semiextended position of intramedullary nailing of the proximal tibia. Clin Orthop. 1996;185–9. https://doi.org/10.1097/00003086-199607000-00029.
Brink O. Suprapatellar nailing of tibial fractures: surgical hints. Curr Orthop Pract. 2016;27:107–12.
Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop. 1995;25–33. https://doi.org/10.1097/00003086-199506000-00004.
Litrenta J, Tornetta P, Mehta S, Jones C, OʼToole RV, Bhandari M, et al. Determination of radiographic healing: an assessment of consistency using RUST and modified RUST in metadiaphyseal fractures. J Orthop Trauma. 2015;29:516–20.
Whelan DB, Bhandari M, Stephen D, Kreder H, McKee MD, Zdero R, et al. Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J Trauma. 2010;68:629–32.
Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. J Bone Joint Surg Am. 2008;90:2567–78. https://doi.org/10.2106/JBJS.G.01694.
Lefaivre KA, Guy P, Chan H, Blachut PA. Long-term follow-up of tibial shaft fractures treated with intramedullary nailing. J Orthop Trauma. 2008;22:525–9.
Maredza M, Petrou S, Dritsaki M, Achten J, Griffin J, Lamb SE, et al. A comparison of the cost-effectiveness of intramedullary nail fixation and locking plate fixation in the treatment of adult patients with an extra-articular fracture of the distal tibia: economic evaluation based on the FixDT trial. Bone Jt J. 2018;100:624–33.
Stinner DJ, Mir H. Techniques for intramedullary nailing of proximal tibia fractures. Orthop Clin North Am. 2014;45:33–45.
Vallier HA. Current evidence: plate versus intramedullary nail for fixation of distal tibia fractures in 2016. J Orthop Trauma. 2016;30(Suppl 4):S2-6.
Behlmer RJ, Whiting PS, Kliethermes SA, Wendt L, Simske NM, Sato EH, et al. Reduction techniques for intramedullary nailing of tibial shaft fractures: a comparative study. OTA Int Open Access J Orthop Trauma. 2021;4: e095.
Natoli RM, Sardesai NR, Richard RD, Sorkin AT, Gaski GE, Virkus WW. Intramedullary nailing of lower-extremity periarticular fractures. JBJS Essent Surg Tech. 2019;9(e35):1–2.
Wang C, Chen E, Ye C, Pan Z. Suprapatellar versus infrapatellar approach for tibia intramedullary nailing: a meta-analysis. Int J Surg Lond Engl. 2018;51:133–9.
Franke J, Hohendorff B, Alt V, Thormann U, Schnettler R. Suprapatellar nailing of tibial fractures-indications and technique. Injury. 2016;47:495–501.
Metcalf KB, Du JY, Lapite IO, Wetzel RJ, Sontich JK, Dachenhaus ER, et al. Comparison of infrapatellar and suprapatellar approaches for intramedullary nail fixation of tibia fractures. J Orthop Trauma. 2021;35:e45-50.
Jones M, Parry M, Whitehouse M, Mitchell S. Radiologic outcome and patient-reported function after intramedullary nailing: a comparison of the retropatellar and infrapatellar approach. J Orthop Trauma. 2014;28:256–62.
De Giacomo AF, Tornetta P. Alignment after intramedullary nailing of distal tibia fractures without fibula fixation. J Orthop Trauma. 2016;30:561–7.
Avilucea FR, Triantafillou K, Whiting PS, Perez EA, Mir HR. Suprapatellar intramedullary nail technique lowers rate of malalignment of distal tibia fractures. J Orthop Trauma. 2016;30:557–60.
Kulkarni MS, Tummala M, Aroor MN, Vijayan S, Rao SK. Suprapatellar nailing in proximal third tibial fractures - clinicoradiological outcome. Injury. 2020;51:1879–86.
Vidyadhara S, Sharath KR. Prospective study of the clinico-radiological outcome of interlocked nailing in proximal third tibial shaft fractures. Injury. 2006;37:536–42.
Auston DA, Meiss J, Serrano R, Sellers T, Carlson G, Hoggard T, et al. Percutaneous or open reduction of closed tibial shaft fractures during intramedullary nailing does not increase wound complications, infection or nonunion rates. J Orthop Trauma. 2017;31:215–9.
Nork SE, Barei DP, Schildhauer TA, Agel J, Holt SK, Schrick JL, et al. Intramedullary nailing of proximal quarter tibial fractures. J Orthop Trauma. 2006;20:523–8.
Schemitsch EH, Bhandari M, Guyatt G, Sanders DW, Swiontkowski M, Tornetta P, et al. Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Joint Surg Am. 2012;94:1786–93.
Bhandari M, Adili A, Leone J, Lachowski RJ, Kwok DC. Early versus delayed operative management of closed tibial fractures. Clin Orthop. 1999;230–9. https://doi.org/10.1097/00003086-199911000-00028.
Bhandari M, Guyatt GH, Tong D, Adili A, Shaughnessy SG. Reamed versus nonreamed intramedullary nailing of lower extremity long bone fractures: a systematic overview and meta-analysis. J Orthop Trauma. 2000;14:2–9.
Duan X, Al-Qwbani M, Zeng Y, Zhang W, Xiang Z. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev. 2012;1:CD008241.
Bhandari M, Tornetta P, Sprague S, Najibi S, Petrisor B, Griffith L, et al. Predictors of reoperation following operative management of fractures of the tibial shaft. J Orthop Trauma. 2003;17:353–61.
Milner SA, Davis TRC, Muir KR, Greenwood DC, Doherty M. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Joint Surg Am. 2002;84:971–80.
Mitchell PM, Weisenthal BM, Collinge CA. No incidence of postoperative knee sepsis with suprapatellar nailing of open tibia fractures. J Orthop Trauma. 2017;31:85–9.
Marecek GS, Nicholson LT, Broghammer FH, Talerico M, Tougas C, Donegan DJ, et al. Risk of knee sepsis after treatment of open tibia fractures: a multicenter comparison of suprapatellar and infrapatellar approaches. J Orthop Trauma. 2018;32:88–92.
Courtney PM, Boniello A, Donegan D, Ahn J, Mehta S. Functional knee outcomes in infrapatellar and suprapatellar tibial nailing: does approach matter? Am J Orthop Belle Mead NJ. 2015;44:E513-516.
Toivanen JAK, Väistö O, Kannus P, Latvala K, Honkonen SE, Järvinen MJ. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft. A prospective, randomized study comparing two different nail-insertion techniques. J Bone Joint Surg Am. 2002;84:580–5.
Isaac M, OʼToole RV, Udogwu U, Connelly D, Baker M, Lebrun CT, et al. Incidence of knee pain beyond 1 year: suprapatellar versus infrapatellar approach for intramedullary nailing of the tibia. J Orthop Trauma. 2019;33:438–42.
Packer TW, Naqvi AZ, Edwards TC. Intramedullary tibial nailing using infrapatellar and suprapatellar approaches: a systematic review and meta-analysis. Injury. 2020 https://doi.org/10.1016/j.injury.2020.09.047.
Funding
This study was funded by Smith & Nephew.
Author information
Authors and Affiliations
Contributions
Material preparation, data collection, and analysis were performed by JVAP, YGS, MCGM, CCR, and EGA. The first draft of the manuscript was written by JTS, JVAP, and YGS, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by our institutional review board (reference number (PR(ATR)100/2019).
Consent to participate and for publication
This is a retrospective study. Its realization did not imply any risk for the participants, and all the collected data were de-identified. Therefore, IRB approved a full waiver of informed consent.
Competing interests
The authors have financial conflicts of interest to declare with Smith & Nephew, Zimmer-Biomet, Link Orthopaedics, Stryker, and MBA Surgical Empowerment.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Teixidor-Serra, J., Andrés-Peiró, J.V., García-Sanchez, Y. et al. Outcomes and their predictors in suprapatellar nailing for tibia fractures. Multivariable analysis of 293 consecutive cases. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02476-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02476-0